Release form
Available in the form of flat, round, white tablets.
Active ingredient: acetazolamide – 250 mg.
Inactive ingredients: potato starch, talc, sodium glycolate.
Diacarb is produced (under the international name Diacarb) in tablet form by the manufacturer Polpharma. Each tablet has a round shape. The package contains 30 tablets and official instructions in Russian.
Diacarb is produced in the form of round, flat, white tablets. Each tablet contains 250 mg of the active substance - acetazolamide, and excipients - talc, potato starch, sodium starch glycolate. 12 pieces in a blister, 2 packs in a cardboard box.
Tablets, 250 mg. 10 tablets each in blister packs made of PVC film and aluminum foil. 3 blister packs are placed in a cardboard pack.
Diacarb price, where to buy
Diakarb tablets have a fairly affordable price. They can be found in many pharmacies. The price of Diakarb is approximately 210 rubles. This product is also sold in Ukraine. The price of Diacarb in 250 mg tablets (30 pieces per package) averages 140 hryvnia.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
- Online pharmacies in KazakhstanKazakhstan
ZdravCity
- Diacarb tablets 250 mg 30 pcs. JSC AKRIKHIN
250 rub. order
Pharmacy Dialogue
- Diacarb tablets 250 mg No. 30Polfarma
RUB 254 order
show more
Pharmacy24
- Diacarb 250 mg N30 tablets Pharmaceutical plant "POLFARMA" S.A., Poland/Medana Pharma Aktsionerne Tovaristvo, Poland
261 UAH.order
PaniPharmacy
- Diacarb tablets Diacarb tablets. 250 mg No. 30 Poland, Polpharma
246 UAH order
show more
Contraindications
The instructions indicate the following range of contraindications to the use of Diakarb:
- Hypersensitivity to one or more components of the drug. Acidosis.
- Chronic adrenal insufficiency (Addison's disease).
- Insufficient secretion of cortisol and aldosterone by the adrenal glands.
- Diabetes mellitus (risk of hyperglycemia).
- Intoxication of the body with products of protein metabolism.
- Hypokalemia (potassium deficiency in the blood).
- Hyponatremia (sodium deficiency).
- Acute liver disorders.
The use of Diacarb is contraindicated in:
- Diabetes mellitus;
- Acute renal and liver failure;
- Hypersensitivity to the active substance;
- Hypokalemia;
- Acidosis;
- Hypocorticism;
- Uremia;
- Addison's disease.
The drug is prescribed with caution for edema of hepatic and renal origin and when taken together with sacetylsalicylic acid (in high doses).
Diacarb is contraindicated for use during pregnancy and lactation.
- allergy to a drug;
- kidney pathologies;
- liver diseases, including cirrhosis;
- kidney failure in acute and severe forms;
- urolithiasis, in which stones form from calcium salts;
- decreased levels of K and Na in the blood;
- angle-closure glaucoma in chronic forms. Diacarb is not used for long-term treatment;
- pregnancy;
- diabetes mellitus of any type;
- children. Diacarb is prescribed from three years of age only for the treatment of epilepsy. The drug is not prescribed to infants, newborns and children under one to three years of age, even for the treatment of epilepsy;
- insufficiency of adrenal glands;
- Addison's disease;
Before prescribing the drug, the doctor will definitely exclude these disorders in patients.
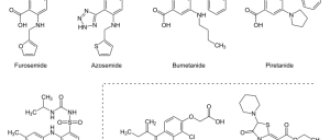
Furosemide
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day...
Read more "
Furosemide is a potent diuretic. It is taken to reduce edema caused by heart or kidney failure, liver cirrhosis, and other causes. This medicine is also sometimes prescribed for high blood pressure. Below you will find instructions for use written in clear language. Study the indications, contraindications and side effects. Find out how to take furosemide: how many times a day, in what dosage, before or after meals, for how many days in a row. The article describes in detail how to be treated with furosemide for edema and high blood pressure. Find out which is better: furosemide or torasemide, why furosemide is sometimes prescribed together with the drugs Veroshpiron and Diacarb. Read what side effects are caused by taking furosemide for weight loss, and whether this drug is compatible with alcohol.
Instructions for use
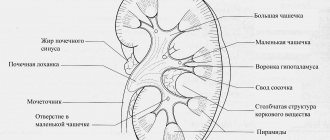
| pharmachologic effect | Furosemide stimulates the kidneys to excrete more fluid and salt in the urine. This is called a diuretic (diuretic) and natriuretic effect. Thanks to it, swelling in patients decreases. Unfortunately, along with excess water and salt, the body also loses valuable electrolytes - potassium and magnesium. This may cause side effects, which are detailed below. The diuretic effect of furosemide is pronounced, and the larger the dose of medication the patient takes, the stronger it is. The kidneys are made up of filtering elements called nephrons. Furosemide acts on a part of the nephron called the loop of Henle. Therefore, it is classified as a loop diuretic. It is more powerful than thiazide and thiazide-like diuretics - Hypothiazide and Indapamide (Arifon). |
| Pharmacokinetics | After taking a furosemide tablet, the diuretic effect begins within 60 minutes. The injection of this medicine begins to act within 5 minutes. Each dose of furosemide lasts 3-6 hours. The diuretic effect wears off quickly and is considered a disadvantage compared to the newer diuretic drug torasemide (Diuver). Furosemide and its metabolites are excreted 88% by the kidneys and 12% by the liver, with bile. The more severe the kidney or liver failure, the slower furosemide is eliminated from the body and the higher the risk of side effects. Also, the excretion of furosemide slows down in patients with heart failure due to weakened renal function. |
| Indications for use | Furosemide can be prescribed for edema caused by heart and kidney failure, and liver diseases. Arterial hypertension is also included in the list of indications for use. Sometimes people voluntarily take furosemide for edema and for weight loss. This is discussed in detail below. Diuver (torasemide) is a medication that replaces furosemide in the treatment of heart failure. Torsemide acts more smoothly and causes less side effects. For hypertension, competent doctors try not to prescribe furosemide for daily use due to frequent side effects. It is sometimes used to provide emergency care during a hypertensive crisis. Furosemide remains a popular treatment for ascites caused by cirrhosis of the liver. It is prescribed together with spironolactone; read the article “Veroshpiron” for more details. |
| Contraindications | Kidney disease in which urine production stops. Allergy to furosemide, sulfonamides or sulfonylurea diabetes medications. Significant deficiency of potassium or sodium in the body. Dehydration. Acute glomerulonephritis. Decompensated mitral or aortic stenosis. Severe liver failure, threat of hepatic coma. Furosemide can harm patients who have high levels of uric acid in the blood or gout, impaired glucose tolerance or diabetes, low blood pressure, acute heart attack, pancreatitis, impaired urinary flow, systemic lupus erythematosus, diarrhea (diarrhea). |
| special instructions | Furosemide can cause weakness and fatigue, which increases the risk of getting into an accident. Refrain from driving vehicles and dangerous machinery for at least the first 5-7 days, until the body gets used to the new medicine. It may make sense to take Asparkam, Panangin tablets or salt substitutes rich in potassium along with a diuretic drug. Discuss this with your doctor and do not take potassium supplements on your own. Also discuss with your doctor how much and what kind of liquid you can drink. Be wary of gastrointestinal illnesses that involve vomiting or diarrhea because they can cause dehydration, a dangerous deficiency of potassium and magnesium in the body. Try not to overheat in the sun; it is not advisable to visit a solarium. |
| Dosage | The doctor selects the dosage of the drug furosemide individually, depending on the indications for use, the severity of the disease, the patient’s age and other factors. Adults take furosemide tablets 20-80 mg once or several times a day. Intravenous or intramuscular injections - 20-240 mg. Sometimes higher doses than those indicated above are prescribed. The initial dose of furosemide for children is 1-2 mg per 1 kg of body weight. Maximum - up to 6 mg per 1 kg of body weight. The initial dosage of the diuretic medication is often increased or decreased later. This depends on whether urine formation has increased, the dynamics of the patient’s condition and test results. |
| Side effects | Furosemide often causes unpleasant and even dangerous side effects. Therefore, it should not be taken for self-medication. Symptoms of dehydration, potassium and magnesium deficiency include muscle cramps, weakness, confusion, drowsiness, dizziness, fainting, dry mouth, thirst, nausea, vomiting, fast or irregular heartbeat, unusual decrease in urine output. If you are concerned about serious side effects, consult your doctor immediately. To reduce dizziness, stand up smoothly rather than abruptly from a sitting or lying position. An allergy to furosemide may cause skin rash, itching, and difficulty breathing. Older age and kidney and liver disease are factors that increase the risk of side effects. |
| Pregnancy and breastfeeding | Furosemide crosses the placental barrier and affects the fetus. During pregnancy, it is occasionally prescribed only for severe illnesses, usually threatening the life of the mother. At the same time, carefully monitor the condition of the fetus. Do not take furosemide during pregnancy without permission! Studies on laboratory animals have shown that furosemide in high doses has a negative effect on pregnancy. No studies have been conducted on humans. Furosemide should not be taken while breastfeeding. This medicine passes into breast milk and may affect the baby. It also suppresses the production of breast milk in the mother's body. |
| Interaction with other drugs | Furosemide interacts negatively with many other medications. Because of this, patients often experience dangerous side effects. To reduce your risk, tell your doctor about all the medications, herbs, and dietary supplements you use before you are prescribed furosemide. Use caution when taking this diuretic medication with hormone medications, antibiotics, nonsteroidal anti-inflammatory drugs (NSAIDs), constipation medications, insulin, and diabetes pills. Furosemide enhances the effect of high blood pressure pills, which can cause hypotension, dizziness, and even fainting. The list of furosemide drug interactions given above is not complete. Discuss the details with your doctor without hiding any of the medications you take. |
| Overdose | An overdose of the drug furosemide causes the symptoms listed above in the “Side Effects” section. Significantly low blood pressure, a state of shock, delirium or apathy, and manifestations of blockage of blood vessels by blood clots may also be observed. It is likely that urine output will stop due to dehydration. Treatment is carried out in the hospital in the intensive care unit. Before emergency help arrives, it is recommended to pour a lot of liquid into the patient’s stomach, then induce vomiting, and give activated charcoal. Next, doctors will take measures to eliminate dehydration and acid-base balance disorders. To replenish the loss of fluid and electrolytes, droppers with saline, potassium and magnesium are used. For hypotension - dopamine or norepinephrine. Treatment is stopped when symptoms of overdose cease to be observed for 6 consecutive hours. |
- Lasix
- Veroshpiron
- Asparkam
- Hypothiazide
How to take furosemide
Take furosemide as prescribed by your doctor. He must select the dosage and indicate how many times a day this medicine should be taken. As a rule, for edema caused by various reasons, a diuretic should be taken 1 or 2 times a day. For daily treatment of hypertension, this drug is prescribed to be taken 2 times a day. Read more about the use of furosemide for hypertension and edema below.
Many patients are interested in how many days in a row they can take furosemide. This should only be decided by the attending physician. Do not prescribe or discontinue diuretic medications on your own initiative. Many people, especially women, more or less often take furosemide for edema, instead of trying to eliminate their causes. You can easily find on Russian-language websites frightening descriptions of severe side effects that lead to self-medication with diuretics for edema.
The official instructions for use do not indicate whether furosemide should be taken before or after meals. An English-language article states that taking furosemide after meals significantly reduces its effectiveness. As a rule, doctors prescribe taking this medicine on an empty stomach, at least 20-30 minutes before meals. Perhaps, for some reason, your doctor will prescribe you to take Furosemide after meals. In this case, follow his instructions.
Frequently asked questions and their answers
Below are answers to questions that patients often have about the use of the diuretic drug furosemide.
Is it possible to drink furosemide every day?
Furosemide is taken every day as prescribed by a doctor for people whose liver cirrhosis is complicated by ascites - an accumulation of fluid in the abdominal cavity. Previously, this daily medication was prescribed to patients with heart failure and hypertension. Now the new drug torasemide (Diuver) is replacing furosemide in the treatment of heart failure. Why torasemide is better is described in detail below. If you take furosemide every day for heart failure, discuss with your doctor whether it should be replaced with torasemide.
If you have hypertension, it is better not to take furosemide daily, like any other loop diuretics. These medications cause too many side effects. Use blood pressure pills that act more gently. Consult your doctor to find a medication regimen that will bring your hypertension under control without worsening your health and test results. Some people take furosemide occasionally when they have a hypertensive crisis. It is better instead to properly treat hypertension so that there are no pressure surges at all. Do not take furosemide daily for weight loss or swelling! This can cause terrible side effects. They are vividly described on many websites and forums in Russian.
Can I take this medicine at night?
As a rule, doctors prescribe taking furosemide in the morning or afternoon, and not at night, so that the patient does not have to get up to go to the toilet too often at night. For some reason, your doctor may tell you to take furosemide at night. In this case, follow his instructions. Many people have voluntarily tried taking this diuretic medicine at night to avoid swelling and look good the next morning. Russian-language sites and forums are replete with terrible descriptions of the side effects that such self-medication leads to. The authors of numerous frightening stories about the side effects of furosemide are not exaggerating at all.
Are furosemide and alcohol compatible?
Alcohol increases the frequency and severity of furosemide side effects. If you use a diuretic drug and alcohol at the same time, your blood pressure may drop too low. Symptoms of this: headache, dizziness, fainting, palpitations. Furosemide often causes orthostatic hypotension - dizziness when standing up suddenly from a sitting or lying position. Alcohol may increase this side effect. Alcohol dehydrates the body and removes beneficial minerals, just like diuretics. Furosemide should be taken only for severe illnesses in which alcohol consumption is completely prohibited. Even a small dose of alcohol will be harmful to you. For mild illnesses that allow moderate alcohol consumption, try to replace the loop diuretic with a more gentle drug or avoid taking medications altogether.
How to take furosemide and Asparkam together?
Take furosemide and Asparkam together only as prescribed by your doctor, and have regular blood tests to check your potassium levels. Furosemide deprives the body of a valuable electrolyte - potassium. Asparkam and Panangin tablets replenish potassium reserves. Discuss with your doctor whether you need to take furosemide and Asparkam at the same time. Don't do this on your own initiative. Asparkam has contraindications. Please read them before using this product. Take both medications in the dosages prescribed by your doctor, as many times a day as your doctor prescribes.
Why do you feed pharmacies if hypertension is afraid of the usual like fire...
Tabakov has revealed a unique remedy against hypertension! To reduce blood pressure while preserving blood vessels, add to…
Why doesn't furosemide work? The patient's swelling does not decrease.
Furosemide is only a temporary solution to the problem of edema. It does not affect their cause, and sometimes even worsens it. If the cause cannot be eliminated, then over time even potent diuretics stop working. Perhaps the patient's kidneys have become so bad that the body has stopped responding to the diuretic medicine. In such situations, you cannot voluntarily increase the dose of furosemide or change it to another diuretic. Talk to your doctor about what to do.
How to restore kidney function after treatment with furosemide?
To find out how furosemide affected the kidneys, ask about the glomerular filtration rate (creatinine clearance), and then take a blood test for creatinine. Learn and follow the rules for preparing for this test to ensure accurate results. Creatinine clearance is the main indicator by which you can judge whether a person's kidneys are working well.
It is rare that unauthorized use of one or more furosemide tablets will cause permanent kidney damage. Most likely, your health and kidney function will return to normal soon after you stop taking the diuretic medication. If you have experienced unpleasant side effects, this will serve as a lesson: you should not take strong drugs on your own initiative.
Unfortunately, for people who develop kidney failure, there is no easy solution to the problem. Furosemide damages the kidneys. But if the swelling is so severe that it is impossible to tolerate it, then you have to use this remedy, despite the side effects. Follow your doctor's diet and medication instructions to delay the point at which your kidneys fail completely. There is no effective alternative treatment for kidney failure. Diabetes patients should study the article “Diet for kidneys in diabetes”.
Torsemide or furosemide: which is better?
Torsemide is better than furosemide for the treatment of heart failure. Both of these medications are loop diuretics. Torsemide was invented 20 years later than furosemide, in 1988. In Russian-speaking countries, the first drug torasemide was registered in 2006.
Furosemide
Torasemide
| Poor absorption when taken with food | Yes | No |
| Excretion from the body | 50/50 kidneys and liver | 80% - liver, 20% - kidneys |
| Potassium deficiency in the body in patients | Often | Rarely |
Torsemide acts more gradually and longer than furosemide and is considered a safer drug. A possible side effect of loop diuretics is a decrease in potassium levels in the blood of patients. Torsemide causes it less frequently. Sometimes torasemide is prescribed to patients in the later stages of renal failure, when furosemide can no longer be taken. After the dose of furosemide has worn off, urinary salt excretion may be significantly reduced due to the rebound effect. Torsemide does not have this problem.
If you are taking furosemide for heart failure edema, talk to your doctor about changing it to torasemide (Diuver). Authors of articles in medical journals claim that in patients with hypertension, torasemide does not affect blood sugar and uric acid levels, unlike furosemide. Don't trust this information too much. People with high blood pressure may benefit from taking safer medications daily than the loop diuretics furosemide and torsemide.
- Diuver
- Britomar
- Trigrim
Torsemide appears to be as good as furosemide for treating fluid accumulation in the abdomen (ascites) caused by cirrhosis of the liver. See, for example, the article “Torasemide versus furosemide in cirrhosis: a long-term, double-blind, randomized clinical study” by Fiaccadori F., Pedretti G., Pasetti G. et al in the journal “The Clinical Investigator” for 1993. However, furosemide is still prescribed many times more often than torasemide for severe liver diseases. Typically, with liver cirrhosis, patients take a loop diuretic and Veroshpiron (spironolactone) simultaneously.
Furosemide or Veroshpiron: which is better? Can it be taken together?
Many patients are interested in which medicine is better: furosemide or Veroshpiron? You can’t pose the question like that, because these are completely different medicines. They are prescribed for different purposes. Therefore, it cannot be said that furosemide is better than Veroshpiron, or vice versa. Sometimes patients have to take both of these drugs at the same time. Furosemide is a powerful diuretic medicine that belongs to the loop diuretics. It stimulates the removal of fluid and salt from the body. Its effect is quick and strong, although not long lasting. While the patient's kidneys can still respond to diuretics, this medicine is good for edema. Veroshpiron has a weak diuretic effect. But it improves the results of treatment with furosemide and reduces the risk of a side effect - potassium deficiency in the body.
The drug Diuver (torasemide) and its analogues have replaced furosemide in the treatment of heart failure. Because torasemide works better and causes fewer side effects. However, furosemide remains a popular treatment for ascites (a build-up of fluid in the abdomen) caused by cirrhosis of the liver. For severe liver diseases, patients are often prescribed furosemide and Veroshpiron together. Usually they start with a dosage of 100 mg of Veroshpiron and 40 mg of furosemide per day. If this dosage does not help enough, it is increased after 3-5 days. At the same time, the ratio of Veroshpiron and furosemide is maintained at 100:40 to maintain optimal potassium levels in the blood.
Furosemide for high blood pressure
Patients should avoid the use of furosemide with high blood pressure, except in the most severe cases. This medicine causes serious side effects if taken daily to treat hypertension. It removes potassium and magnesium from the body, which negatively affects the well-being of patients. Furosemide also accelerates the development of diabetes and gout. If a patient with hypertension already suffers from diabetes or gout, then taking a strong diuretic medication will worsen his condition.
For high blood pressure, furosemide is prescribed for daily use to seriously ill patients who are no longer helped by thiazide and thiazide-like diuretics - Hypothiazide, Indapamide and their analogues. During hypertensive crises, this medicine can be taken occasionally, but only as prescribed by a doctor. Study the article “Hypertensive crisis: emergency care“. Furosemide and other diuretics are not the best choice when you need to quickly stop a hypertensive crisis. Use less harmful medications for this. Talk to your doctor about which blood pressure pills you should take every day. The doctor will likely prescribe combination medications that contain diuretic components, but not powerful loop diuretics.
- The best way to cure hypertension (quickly, easily, healthy, without “chemical” drugs and dietary supplements)
- Hypertension is a popular way to cure it at stages 1 and 2
- Causes of hypertension and how to eliminate them. Tests for hypertension
- Effective treatment of hypertension without drugs
Furosemide for edema
Furosemide helps with edema because it stimulates the kidneys to remove salt and fluid from the body. Unfortunately, this medicine does not eliminate the causes of edema, and sometimes even worsens them. As a rule, edema is caused by heart failure, kidney or liver disease, and also problems with blood vessels in the legs. It is necessary to take measures to eliminate the cause of edema, and not just muffle their symptoms with furosemide. Unauthorizedly taking diuretics for edema, you can get yourself into trouble. Furosemide is a powerful medicine that causes serious side effects. There is a possibility that it will permanently damage the kidneys.
If you regularly experience swelling, do not ignore it, but consult a doctor as soon as possible. Get a medical examination to determine the cause. The diseases listed above respond well to treatment in the early stages. Potent diuretic drugs are prescribed as symptomatic treatment in severe cases, when time has been lost and the underlying disease can no longer be affected. Furosemide for edema sometimes helps even patients for whom it is no longer useful to take thiazide diuretics (Hypothiazide and its analogues).
Furosemide for weight loss
Taking furosemide for weight loss is a bad idea. You will be able to lose no more than 2-3 kg, but at the same time you will cause significant harm to your health. Furosemide reduces the amount of water in the body, but does not promote fat burning. Excess weight is not an indication for the use of this drug. No doctor or nutritionist in their right mind would approve the use of strong diuretic drugs for weight loss. Because side effects are common and severe.
Weight loss when taking furosemide occurs because this medicine quickly causes dehydration. A lack of water in the body leads to diseases of the joints and internal organs. They develop over time. Dehydration also worsens the appearance of women's skin, and this becomes immediately noticeable. In addition to water, furosemide removes valuable minerals from the body - potassium and magnesium. Deficiency of electrolytes will worsen your well-being and attractiveness. Do not use strong diuretics for weight loss. Pay attention to metformin (Siofor, Glucophage). This is a very safe drug that allows you to reduce fat deposits.
- Treatment of hypertension in older people
Pharmacology
Diacarb has a mild diuretic effect. Suppresses the enzyme carbonic anhydrase in the proximal convoluted tubule of the nephron, increasing the excretion of the body's main electrolytes in urine, and has no effect on the excretion of chlorine ions. Helps increase the balance of alkalis and acids in the urine. By inhibiting carbonic anhydrase of the ciliary body, the formation of aqueous humor is reduced, helping to lower eye pressure.
Duration of action is up to 12 hours.
Instructions for use Diacarb
Diacarb is used regardless of food only internally. The recommended starting dosage for adult patients is 250 mg.
Dosage regimens for adults for edema
The diuretic Diacarb is used only in adults in doses of 250 to 375 mg in the morning (before lunch). The diuretic effect appears more often on the second day of administration. For this pathology, Diacarb is used in combination with other drugs intended for the complex treatment of heart diseases. The duration of the appointment is selected by the doctor individually.
Course of treatment for epilepsy
Recommended daily dosages are from 250 to 1000 mg of Diacarb. The average therapeutic dose is from 8 to 30 mg per kilogram of body weight. The total dose is divided into 1-4 applications (morning, afternoon, evening).
Dosage regimen for glaucoma
For exacerbation of angle-closure forms: 1 tablet four times a day.
Open-angle glaucoma: 1 tablet 1 to 4 times a day. Increasing the daily dose to more than 1000 mg will not increase the effects of the drug.
Secondary forms of glaucoma: one tablet every four hours. Long-term use of the medication is not recommended.
Use for the treatment and prevention of mountain sickness
Daily dosages – from 500 to 1000 mg of the drug. It is recommended to divide it into several applications.
According to the instructions, Diacarb is prescribed to adults in the following doses:
- For edema syndrome - in the morning, 1 time per day at a dose of 250-375 mg. The best effect is achieved with the following regimen: taken every other day or two days in a row with a one-day break. When using Diakarb, therapy for circulatory failure, including cardiac glycosides and a low-salt diet, should not be canceled;
- For open-angle glaucoma, 250 mg is prescribed 1-4 times a day. It should be borne in mind that increasing the dose to more than 1 g does not increase the therapeutic effect;
- For acute attacks of glaucoma, the drug is prescribed 250 mg 6 times a day at equal intervals;
- For secondary glaucoma, the drug is prescribed in the same dose, only every 4 hours. Sometimes the therapeutic effect appears after short-term administration of the drug 250 mg 2 times a day;
- For epilepsy, 250-500 mg per day is prescribed once for 3 days, and on the fourth day a break is taken;
- For mountain sickness, an increased dose is prescribed - 500-1000 mg per day; and in cases of rapid ascent - 1000 mg per day, divided in equal doses into several doses. The drug should be used before climbing, 24-48 hours before. If symptoms of the disease appear, you need to continue treatment for the next two days or, if necessary, more.
If you accidentally miss a dose of Diacarb, you should not increase the dose at the next dose.
For children with epilepsy, according to the instructions, Diacarb is prescribed in the following doses:
- From 4 to 12 months – 50 mg per day, divided into two doses;
- From 2 to 3 years – 50-125 mg per day, also dividing the dose into two doses;
- From 4 to 18 years – 125-250 mg per day once, preferably in the morning.
If other anticonvulsants are used simultaneously with Diacarb, then at the beginning of treatment only one tablet is used, and if necessary, the dose can be gradually increased, but do not use more than 750 mg per day.
For children with attacks of glaucoma, the daily dose is calculated at 10-15 mg per kg of body weight, and divided into 3-4 doses in equal parts.
Children under one year of age are often prescribed Diacarb and Asparkam as part of complex therapy for the treatment of increased intracranial pressure and hydrocephalus. The dosage is calculated by a neurologist individually depending on age and condition, most often in a course of three days every other three days. The medications are taken in the morning. Diacarb and Asparkam in this case act as complementary drugs. Potassium destroyed by the action of Diacarb is replenished with Asparkam.
Pharmacological properties of the drug Diacarb
Pharmacodynamics. Acetazolamide is a potent carbonic anhydrase inhibitor and has a weak diuretic effect. The mechanism of action is based on inhibition of the release of sodium and hydrogen ions from carbonic acid. Carbonic anhydrase catalyzes the reaction that produces carbonic acid. Inhibition of this enzyme by acetazolamide leads to inhibition of carbonic acid synthesis in the proximal tubules. The deficiency of carbonic acid as a source of hydrogen ions increases the excretion of water and sodium. The effect of acetazolamide is due to increased natriuresis and diuresis. Acetazolamide loses its diuretic properties after 3 days of use. A short break in use leads to restoration of the diuretic effect of acetazolamide, since carbonic anhydrase activity is resumed. Acetazolamide increases not only the excretion of sodium, but also bicarbonate, which can cause metabolic acidosis. Excretion of a significant amount of sodium due to acetazolamide leads to increased excretion of water with loss of potassium and the development of hypokalemia. Acetazolamide also increases the excretion of phosphate, magnesium and calcium in the urine, which can lead to corresponding metabolic disorders. The extrarenal effect of acetazolamide is used in the treatment of glaucoma. Acetazolamide reduces the amount of fluid in the eye, lowering intraocular pressure. Inhibition of carbonic anhydrase in the central nervous system inhibits abnormal neuronal transmission, as a result of which the drug is also used in the complex treatment of epilepsy. Pharmacokinetics. Acetazolamide is well absorbed from the gastrointestinal tract. After oral administration at a dose of 500 mg, the maximum concentration (12–27 mcg/ml) is achieved after 1–3 hours. A low concentration of acetazolamide is maintained in the blood for 24 hours. Distribution. Acetazolamide is widely distributed in the body. Penetrates into red blood cells, blood plasma, kidneys and in significant quantities into the liver, muscles, eyes and central nervous system. The drug does not accumulate in tissues. Metabolism. Acetazolamide is not metabolized. Elimination. The drug is excreted unchanged by the kidneys. After oral administration, about 90% of the dose taken is excreted in the urine within 24 hours.
Pharmacokinetics
Oral administration of the drug ensures immediate absorption from the gastrointestinal tract. After which the maximum concentration of acetazolamide in the blood is observed after 2-3 hours. The active ingredient Diacarb enters the bloodstream, red blood cells, kidneys, a small amount of it ends up in muscle tissue, liver parenchyma, central nervous system, eyes. Does not accumulate in tissues.
In unchanged form, 90% of the drug is excreted by the kidneys through the urinary tract per day.
Therapeutic effect of the drug Diacarb
Diacarb is a universal remedy and has a complex effect on the human body due to the active substance and additives.
The drug has the following therapeutic effects, such as:
- Diuretic action.
- Antiepileptic effect.
- Antiglaucoma effect.
- Reduced intracranial pressure.
Let's analyze this set of actions in more detail.
Diacarb as a diuretic is rather ineffective, but effective and noticeable. An increase in the excretion of fluid from the body leads to a greater loss of potassium from the cells, so it is advisable to simultaneously take drugs such as Panagin, Aspanagin or Asparkam. This will help avoid hypokalemia (a condition in the body when the potassium level in the blood is below normal).
Using the same principle, phosphorus, calcium and magnesium are removed from the patient’s body, but in much smaller volumes. If you take Diakarb for more than two weeks, you should additionally take medications containing the above microelements.
In addition, the drug itself has a diuretic effect within a three-day period. After this period, subject to continuous use, Diacarb loses its diuretic properties. Therefore, doses should be taken at intervals of one to three days.
Antiglaucoma effect. Diacarb reduces the amount of fluid produced in the anterior chamber of the eyeball, which helps reduce intraocular pressure. This should also include a similar effect on the central nervous system, which helps to lower intracranial pressure.
Antiepileptic effect. Diacarb blocks areas of the brain responsible for pathological excitability. This effect reduces the likelihood of an attack in patients taking the drug.
Overdose
- imbalance of electrolytes in the body;
- muscle spasms;
- drowsiness;
- decreased urine output.
When taking high doses, it is recommended to rinse the stomach, and if the patient’s condition is serious, discontinue the drug.
No data on pharmaceutical overdose have been recorded. Signs of adverse reactions may increase. Therapy is aimed at eliminating manifestations and normalizing the patient’s condition. There is no antidote for the pharmaceutical drug Diacarb. If acidosis occurs, bicarbonates are indicated. To remove acetazolamide from the body, hemodialysis is recommended.
Side effects
- nausea;
- decreased or complete lack of appetite;
- allergy;
- thirst;
- anemia;
- erythema;
- increased sensitivity to light;
- decreased sex drive;
- reversible myopia;
- bile stagnation;
- hepatic colic;
- death of liver tissue (extremely rare);
- general weakness;
- attacks of headache;
- attention disorders;
- dizziness;
- feeling of hair on the surface of the tongue;
- convulsions;
- muscle spasms.
Diacarb is a low-toxic drug. When used, tinnitus, paresthesia, convulsions and, extremely rarely, according to reviews of Diakarb, myopia may occur. With prolonged use of the drug - disorientation, dizziness, impaired sense of touch, drowsiness. In these cases, you cannot drive vehicles or perform work that requires increased concentration.
The drug should be administered with caution for more than 5 days in a row due to an increased risk of metabolic acidosis. Therefore, with long-term use, the peripheral blood picture should be monitored, as well as indicators of water-electrolyte and acid-base balance.
In some cases, according to reviews of Diakarb, allergic reactions (itching or urticaria), anorexia, and muscle weakness may develop.
With long-term use of the drug - transient hematuria, nephrolithiasis, glucosuria, vomiting, nausea, diarrhea, hemolytic anemia, leukopenia or agranulocytosis.
When using Diacarb with theophylline and other diuretics, it should be taken into account that the drug enhances the diuretic effect, and when used simultaneously with acid-forming diuretics, it reduces it. When used in complex therapy with antiepileptic drugs, Diacarb enhances the manifestations of osteomalacia.
Cases of overdose or acute poisoning by the drug have not been described.
Pharmacological features
What do Diacarb tablets help with? According to the instructions, the drug has the following therapeutic properties:
- diuretic;
- antiglaucoma;
- antiepileptics;
- help reduce intracranial pressure.
When compared with other diuretic drugs, the diuretic effect of Diacarb is weaker. When fluid is removed from the body, a large number of potassium ions are removed along with it. It is for this reason that during treatment, patients are additionally prescribed medications that enrich the body with potassium and magnesium (for example, Panangin, Asparkam).
In a smaller volume, compared with potassium ions, phosphates, calcium and magnesium ions are washed out of the body. To avoid the development of metabolic disorders, it is necessary to replenish the losses of relevant microelements. This recommendation applies to cases where the course of treatment lasts 2 weeks or more.
The mechanism of action of the drug is such that after 3 days it loses its diuretic effect. Therefore, using it to remove excess fluid for longer than this period is considered inappropriate. However, if 2 days after you start taking it you take a short break for 1-3 days, the medication again begins to have a diuretic effect. As a result, you need to take Diacarb not continuously, but with short breaks.
Diuretic is not the only effect that is stated in the instructions. The drug also has an antiglaucoma effect. After its use, the production of moisture in the anterior chamber of the eye decreases, and intraocular pressure decreases.
Diacarb also reduces the amount of fluid produced in the cerebral ventricles and cerebrospinal fluid. This helps normalize intracranial pressure and the dynamics of cerebral cerebrospinal fluid. Therefore, the medicine is often prescribed to patients in the complex treatment of various disorders caused by increased intracranial pressure.
The antiepileptic effect is achieved due to the fact that the drug stops foci of pathological excitability in the structures of the brain.
In addition to the above therapeutic properties, side effects of the drug are often used in practice, namely the ability to cause metabolic acidosis. It eliminates respiratory disorders, including sleep apnea.
During pregnancy and lactation
Diacarb is not used during pregnancy, since the active substance has the ability to penetrate the placenta and negatively affect the development of the fetus.
Acetazolamide is excreted in small quantities into breast milk. Diakarb during breastfeeding (in the presence of an active lactation process) requires stopping breastfeeding. The entire treatment process must be carried out under the supervision of a doctor.
The pharmaceutical product should not be used by pregnant women and women breastfeeding.
Using the medication for more than 5 days increases the risk of a disorder with increased acidity and decreased pH balance in the body (acidosis).
The risk factor for acidosis increases in the elderly and in people with severe renal impairment.
Use in pregnant women and children
During pregnancy, Diakarb is not recommended for use, since there is no data on its effect on the fetus. If indicated, you can take pills starting from the second trimester under strict medical supervision.
Acetazolamide can pass into breast milk, so breastfeeding should be stopped during treatment.
The drug has a weak diuretic effect, so to achieve results it must be used as part of a complex treatment.
For children, the medicine can be prescribed for increased intracranial pressure, hydrocephalus, and epilepsy. It is usually used after reaching the age of three; it is rarely prescribed to infants and not earlier than 4 months. Before using Diacarb in children, it is necessary to carefully weigh the expected benefits and possible risks.
Interaction with other tools
- Folic acid antagonists;
- hypoglycemic agents;
- anticoagulants;
- Phenytoin;
- Primidone;
- Atropine;
- Quinidine;
- Carbamazepine;
- cardiac glycosides;
- Ephedrine;
- Mmorelaxants;
- Carbonic anhydrase inhibitors with a different chemical structure;
- Cyclosporine.
Compatibility with Acetylsalicylic acid is not recommended, since toxic effects on the functioning of the nervous system and acidosis with possible fatal outcomes develop.
Diakarb is used with extreme caution in combination with hypertensive drugs and cardiac glycosides. It is important to adjust the dosages of these groups of drugs.
Diacarb leads to a decrease in the effectiveness of drugs containing lithium salts. Diuretics, the mechanism of action of which is based on the formation of acids, reduce the effectiveness of Diacarb.
Combinations with drugs containing Sodium Bicarbonate lead to increased formation of insoluble kidney stones (stones).
Alcohol
Ethyl alcohol negatively affects the health of people with glaucoma, epilepsy and increased intracranial pressure. Alcohol and Diacarb have poor compatibility and, in combination with each other, negatively affect the liver and kidneys, so we advise you to completely abstain from alcohol during treatment with the drug.
It is prohibited to use the drug "Diacarb" in the treatment of children under three years of age.
Ethyl alcohol has a negative effect on the body, especially in patients with epilepsy, glaucoma and heart pathologies. The interaction of Acetazolamide with alcohol should be prevented. Diacarb and alcohol are characterized by poor compatibility, which can have dangerous consequences for the patient’s body.
Overdose
The instructions for use of the medication clearly indicate the procedure for using and prescribing the medication for certain pathological conditions.
Edema syndrome. The initial dose of the drug is set within 250-375 mg once a day in the morning. The greatest diuretic result is achieved when using the medication after 1 day or 2 days without a break, with an interval of a day. It is recommended to use medications that improve blood circulation and medications with cardiotonic and antiarrhythmic effects together with Diacarb. It is necessary to adhere to a diet that compensates for the lack of potassium, but limit the intake of salt into the body.
Open angle glaucoma. For adults, the recommended therapeutic dose is 250 mg 1-4 times a day. A portion of the drug greater than 1 g does not increase the therapeutic result. For the treatment of secondary glaucoma, it is recommended to take 250 mg of the drug every 4 hours. Some patients report relief from short-term use of the pharmaceutical drug at a dose of 250 mg 2 times a day. Acute attacks of glaucoma require increasing the dosage to 250 mg 4 times a day.
An attack of glaucoma in children is treated with medication at a dose of 10-15 mg per kilogram of body weight per day, divided into 3-4 doses.
Epilepsy. Patients suffering from this disease are recommended to take Diacarb 250-500 mg per day for 3 days, taking a break on day 4. Children from 4-12 months - 50 mg per 24 hours, divided into 1-2 times, 2-3 years - 50-125 mg per 24 hours, divided into 1-2 times, 4-18 years - 125-250 mg once a day in the morning.
Mountain sickness. The pharmaceutical product is prescribed at a dose of 500-1000 mg per day, divided into several doses. When climbing mountains at high speed, 1000 mg per day is used, divided into doses. Therapy is started a day or two before climbing the mountains; if signs of the disease appear, treatment is continued for another 2 days or more, if necessary.
Indications for use
According to the instructions for use, Diacarb is prescribed for the treatment of the following diseases and pathological conditions:
- mild or moderate edema syndrome associated with disruptions in cardiovascular activity, medication or other disorders;
- different forms of glaucoma (primary, secondary, open- or closed-angle);
- respiratory diseases, including bronchial asthma, pulmonary emphysema;
- heart failure;
- gout;
- swelling caused by premenstrual syndrome;
- epilepsy;
- preeclamptic state;
- "altitude" sickness;
- Meniere's disease;
- Titania.
Indications for use of Diakarb Asparkam: preparation for ophthalmological operations to remove glaucoma to eliminate edema and reduce the likelihood of their development in the postoperative period.
Adverse reactions
Diacarb during therapy can cause a number of adverse effects on the body:
- Hearing impairment (lack of perception or noise), changes in consciousness, loss of muscle tone, painful sensitivity to light in the organs of vision, temporary loss of vision, drowsiness.
- Loss of appetite, painful sensation in the epigastric region and pharynx, leading to vomiting, diarrhea, increased urine production, blood in the urine, hepatic colic, urolithiasis, kidney stones.
- An imbalance between anions and cations, the occurrence of a disorder with increased acidity and a decrease in pH balance in the body.
- A decrease in the number of white blood cells and platelets in the blood, agranulocytosis, a disorder of the hematopoietic capacity of the bone marrow, pancytopenia.
- Anaphylactic shock, acute, toxic epidermal necrolysis, malignant exudative erythema, multimorphic exudative erythema, manifestations in the form of rash, itching on the skin.
Diakarb's analogs
There are no structural analogues of Diacarb for the active substance – acetazolamide.
The drug has analogs that are identical to the active ingredient and therapeutic effect on the body:
- Acetazolamide produced in Moldova.
- Acetazolamide-Acri Russian analogue.
- Diuremide produced in Ukraine.
- Diamox made in the USA.
- Fonurit manufacturer Hungary.
- Diuremide tablets (Ukraine) containing 250 mg of Acetazolamide per dose;
- Fonurit;
- Acetazolamide;
- Diamox;
- Diluran;
- Ederen;
- Acetamoc;
- Renamide.
Diacarb differs from such products only in the manufacturer and origin of the active substance. The effectiveness of these drugs is no different.
Reviews
Attention! The information presented in the article is for informational purposes only. The materials in the article do not encourage self-treatment. Only a qualified doctor can make a diagnosis and give treatment recommendations based on the individual characteristics of a particular patient.
Marina Ivanenko, 38 years old
“The doctor prescribed a drug to reduce intracranial pressure. After taking the medication, the headaches began to bother me much less often.”
Anatoly Sahoy, 47 years old
“Diacarb” helps relieve swelling, since I have had heart problems for a long time. I started feeling much better.”
Reviews from patients
Inna R.: I have had epilepsy since I was young, I often have headaches, and lately I have had problems with skin and hair loss. As part of the complex treatment, the doctor prescribed Diacarb and Deacur (Biotin). I clarified what these tablets (Diacarb) are taken for. The doctor indicated that they help reduce intracranial pressure, as well as excessive irritation of the nerve cells in the brain that provoke attacks. I’ve been taking Diacarb for a week now and I’m happy with the results.
Kirill G.: I have chronic heart pathologies. The radiologist recommended Furosemide (Diacarb) and Asparkam (Panangin) in adult dosages. I will say that after 7 days of using the drug Diacarb, the swelling did not worsen, and even almost completely disappeared. The drug helps a lot and is very gentle. The difference is that Furosemide is more aggressive, but not more effective for me. Therefore, replacement with domestic Furosemide was not carried out.
Reviews from medical specialists
Olga Kharchenko, cardiologist: in my experience, Russian (cheaper) and foreign analogues of Diakarb are often less effective, especially for chronic heart pathologies accompanied by edema. Diakarb perfectly helps to gently eliminate tissue swelling and reduce the load on the heart.
Irina Kural, neurologist: I am always pleased with the results of patients using Diacarb, including those with epilepsy. The drug is approved from the age of 3, so I often use it to treat children. Analogues produced by the domestic pharmaceutical industry (Russian) are cheaper. But their effectiveness does not always satisfy the doctor and the patient. Diakarb is quite affordable in price, so there is no point in making replacements.
Compatibility with other medical devices
When using the drug simultaneously with other medications, the following is noted:
- Increased diuretic effect from diuretic medications. Reduction of the diuretic reaction when taken in parallel with acid-forming diuretics.
- Increased toxic effects when taken in parallel with increased portions of depolarizing muscle relaxants, carbamazepine, ephedrine, acetylsalicylic acid.
- Acetazolamide may increase the effect of antidiabetic agents and medications that affect blood viscosity.
- When used in parallel with medications that increase blood pressure, the dose of acetazolamide is adjusted.
- Diacarb is able to increase the concentration of antiepileptic drugs from the carboxamide group in the blood.
If a pharmaceutical dose is missed, increasing subsequent doses is not required.
Do not use the medicine for more than 7 days.
During long-term treatment, periodic monitoring of the blood count, the equilibrium indicator of anions and cations in the body, and the balance of acids and bases is desirable.
Best before date
Diacarb is classified as a List B drug. Shelf life is 5 years.
The period of suitability is no longer than 5 years. After the expiration date, use is unacceptable
Diakarb is stored for 5 years from the date of issue. After the specified expiration date, the drug is not used.
tablets 250 mg - 5 years.
tablets 250 mg - 5 years.
Do not use after the expiration date stated on the package.
Synonyms of nosological groups
| Category ICD-10 | Synonyms of diseases according to ICD-10 |
| E87.3 Alkalosis | Hypokalemic alkalosis |
| Hypokalemic alkalosis with hypercalciuria | |
| Respiratory alkalosis | |
| Metabolic alkalosis | |
| Alkalosis in liver diseases | |
| Respiratory alkalosis | |
| Hypochloremic alkalosis | |
| Respiratory alkalosis | |
| Metabolic alkalosis | |
| G40 Epilepsy | Atypical seizures |
| Atonic seizures | |
| Grand mal seizures | |
| Grand mal seizures in children | |
| Grand mal seizures | |
| Generalized absence seizures | |
| Jacksonian epilepsy | |
| Diffuse grand mal seizure | |
| Diencephalic epilepsy | |
| Cortical and non-convulsive forms of epilepsy | |
| Primary generalized seizures | |
| Primary generalized seizure | |
| Primary generalized seizure | |
| Primary generalized tonic-clonic seizure | |
| Pycnoleptic absence | |
| Repeated epileptic seizures | |
| Generalized seizure | |
| Convulsive seizure | |
| Refractory epilepsy in children | |
| Complex seizures | |
| Mixed seizures | |
| Mixed forms of epilepsy | |
| Convulsive state | |
| Seizures | |
| Convulsive conditions | |
| Convulsive forms of epilepsy | |
| Grand mal epilepsy | |
| Epileptic seizures | |
| G93.2 Benign intracranial hypertension | Intracranial hypertension |
| Intracranial hypertension | |
| Increased intracranial pressure | |
| Persistent cerebral hypertension | |
| H40 Glaucoma | Antiglaucoma intervention |
| Aphakic glaucoma | |
| Narrow-angle glaucoma | |
| Chronic glaucoma | |
| Chronic open-angle glaucoma | |
| Wide angle glaucoma | |
| H40.9 Glaucoma, unspecified | Aphakia with glaucoma |
| Acute glaucoma | |
| Acute attack of glaucoma | |
| R60 Edema, not elsewhere classified | Painful swelling after injury or surgery |
| Painful swelling after surgery | |
| Dropsy | |
| Dystrophic nutritional edema | |
| Lymphostasis and swelling after breast cancer therapy | |
| Swelling due to sprains and bruises | |
| Edema due to the constitution | |
| Edema of renal origin | |
| Peripheral edema | |
| Edema-ascitic syndrome in liver cirrhosis | |
| Edema syndrome | |
| Edema syndrome intoxication | |
| Edema syndrome due to secondary hyperaldosteronism | |
| Edema syndrome of hepatic origin | |
| Edema syndrome in heart diseases | |
| Edema syndrome in congestive heart failure | |
| Edema syndrome in heart failure | |
| Edema syndrome in heart failure or cirrhosis of the liver | |
| Pastosity | |
| Peripheral congestive edema | |
| Peripheral edema | |
| Hepatic edema syndrome | |
| Premenstrual edema | |
| Cardiac edema syndrome | |
| Iatrogenic edema | |
| R60.9 Edema, unspecified | Dropsy of the joints |
| Inflammatory swelling of soft tissues | |
| Dysproteinemic edema | |
| Fluid retention in the body | |
| Fluid retention in obesity | |
| Edema | |
| Hypothyroid edema | |
| Edema of renal origin | |
| High altitude edema | |
| Edema syndrome in muscular-articular diseases | |
| Increased accumulation of fluid in body tissues | |
| T70.2 Other and unspecified effects of high altitude | Acclimatization to high altitudes |
| Barotraumatic osteonecrosis | |
| Acosta's disease (d'Acosta) | |
| altitude sickness | |
| Altitude sickness | |
| High altitude pulmonary edema | |
| Altitude sickness | |
| Retinal hemorrhages at altitudes | |
| Monkhe disease | |
| High altitude edema | |
| Z100* CLASS XXII Surgical practice | Abdominal surgery |
| Adenomectomy | |
| Amputation | |
| Angioplasty of coronary arteries | |
| Carotid angioplasty | |
| Antiseptic treatment of skin for wounds | |
| Antiseptic hand treatment | |
| Appendectomy | |
| Atherectomy | |
| Balloon coronary angioplasty | |
| Vaginal hysterectomy | |
| Corona bypass | |
| Interventions on the vagina and cervix | |
| Bladder interventions | |
| Intervention in the oral cavity | |
| Restorative and reconstructive operations | |
| Hand hygiene of medical personnel | |
| Gynecological surgery | |
| Gynecological interventions | |
| Gynecological surgeries | |
| Hypovolemic shock during surgery | |
| Disinfection of purulent wounds | |
| Disinfection of wound edges | |
| Diagnostic interventions | |
| Diagnostic procedures | |
| Diathermocoagulation of the cervix | |
| Long surgical operations | |
| Replacing fistula catheters | |
| Infection during orthopedic surgery | |
| Artificial heart valve | |
| Cystectomy | |
| Short-term outpatient surgery | |
| Short-term operations | |
| Short-term surgical procedures | |
| Cricothyroidotomy | |
| Blood loss during surgery | |
| Bleeding during surgery and in the postoperative period | |
| Culdocentesis | |
| Laser coagulation | |
| Laser coagulation | |
| Laser coagulation of the retina | |
| Laparoscopy | |
| Laparoscopy in gynecology | |
| CSF fistula | |
| Minor gynecological operations | |
| Minor surgical interventions | |
| Mastectomy and subsequent plastic surgery | |
| Mediastinotomy | |
| Microsurgical operations on the ear | |
| Mucogingival surgeries | |
| Stitching | |
| Minor surgeries | |
| Neurosurgical operation | |
| Immobilization of the eyeball in ophthalmic surgery | |
| Orchiectomy | |
| Complications after tooth extraction | |
| Pancreatectomy | |
| Pericardectomy | |
| Rehabilitation period after surgery | |
| The period of convalescence after surgical interventions | |
| Percutaneous transluminal coronary angioplasty | |
| Pleural thoracentesis | |
| Pneumonia postoperative and post-traumatic | |
| Preparing for surgical procedures | |
| Preparing for surgery | |
| Preparing the surgeon's hands before surgery | |
| Preparing the colon for surgery | |
| Postoperative aspiration pneumonia during neurosurgical and thoracic operations | |
| Postoperative nausea | |
| Postoperative bleeding | |
| Postoperative granuloma | |
| Postoperative shock | |
| Early postoperative period | |
| Myocardial revascularization | |
| Resection of the apex of the tooth root | |
| Gastric resection | |
| Bowel resection | |
| Resection of the uterus | |
| Liver resection | |
| Small bowel resection | |
| Resection of part of the stomach | |
| Reocclusion of the operated vessel | |
| Bonding tissue during surgery | |
| Removing stitches | |
| Condition after eye surgery | |
| Condition after surgery | |
| Condition after surgical interventions in the nasal cavity | |
| Condition after gastrectomy | |
| Condition after resection of the small intestine | |
| Condition after tonsillectomy | |
| Condition after removal of the duodenum | |
| Condition after phlebectomy | |
| Vascular surgery | |
| Splenectomy | |
| Sterilization of surgical instruments | |
| Sterilization of surgical instruments | |
| Sternotomy | |
| Dental operations | |
| Dental intervention on periodontal tissues | |
| Strumectomy | |
| Tonsillectomy | |
| Thoracic surgery | |
| Thoracic operations | |
| Total gastrectomy | |
| Transdermal intravascular coronary angioplasty | |
| Transurethral resection | |
| Turbinectomy | |
| Removal of a tooth | |
| Cataract removal | |
| Cyst removal | |
| Tonsil removal | |
| Removal of fibroids | |
| Removal of mobile baby teeth | |
| Removal of polyps | |
| Removing a broken tooth | |
| Removal of the uterine body | |
| Removing stitches | |
| Urethrotomy | |
| CSF duct fistula | |
| Frontoethmoidohaymorotomy | |
| Surgical infection | |
| Surgical treatment of chronic limb ulcers | |
| Surgery | |
| Surgery in the anal area | |
| Colon surgery | |
| Surgical practice | |
| Surgical procedure | |
| Surgical interventions | |
| Surgical interventions on the gastrointestinal tract | |
| Surgical interventions on the urinary tract | |
| Surgical interventions on the urinary system | |
| Surgical interventions on the genitourinary system | |
| Heart surgery | |
| Surgical procedures | |
| Surgical operations | |
| Vein surgery | |
| Surgical intervention | |
| Vascular surgery | |
| Surgical treatment of thrombosis | |
| Surgery | |
| Cholecystectomy | |
| Partial gastrectomy | |
| Transperitoneal hysterectomy | |
| Percutaneous transluminal coronary angioplasty | |
| Percutaneous transluminal angioplasty | |
| Coronary artery bypass surgery | |
| Tooth extirpation | |
| Extirpation of baby teeth | |
| Pulp extirpation | |
| Extracorporeal circulation | |
| Tooth extraction | |
| Tooth extraction | |
| Cataract extraction | |
| Electrocoagulation | |
| Endourological interventions | |
| Episiotomy | |
| Ethmoidotomy |
special instructions
During treatment, the dosage regimen should be followed. Exceeding doses can lead not only to the development of serious side effects, but also cause life-threatening conditions such as coma or death of the patient (extremely rare).
If the patient missed a dose of the drug, then the next dosage should be taken as usual, without doubling it.
Before driving, you should assess the tolerability of the drug, which can cause dizziness, drowsiness, and decreased attention.
Storage
The pharmaceutical product is stored in a dry place at 25 °C, away from children and away from sunlight.
On prescription.
At a temperature not exceeding 25 °C.
Keep out of the reach of children.
Diacarb can be purchased at a pharmacy only if you have a prescription written on a special form in Latin, indicating the INN of the drug (in Latin).
The drug is stored in dry rooms where there is no direct light. Recommended storage temperature is no more than 25⁰C. Children should not have access to the medicine.