What is a bladder tumor
Neoplasms in bladder tissue can be of many types and have different activities in terms of the formation of metastases.
Victims of the disease are predominantly people over 55 years of age, often living in environmentally unfavorable areas or working in hazardous industries. Negative changes in the environmental situation, social factors and smoking are partly to blame for the increase in the frequency of tumor diagnosis.
Bladder tumors in men are 6 times more common than in women, which is associated with some anatomical and physiological characteristics of the male body:
- genetic predisposition, increasing after 50 years;
- hormonal disorders that stimulate tumor development;
- development of prostate adenoma.
The most common types of tumors are:
- benign tumor of the bladder (highly differentiated), located on the surface of the mucosa;
- malignant tumor (poorly differentiated) affecting muscle tissue.
In the first case, the growth of the tumor occurs in the direction of the bladder cavity, forming a connection in the form of a stalk with the mucous surface. As a rule, a tumor with such a growth pattern is called exophytic or papillary.
The second type is characterized by intensive growth into the tissue structure with the rapid formation of metastases. This type of tumor is called endophytic or invasive.
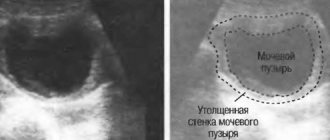
Ultrasound examination
The bladder in women and men is examined using ultrasound diagnostics. This method is painless and is indicated for newborns and older children. Before carrying out the manipulation, the bladder must be full in order to obtain the most reliable information. The procedure is carried out in several ways:
- transabdominal (access through the abdominal wall);
- transvaginal (using a vaginal sensor);
- transrectal (introducing the sensor through the rectum).
Ultrasound examination today is the most acceptable diagnostic method, which provides the most accurate information. It is used to determine the presence of tumors and stones in the bladder. At the same time, the doctor is able to identify abnormalities in the functioning of the uterus and appendages in women.
Mechanism of development (pathogenesis)
All cells of the body contain genetic material, which determines their functional activity and the intensity of the division process (proliferation). Certain changes (mutations) in the genome can lead to the fact that such cells become foreign to the body and begin to rapidly divide with the formation of a neoplasm that has several distinctive malignant properties:
- Rapid increase in size - the intensity of division of genetically altered cells is significantly higher than that of healthy ones. The possibility of growth of a tumor malignant neoplasm is limited only by the resources of the body, which provides it with nutritional compounds and oxygen.
- Invasive growth with germination into healthy tissues and their destruction.
- Metastasis is the formation of daughter malignant neoplasms in various organs and tissues, which is a consequence of the spread of cancer cells from the primary tumor through the blood and lymph.
- Altered metabolism (metabolism) of tumor cells, as a result of which waste products are released that are toxic to the human body.
Such features of a cancerous tumor are the main reason for the rather difficult treatment (in most cases, radical cancer therapy is impossible), as well as the high frequency of deaths, which often occur when the oncological process is not detected in a timely manner.
One of the features of cancer cells is the synthesis and release of biologically active compounds that stimulate the growth of blood vessels in the tumor. The malignant neoplasm thus “provides” itself with nutrition.
What is studied through cytology
Cytological examination of the bladder is a study using a microscope of sediment from a urine sample obtained after centrifugation of the biomaterial. This study is carried out by a histologist in a laboratory setting.
The purpose of cytology is to detect abnormal cells that may be excreted in the urine. Diagnostics makes it possible to accurately identify the presence of a malignant process in the organs of the urinary system.
However, if you receive an unsatisfactory, atypical or suspicious result, you should resort to repeated and additional tests.
Causes (etiology)
For modern medicine, the exact reasons for the development of tumors in the body, including tumors that form in the bladder, remain unknown. There is a group of predisposing factors that, according to statistical data, can contribute to the appearance of neoplasms, which include:
- hormone imbalance, decreased activity of the body's defense system;
- harmful substances in the environment;
- chronic inflammatory processes in the urethra and bladder, as well as other pathologies of the genitourinary system (leukoplakia, cervical cystitis, urolithiasis, prostatitis, ulceration of the bladder walls, etc.);
- stagnant processes in the bladder in combination with smoking (often harmful chemicals contained in cigarette smoke linger on the walls of the bladder and provoke the proliferation of its epithelial cells);
- parasite infestations (schistosomiasis, bilharzia and others);
- the patient's age and anatomical features of the bladder.
Classification of benign bladder tumors
These neoplasms can be of epithelial and non-epithelial origin. Epithelial benign tumors are not common, since the majority of neoplasms from the epithelium are malignant. Benign epithelial neoplasms include polyps and papillomas, some of which may have a tendency to malignancy.
Polyps come in various sizes and are tissue protrusions into the lumen of the bladder. This type of urological tumors can be single or multiple.
Bladder papillomas grow from the surface epithelium and are mature neoplasms with exophytic growth. Microscopic examination reveals the presence of a velvety, papillary surface.
They are pinkish-white in color and soft in texture. Papillomas can also be multiple or single in nature, and sometimes there is total damage to the walls of the bladder in the form of papillomatosis.
Benign neoplasms of non-epithelial etiology include: fibroids, fibromas, hemangiomas, fibromyxomas, neuromas.
There is no generally accepted hypothesis regarding the etiology of bladder cancer. However, there are certain risk factors that significantly contribute to the development of bladder cancer.
Against the backdrop of numerous studies, which have been especially active lately, an exact answer has not yet been found regarding the causes of the disease. However, during scientific research, scientists were able to identify various factors that by themselves cannot cause tumor growth, but under a combination of circumstances increase the risk of the disease.
Carcinogenic substances entering the body go through all stages of metabolism and are partially excreted by the kidneys. They are the root cause of the development of tumors, since they are in direct contact with the mucous membrane of the bladder.
Exposure to carcinogens can disrupt the functioning of the genetic apparatus of cells, thereby interfering with the reproduction of cells characteristic of a given organ and provoking the growth of cancer cells.
The main external causes that provoke the development of bladder cancer:
- daily exposure to volatile chemicals generated during the production of plastic, rubber and other products or paint production;
- smoking;
- exposure to ionizing radiation;
- viral diseases (mainly human papillomavirus, which has highly oncogenic properties);
- systematic untimely or incomplete emptying of the bladder with prostate adenoma;
- chronic inflammatory diseases of the bladder.
An increase in the size of the prostate gland with a prostate provokes the development of congestion in the bladder and impairs the elasticity of the muscle layer. The inability to completely empty the bladder causes deformation of the walls of the bladder; they stretch, creating a “reservoir” where urine accumulates and the negative impact on the mucous membrane increases.
Chronic inflammatory diseases are also risk factors, since the process of tissue regeneration that occurs during inflammatory processes, under the influence of carcinogens or due to genetic disorders can acquire the nature of metaplasia, that is, the replacement of damaged cells with modified cells or cells that do not belong to the organ.
Often this process is characterized as leukoplakia of the bladder walls and is a precancerous condition.
Types of bladder tumors - how to distinguish benign neoplasms from oncology?
This pathology currently accounts for about 4% of all types of cancer. Every year this figure increases. It is primarily older men who are at risk. In women, this disease is diagnosed 4 times less often, and in children – 60 times less often than in men.
The symptoms of this disease depend on the type of tumor, its location, and stage of development.
They are a defective proliferation of connective tissue cells that are attached to the mucous membrane of the bladder with the help of a thin stalk.
Externally, in their shape, they resemble a mushroom, the stem of which is directed into the cavity of the bladder. They have a smooth surface, soft in structure and quite fragile.
Technique of the procedure
Cystoscopy is done using a special instrument - a cystoscope. In its structure, it is one of the types of endoscope with a mini-camera and a lighting lamp at one end and a manual control system at the other.
There are several types of cystoscope: flexible and rigid.
Flexible cystoscope
Rigid cystoscope
The latter is used extremely rarely, only when such a choice is due to the specific purpose of the study.
The duration of cystoscopy varies from 25-40 minutes for diagnosis to 1.5-2 hours for therapeutic procedures.
Types of formations
Degrees of education.
Increase. Among bladder formations, classification according to morphological criteria divides them into the following:
- Malignant;
- Benign.
In this case, they can be of the following origin:
- Epithelial;
- Non-epithelial.
Most neoplasms of this type are epithelial (95%). Moreover, 90% of this number is cancer.
Those types of tumors that are benign are cysts, polyps, and papillomas. However, such epithelial neoplasms can be called benign very conditionally.
The reason for this is that tumors of this type have a large number of transitional forms, and therefore often become malignant (degenerate). The most common types are infiltrating and papillary cancer.
Cysts in the bladder are benign formations filled with glandular contents.
Polyps in this organ are papillary formations located on a thin (sometimes wide) fibrovascular base (neck), which are covered with unchanged urothelium.
Papillomas that form in the bladder are mature tumors that have exophytic growth. Moreover, they develop from the upper layer of the epithelium. Such formations have a papillary surface and a soft consistency. Sometimes multiple papillomas can be detected, more rarely – diffuse papillomatosis.
Worth knowing! Benign formations of the non-epithelial type include myomas, fibromas, and neuromas. If we talk about malignant tumors of the bladder, then these are sarcomas. They have very rapid growth, as well as early formation of metastases. Myofibroblastic tumor is also found, but very rarely and it is represented by spindle-shaped myofibroblasts.
Depending on the tissue structure of the tumor, bladder cancer is divided into several histological types, which include:
- Transitional cell papilloma.
- Squamous cell papilloma.
- Transitional cell carcinoma (the tumor that is diagnosed most often).
As the oncological process progresses, there are 4 stages of development of bladder cancer:
- Stage 1 – the size of the tumor is minimal, and it does not destroy tissue and does not metastasize.
- Stage 2 – the tumor enlarges, grows through the basement membrane, and gives single metastases to nearby lymph nodes.
- Stage 3 – the size of the tumor is significant; with exophytic growth, it can lead to disruption of the functional activity of the bladder; also, against the background of multiple metastases in the regional lymph nodes, single daughter tumors are detected in distant organs.
- Stage 4 is the terminal stage of the oncological process with multiple distant metastases, as well as the development of severe cancer intoxication.
The classification of bladder cancer allows the oncologist to select the most optimal treatment.
In modern oncology, the TNM classification is used, which is based on tumor size, involvement of regional lymph nodes, and the presence of distant metastases.
Bladder tumors are a pathological process caused by the appearance of malignant atypical cells in the mucous layer or in any other layer of the bladder.
Bladder oncology
Pathologies
Bladder tumors, as a variety of nosoological units that have been classified, are a fairly common disease: its incidence is approximately 6% of all cases.
This disease occupies the 12th level in the structure of diagnoses.
The incidence of this pathology is approximately 13 cases per 100,000 people over an annual period.
Residents of developed regions, residents of Europe and the USA, and representatives of the white race are susceptible to this disease.
Tumor processes, united by the concept of “bladder cancer,” differ in histological type, degree of cell differentiation, growth pattern, and tendency to metastasize. Taking these characteristics into account is extremely important when planning treatment tactics.
According to morphological characteristics, the most common in oncourology are transitional cell (80-90%), squamous cell cancer of the bladder (3%), adenocarcinoma (3%), papilloma (1%), sarcoma (3%).
Based on the degree of anaplasia of cellular elements, low-, moderate- and highly differentiated bladder cancer is distinguished.
Of practical importance is the degree of involvement of different layers of the bladder in the cancer process, and therefore they speak of low-stage superficial bladder cancer or high-stage invasive cancer. The tumor can have a papillary, infiltrative, flat, nodular, intraepithelial, or mixed growth pattern.
According to the international TNM system, the following stages of bladder cancer are distinguished.
- T1 – tumor invasion affects the submucosal layer
- T2 – tumor invasion extends to the superficial muscle layer
- T3 – tumor invasion extends to the deep muscular layer of the bladder wall
- T4 – tumor invasion affects the pelvic tissue and/or adjacent organs (vagina, prostate gland, abdominal wall)
- N1-3 – metastasis to regional or adjacent lymph nodes is detected
- M1 - metastasis to distant organs is detected
First of all, regardless of location, neoplasms can be divided into benign (relatively safe) and malignant (dangerous).
Signs of good quality:
- growth with “pushing apart” tissues or into an organ cavity;
- grow relatively slowly, sometimes “freeze” for years;
- the cellular composition of such a tumor has a high degree of differentiation (it is possible to distinguish whether it belongs to a certain type of tissue);
- not capable of spreading (no metastases);
Signs of malignancy:
- grow deep into the tissue, damaging it;
- growth is fast, rapid;
- often ulcerate, easily injured, bleed;
- low degree of differentiation (tissue type is not determined);
- capable of spreading (give metastases).
A) Neoplasms from epithelial tissue (they account for 95 cases out of 100):
- transitional cell papilloma, squamous cell;
- cancer (glandular, squamous or mixed type);
- adenocarcinoma;
- cancer with a complete lack of differentiation of cellular composition.
B) Changes in the epithelial layer of a non-tumor nature:
- papillomatous hyperplasia - against the background of inflammation, more often with a parasitic lesion, there is a small, scattered proliferation of epithelial tissue. It is very reminiscent of papillomas, but essentially is not one;
- cystic cystitis - the formation of microcysts covered with several layers of epithelial tissue;
- von Brunn's nests are a tumor-like disease characterized by the proliferation of epithelial cells in the form of isolated formations, giving the bladder cavity a rough appearance;
- glandular cystitis is essentially a further development of cystic cystitis, in this case the microcyst cavity is covered with cylindrical cells and mucus-producing cells;
- nephrogenic metaplasia;
- degeneration of the squamous cell type (leukoplakia).
B) Tumor-like formations:
- cystic adenomyosis is a disease characteristic only of women. Characterized by the proliferation of uterine endometrial cells outside their normal anatomical structures;
- Follicular cystitis is one of the complications of cystitis, which is chronic. It is characterized by a significant proliferation of lymphoid follicles in the submucosa, which gives the bladder membrane unevenness;
- polypoid cystitis is a disease characterized by the proliferation of connective tissue in the thickness of the bladder wall; the underlying epithelium does not change. This disease is often called pseudopolyp;
- cystic cysts are cavities filled with fluid. Can form from von Brunn nests. Depending on the location and size, they can often block the outflow of urine, causing the volume of the bladder cavity to change;
- Bladder teratomas are a type of tumor-like formation characterized by a mixtome, that is, the content of various tissue structures;
- Malakoplakia is a disease that can rarely be found in the walls of the bladder. Malakoplakia occurs 4 times more often in women than in men. In appearance, it resembles small, gray or brownish plaques, which may contain ulceration in the central part. The preceding background is a chronic inflammatory process;
- cystic amyloidosis - this disease is so rare that it can rather be considered casuistry. It appears only in severe cases, it can be found in the submucosal layer.
Symptoms and clinical course:
- a feature of the tumor process is the complete absence of a clinical picture in the early stages of the disease, which makes timely diagnosis and treatment difficult;
- benign neoplasms may not be detected for a long time, may be discovered by chance, or may even be discovered after death without being its immediate cause;
- symptoms of a benign tumor: impaired urine outflow, acute urinary retention, rapid filling of the bladder;
- symptoms of a malignant tumor: the appearance of blood in the urine, initially a short-term phenomenon, then becomes permanent. Symptoms of dysuria include frequent, painful urination. Pain is the third characteristic sign. General symptoms: emaciation, exhaustion, malaise, weakness, aversion to meat foods.
Almost all pathological neoplasms of the bladder are a consequence of the development of transitional cell carcinoma. However, there is a possibility of developing other forms:
- squamous cell carcinoma;
- glandular cancer (adenocarcinoma);
- undifferentiated tumor;
- lymphoma.
Epithelial neoplasms:
- some types of papillomas (transitional cell and squamous cell);
- transitional cell carcinoma;
- combination of transitional cell carcinoma with tissue metaplasia;
- glandular cancer;
- undifferentiated cancer;
- squamous cell carcinoma.
Neo-epithelial neoplasms:
- highly differentiated neoplasms (benign bladder tumor);
- poorly differentiated neoplasms (rhabdomyosarcoma).
Neoplasms with metastatic spread:
- glandular metaplasia;
- polypoid cystitis;
- squamous metaplasia.
Extensive tumor spread:
- multiple cystic formations;
- follicular cystitis;
- malocoplakia (extensive neoplasms in the form of multiple plaques).
Important: Non-epithelial neoplasms, especially malignant ones, are quite rare and mainly occur in young people. They are characterized by rapid growth and widespread spread of metastases.
Decoding
After a laboratory examination of urine, a specialist draws up a conclusion. For an ordinary person it is not clear, as it consists of unusual terms and numbers. Decoding largely depends on the laboratory diagnostic equipment used. This should only be done by a qualified specialist.
After studying the diagnostic results, the physician can give the patient the most accurate diagnosis. Some generally accepted designations can be found in any decoding, and they are interpreted in the same way.
- If it is indicated that the diagnostic result is unsatisfactory, then the number of atypical cells detected is not enough to make an accurate diagnosis. The patient is recommended to have his urine tested again.
- The result is atypical. Deformed cells were found in the patient's urine, but this does not mean that the person definitely has cancer. It is recommended to undergo additional research.
- Positive cytology indicates the presence of altered cells, which can be either benign or malignant.
- Negative indicators confirm the absence of atypical cells in the patient’s body.
If a patient has a positive result after cytology, it can be said that there are cancer cells in his body. The exact location of the tumor is determined using ultrasound. Additional methods for diagnosing MP oncology include various laboratory and instrumental techniques.
Only after making an accurate diagnosis can the most effective treatment be selected. Cytology of the bladder can detect malignancy at an early stage. The research is quite fast and does not take much time.
Symptoms
The first sign of bladder cancer is the presence of blood in the urine. If blood is visible to the eye, it means the tumor has grown quite large and damaged a large number of blood vessels. In the initial stages, red blood cells in the urine can only be detected under a microscope.
Aggregated blood inside the bladder often clogs the urethra, which leads to difficulty urinating and painful sensations. The tumor itself, as well as stagnant urine inside the bladder, stretches and irritates the walls, which causes a frequent urge to urinate.
The possible development of an oncological process in the bladder is indicated by a triad of characteristic symptoms, which include:
- Dysuric manifestations, characterized by the appearance of burning and pain during urination and immediately after it.
- Hematuria is the appearance of blood in the urine, which can be caused by drinking alcohol. At later stages of cancer development, blood in the urine may appear spontaneously.
- Pain is a sign indicating a significant increase in tumor size, as well as the formation of metastases of various locations.
In the later stages of development of bladder cancer, pain becomes intense, and the use of narcotic painkillers is necessary to relieve it. Cancer intoxication also develops, manifested by increased body temperature, weakness, aches and significant exhaustion of the body.
Quite often the clinical picture of this pathology is hidden. In most cases, symptoms of benign bladder tumors are dysuria and hematuria.
An early manifestation of bladder cancer is the release of blood in the urine - microhematuria or gross hematuria. Minor hematuria leads to a pinkish coloration of urine; it may be episodic and not recur for a long time.
In other cases, total hematuria immediately develops: the urine becomes bloody in color, and blood clots may be released. Prolonged or massive hematuria sometimes causes the development of bladder tamponade and acute urinary retention.
Against the background of hematuria, there is a progressive decrease in hemoglobin and anemia of the patient.
Features of the technique in different groups of patients
The procedure for internal examination of the bladder is unpleasant. But its purpose helps to identify the causes of many diseases of this organ.
Feedback from women about the sensations during the study varies and depends primarily on the type of anesthesia and general physical condition
Natalya, 34 years old I had a cystoscopy for the first time, I was terribly afraid! The procedure took place in a public hospital. When I asked about anesthesia, the doctor only smiled, which only worsened my fear. But oddly enough, the examination turned out to be not as painful as many people write. I only felt a sharp pain at the very beginning, and then just a slight discomfort.
Albina, 28 years old I had to go through cystoscopy as many as 4 times. Each time the pain was different. Without anesthesia, of course, it hurts, especially at the beginning of the procedure. But even local anesthesia greatly relieves all unpleasant sensations. But the procedure performed with a Japanese cystoscope turned out to be the most painless - only slight discomfort was felt.
Lyudmila, 39 years old I was examined with both a rigid and flexible cystoscope. So, a rigid one hurts much more than a flexible one, especially in those moments when the doctor begins to turn it. And after the procedure you have to lie in a chair for about an hour. At first, urination is very painful, regardless of the type of cystoscope. But the doctor immediately warns about this, so you just need to endure it.
Cystoscopy in women is less painful than in men. And some discomfort after it is justified by the high results obtained during the research process.
Diagnostics
Bladder cancer.
Diagnosis As a rule, it is necessary to be screened from time to time for signs of tumors, because, as already noted, the presence of symptoms already indicates a severe stage. Detection of tumor markers at the initial stage is the key to successful treatment. However, if the symptoms described above appear, you should immediately consult a doctor.
A cystoscope (a thin, tube-like instrument with a light and viewing lens) is inserted through the urethra and into the bladder. The fluid is used to fill the bladder. The doctor looks at an image of the inner wall of the bladder on a computer monitor.
In order to detect the presence of neoplasms, ultrasound, endoscopic biopsy, cystography, and CT are performed. Thus, ultrasound is a non-invasive method for diagnosing tumors, allowing one to find out their presence, location and size. To clarify the process parameters, it is necessary to obtain computed tomography and magnetic resonance imaging data.
Cystoscopy is a procedure necessary to look inside the bladder and urethra to check for abnormal areas. The cystoscope is inserted through the urethra into the bladder. A cystoscope is a thin, lamp-based instrument with lighting and special lenses for viewing. It also has an instrument for taking tissue samples, which are checked under a microscope for signs of cancer.
The most important imaging test to detect a tumor is cystoscopy, which is an endoscopic examination of the inside of the bladder. This makes it possible to identify the location of the tumor, its size and level of spread.
In addition, a transurethral biopsy is performed simultaneously. If it is not possible to take a biopsy sample, a cytological examination of urine is performed.
Emergency urography has the greatest diagnostic value for tumor research. It also allows you to understand the condition of the upper urinary tract.
Based on the results of the study, the oncologist makes a final diagnosis in accordance with the classification and also prescribes appropriate treatment.
Diagnosis of this group of pathologies is carried out on the basis of anamnesis, examination of the patient, as well as the results of instrumental and laboratory studies.
In the process of collecting anamnesis, special attention is paid to the presence of factors that can identify the patient at risk for developing neoplasms, in particular his genetic predisposition, harmful working conditions, smoking, etc.
Diagnostic measures include:
- examination by a doctor: general examination, vaginal examination in women, rectal examination in men (in parallel examination of the prostate gland);
- laboratory research methods:
- general urine test (presence of red blood cells, presence of atypical cells);
- BTA test – chromatographic method for detection of tumor antigens;
- Study of nonspecific marker substances (B-5, tumor growth factors).
- instrumental research:
- visual examination (cystoscopy) with biopsy;
- fluorescent study with aminolevulonic acid;
- Ultrasound of the pelvic organs, transvaginal examination is possible in women;
- X-ray methods (CT, MRI);
Optimal treatment depends on the type of tumor process, its prevalence and clinical manifestations.
Surgery:
- indicated in the vast majority of benign tumors and in some malignant cases;
- methods: electrocoagulation, tumor resection, removal of the entire bladder;
- palliative surgery is performed when complete removal is not possible, but is aimed at improving the quality of life.
Conservative treatment:
- drug therapy (hormonal, chemotherapy, immunotherapy, symptomatic and supportive);
- radiation therapy.
Diagnosis of a tumor is the second stage of the standard scheme, consisting of identification of symptoms, diagnosis and treatment. The purpose of diagnosis is:
- confirmation of the presence of a neoplasm;
- determination of tumor localization;
- determination of histological characteristics of the tumor;
- determining the extent of spread and the presence of metastases;
- assessment of kidney condition;
- assessment of the degree of risks during surgical intervention.
At the first stages of diagnosis, a thorough analysis of the existing symptoms is carried out:
- find out their duration;
- intensity;
- the presence of accompanying symptoms (loss of appetite, weight loss, weakness).
If there is at least one sign that raises suspicions about the presence of a neoplasm, it is necessary to conduct a set of special studies, which include:
- bimanual palpation;
- laboratory urine test;
- magnetic resonance imaging (MRI);
- excretory urography;
- ultrasound examination (ultrasound);
- cystoscopy.
After the procedure
For several days after cystoscopy, a small amount of blood may be present in the urine, and the process of urination may cause discomfort. This is due to the fact that direct contact of the urethral mucosa and the cystoscope tube causes local irritation and possible trauma. But all negative symptoms disappear after 2 - 3 days.
If the unpleasant consequences of the procedure persist for a longer period of time, a consultation with a urologist is necessary.
To prevent possible infection or inflammation of the urethra and bladder, doctors recommend a short course of antibiotics and increasing the volume of fluid consumed.
From 0.15 to 0.2 liters of contrast agent is injected into the patient's body directly into the bladder through a catheter. The patient should be lying on his back, his hips are moved to the side and slightly bent at the knees. The X-ray beam must be directed vertically, maintaining an angle of 70 degrees to the horizontal. This is necessary to eliminate shadows from the pubic bone onto the surface of the bladder.
Cystography should be performed in the right, axial and left oblique directions in order to obtain a general picture of the location of all organs in the genitourinary system. When using the axial direction, the patient must sit on the table with the device at an angle of 135 degrees horizontally. The direction of the beam is kept vertical, directly above the pubic bone.
Cystography will be successful, and the results will be accurate and clear, if the contrast fills the entire bladder. If there is not enough filling, the shadows on the final cystogram will be unclear or blurred, which will lead to an incorrect diagnosis.
The resulting contours of the organ vary depending on the age and gender of the patient. The male bladder is characterized by a round shape on the cystogram, the female bladder on the picture is oval, and in the child on the cystogram it has the shape of a pear, with its narrow part facing the pubic bone.
DETAILS: Urinalysis - the norm in women and men
Treatment
Treatment of bladder cancer
Both diagnosis and the initial measure to remove superficial tumors is TUR. After the procedure, a course of chemotherapy, external or interstitial radiotherapy is carried out. Everything taken together allows us to achieve a five-year survival rate of 68% and a ten-year survival rate of 30%.
To treat the initial stage of the tumor and prevent the return of the disease, they resort to immunological therapy - courses of intravesical administration through a catheter of the BCG vaccine, whose original classification is an antituberculosis drug. According to statistics, periodic instillations - once every 90 days for 36 months - reduce the risk of relapse by 60%.
Surgery should not be a “last resort” after a series of ineffective conservative methods. The “trial and error” method is not justified in the case of such a serious illness, otherwise even a radical measure may become too late. The decision to undergo surgical treatment for bladder cancer must be made from the moment the diagnosis is made. It remains the main solution for invasive forms of tumors.
The classification, localization, level of germination and degree of malignancy of the tumor determine the possibility of cure with preservation of the bladder and restoration of the functioning of the organ. A gentle approach, or partial removal of the bladder, is accompanied by a high risk of relapse and a rather low five-year survival rate.
An extremely accurate diagnosis is needed, with the exception of oat cell carcinoma.
After diagnosis, treatment should be prescribed only if an epithelial neoplasm is detected. First of all, treatment consists of various forms of surgery, radiation, and drug therapy.
At the same time, doctors try to choose the most optimal option that best contributes to the patient’s recovery. The reason is that in the case of growth of the tumor into the muscle layer, treatment is carried out fundamentally differently than in the case of its absence.
A favorable prognosis for bladder cancer is possible only at stage 1 or partially at stage 2. At the same time, surgical intervention significantly increases the patient's chances of five-year survival.
In patients with localized, superficially growing cancer, transurethral resection (TUR) of the bladder may be performed. TUR can be a radical intervention for stages T1-T2 of bladder cancer; with a widespread process (T3) it is carried out for palliative purposes.
During transurethral resection of the bladder, the tumor is removed using a resectoscope through the urethra. In the future, TUR of the bladder can be supplemented with local chemotherapy.
Open partial cystectomy of the bladder has been used less and less in recent years due to the high rate of relapses, complications and low survival.
In most cases of invasive bladder cancer, radical cystectomy is indicated. In radical cystectomy, the bladder is removed en bloc with the prostate gland and seminal vesicles in men; appendages and uterus in women. At the same time, part or all of the urethra and pelvic lymph nodes are removed.
The methods used in the treatment of bladder tumors depend on the nature of the tumor (malignant, benign) and location (invasive or papillary type). In almost all cases, surgical intervention takes place, which can be divided into the following types:
- TUR of bladder tumor.
- Open surgery to remove a piece of diseased tissue.
- Electrocoagulation of a non-invasive tumor.
- Radical cystectomy.
- Chemo and radiation therapy.
Transurethral resection is performed if a benign bladder tumor is diagnosed. The neoplasm is removed along with adjacent tissues to visually healthy boundaries. At the same time, tissue is collected for histological examination.
Important: When performing a TUR of the bladder, the probability of disease recurrence is more than 45%.
If a poorly differentiated invasive form of the tumor is diagnosed, removal of the bladder with external urine diversion or the creation of a container for accumulating fluid from a fragment of the rectum is indicated. Due to the fact that it is quite difficult to treat the tumor, plastic surgery is usually postponed, giving preference to the creation of percutaneous urinary drainage pathways.
If the images show that the tumor has grown into nearby tissues, they must also be removed, followed by a course of chemotherapy. Thus, treatment of a tumor in the bladder of men is often accompanied by removal of the prostate gland, and in women the urethra and uterus.
A course of chemotherapy and radiation therapy can be carried out before, after and instead of surgery, using intravesical or intravenous administration of drugs.
Bladder biopsy
A biopsy removes tissue from an internal organ to perform a microscopic examination. Bladder biopsy in women and men is performed using two main methods:
- The use of cold biopsy involves transurethral diagnosis, in which forceps with two-bladed spoons are used. Then, through a cystoscope, the doctor enters the bladder and performs an examination.
- A TUR biopsy of the bladder is performed by a surgeon and thus it is possible to accurately assess how deeply the malignant tumor has penetrated and spread. This procedure is both a diagnosis and a treatment method.
Prognosis and prevention of bladder cancer
A bladder tumor “finds soil” with bad habits: smoking, alcohol, as well as constant human contact with carcinogenic substances that are part of dyes and paints. Therefore, these harmful factors should be avoided.
Periodically, at least once a year, you need to undergo general medical examination and cancer screening.
For non-invasive bladder cancer, the 5-year survival rate is about 85%. The prognosis is much less favorable for invasively growing and recurrent tumors, as well as bladder cancer that gives distant metastases.
Quitting smoking, eliminating occupational hazards, drinking purified drinking water, and eliminating urostasis will help reduce the likelihood of developing bladder cancer. It is necessary to conduct a preventive ultrasound, urine examination, timely examination and treatment by a urologist (nephrologist) for symptoms of urinary tract dysfunction.
History taking and examination
A urologist interviews and examines a patient who suspects bladder disease, prescribing the required tests.
At the first visit, the doctor will interview the patient. In addition to a detailed description of the symptoms of the disease, it is important for the patient to remember when he first felt unwell and what type of pain he experienced. It is also important to mention the use of pharmaceuticals on the eve of the appearance of the deviation. People who have been exposed to cold and often experience stressful situations are in particular need of examination.
After receiving all the necessary information and interviewing the patient, the doctor prescribes a number of directions to accurately determine the location of the inflammatory process.
Predicting disease outcomes
The prognosis of the disease is completely determined by the classification, degree of differentiation of tumor cells and stage. The chance of recurrence increases with time after transurethral resection. In 60% of patients, the disease returns in the first 5 years after therapy and achieving remission.
If metastases are detected, the prognosis is unfavorable for ¾ of patients within 20 months. Local spread and the presence of metastases only in the lymph nodes gives hope for a five-year survival rate of 25%.
After cystectomy and proper treatment, the prognosis is relatively favorable: 5-year survival rate is about 80%.
- benign tumors have an almost 100% favorable prognosis;
- malignant tumors have a more complex five-year survival prognosis:
- initial stages 95%;
- Stage 1 about 70%;
- stage 2 64-65%;
- stage 3a about 50%;
- stage 3b about 30%;
- Stage 4 less than 28%.