17-ketosteroids
- compounds that are metabolic products of sex hormones from the steroid group, which are excreted through the kidneys and reflect the level of androgen production. A study of the amount of 17-CS in daily urine is performed together with tests for hormones in serum. The results are used in endocrinological, gynecological and andrological practice. They are diagnostically significant, as they allow one to assess the condition of the adrenal cortex, the secretion of steroid hormones in the male body, and identify pathologies of the reproductive system, disorders of puberty, and tumors. The biomaterial for analysis is a urine sample collected per day. The study of 17-KS in urine is carried out using ion exchange chromatography. The normal values for men are 10-25 mg/day, for women – 7-20 mg/day. The diagnostic period is up to 16 days.
17-ketosteroids
- compounds that are metabolic products of sex hormones from the steroid group, which are excreted through the kidneys and reflect the level of androgen production. A study of the amount of 17-CS in daily urine is performed together with tests for hormones in serum. The results are used in endocrinological, gynecological and andrological practice. They are diagnostically significant, as they allow one to assess the condition of the adrenal cortex, the secretion of steroid hormones in the male body, and identify pathologies of the reproductive system, disorders of puberty, and tumors. The biomaterial for analysis is a urine sample collected per day. The study of 17-KS in urine is carried out using ion exchange chromatography. The normal values for men are 10-25 mg/day, for women – 7-20 mg/day. The diagnostic period is up to 16 days.
17-ketosteroids are intermediate products of the transformation of steroids. In the body of women, the entire amount of 17-KS excreted in the urine is formed from androgens synthesized by the adrenal cortex. In men, about a third of these compounds are the result of the metabolism of hormones produced by the testes, the rest are formed from hormones of the adrenal cortex. Androgens break down and are converted into 17-ketosteroids and other final compounds in liver cells with the participation of glucuronide and sulfate. They are then excreted through the kidneys in the urine.
17-CS in urine are mostly DHEA or dehydroepiandrosterone and epiandrosterone. Both of these compounds are formed from hormones secreted by the adrenal glands. Other 17-ketosteroids include androsterone, androstenedione, etiocholanolone, epiandrosterone. In the absence of pathologies of the adrenal glands and testicles, the concentration of 17-KS in plasma and urine remains stable, despite the fact that hormones enter the blood unevenly depending on cyclical fluctuations in biological processes and changes in the concentration of other active compounds. When studying the level of 17-ketosteroids in urine, part of the biomaterial collected within 24 hours is examined. The analysis is performed by ion exchange chromatography. The results make it possible to assess the functioning of the adrenal cortex, as well as the male gonads, and are widely used in endocrinology, gynecology, andrology and reproductology.
Indications
In clinical practice, urine analysis for the content of 17-ketosteroids is used to assess the activity of the adrenal cortex and male gonads. The study is indicated for the diagnosis of congenital adrenal hyperplasia, polycystic ovary syndrome, Cushing's disease and syndrome, Addison's disease, hyperpituitarism. In addition, the analysis is prescribed to identify tumors of the adrenal glands, ovaries, testicles, and lungs. As part of a comprehensive examination, a test for KS-17 in urine is indicated for diseases accompanied by disorders of sexual development and reproductive function. For example, an analysis can be prescribed for female pseudohermaphroditism, genetic pathologies with a violation of the formation of gender characteristics, such as Klinefelter syndrome or Prader-Willi syndrome. The basis for conducting a test for 17-ketosteroids in urine may be a violation of reproductive function. The analysis is performed for patients with miscarriage, infertility, menstrual irregularities, and excessive development of male characteristics.
The level of 17-CS in urine is less susceptible to fluctuations than in plasma, which means it allows a more accurate assessment of the functioning of the adrenal cortex and gonads. For this reason, this analysis is more often used in medical practice, in particular when establishing the causes of infertility and miscarriage. A limitation of the study may be the need to collect 24-hour urine; the results are distorted if the requirements for this procedure are not met, as well as in some renal and hepatic pathologies. In some cases, testing for 17-ketosteroids in urine can be replaced by testing DHEA-SO4 in serum.
Analysis for 17-ketosteroids in urine
A urine test prescribed at CS 17 will help assess the degree of activity of male sex hormones. Androgens are synthesized in men and women and are responsible for many functions. Changing indicators is necessary to identify a number of endocrine disorders, causes of pathological pregnancy, and tumor-like formations of the endocrine glands.
Preparation for analysis and collection of material
Hemorrhoids kill the patient in 79% of cases
When performing a urine test for 17-ketosteroids, a portion of daily material is examined. 2 days before the start of collection, it is necessary to stop taking diuretics, 1 day before - to refrain from drinking alcohol, spicy foods, foods that change the color of urine: beets, carrots, berries, etc. In addition, during the day, urine collection should be avoided. heavy physical and psycho-emotional stress, maintain the usual drinking regime. Many medications can distort the test result by decreasing or increasing the concentration of 17-KS in the urine. Therefore, taking medications should be discussed with the doctor referring you for the study.
To collect urine, you need to prepare a sterile container with a lid with a volume of 2-3 liters. The first morning urination is skipped, but its timing must be noted. All subsequent urine samples must be collected within 24 hours. The last collection is the first urination the next morning. The container should be stored in the refrigerator without freezing throughout the day. Before sending to the laboratory, you need to determine the total volume of urine, and then separate a portion of 50-100 ml into a container. The daily urine output in ml should be noted on the label.
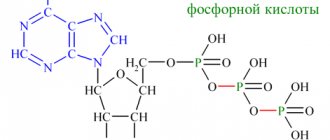
In the laboratory, determination of the level of 17-KS in urine is most often performed by ion exchange chromatography. This is a physicochemical research method based on ionic interactions - the analyzed molecules have a certain charge, which is opposite to the charge of the functional groups of the stationary phase (sorbent). During interaction, differently charged ions are attracted, the molecules under study are retained in the stationary phase, and then their number is determined. Preparation of research results takes from 8 to 16 days.
What hormone tests does an expectant mother need to take?
Estradiol
. This hormone is the most active female sex hormone. Outside of pregnancy, it is produced in the ovaries and adrenal glands, and during pregnancy - also in the placenta. Outside of pregnancy, the concentration of this hormone depends on the phase of the menstrual cycle; During pregnancy, its amount increases, reaching a “peak” before childbirth. We can say that estradiol is responsible for the normal course of pregnancy. The amount of estradiol returns to normal by the 4th day after birth. The functioning of the placenta is assessed by the concentration of estradiol during early pregnancy. A decrease in the amount of estradiol is determined when there is a threat of termination of pregnancy.
Progesterone
. A hormone necessary at all stages of pregnancy, which ensures its preservation. In particular, progesterone during pregnancy is “responsible” for the normal attachment of the fertilized egg to the uterus and for its development.
This hormone is also produced in the ovaries and adrenal cortex, during pregnancy - first in the mother's ovaries, and then by the placenta. Outside of pregnancy, its concentration also depends on the phase of the menstrual cycle. Throughout pregnancy, the amount of progesterone increases towards the 37-38th week. The amount of this hormone in a woman’s blood determines the condition of the placenta in the second half of pregnancy. A decrease in the amount of progesterone is observed when there is a threat of termination of pregnancy. In addition, this hormone helps determine post-term pregnancy.
Free estriol (EF)
. It is sometimes called the main estrogen (sex hormone) of pregnancy. Outside of pregnancy, there is very little of it in a woman’s body. Since it is produced by the placenta, during pregnancy, when the placenta begins to mature, the amount of this hormone increases sharply. Estriol increases blood flow through the vessels of the uterus, and also promotes the development of the mammary gland duct system during pregnancy. With the development of a pathological condition, the amount of the hormone changes before symptoms appear. Therefore, the concentration of this hormone in the blood is used to assess the state of blood flow in the placenta, umbilical cord (for a period of 12-15 weeks), as well as the formation of the placenta. Attention is paid to the concentration of the hormone if a post-term pregnancy or delayed fetal development is suspected.
Alpha fetoprotein (AFP)
. One of the main hormones, the concentration of which determines the development of the fetus. This hormone is produced not by the woman’s body, but by the growing body of the fetus. The hormone enters the mother's body through the placenta. Its greatest amount in the fetus is observed at 12-16 weeks of pregnancy, then the amount of the hormone decreases and by the end of pregnancy it becomes the same as in an adult. In a pregnant woman, the concentration of the hormone in the blood begins to increase from the 10th week, and decrease from the 34th week. The amount of hormone in combination with other studies reveals possible fetal malformations.
Human chorionic gonadotropin (hCG), a specific pregnancy hormone
. This hormone appears in a woman’s blood within a week after fertilization, and in the urine 1-2 days later. HCG during pregnancy stimulates the production of other hormones necessary for its maintenance and development. The maximum concentration of the hormone occurs in the 10-11th week of pregnancy, and its concentration increases proportionally depending on the number of fetuses. Then the concentration of the hormone decreases. It is on the determination of this hormone that a home rapid pregnancy test is based. The second strip of the test system is colored when a sufficient amount of hCG accumulates. Different test systems have different sensitivity to the hormone, so some tests can determine pregnancy even before a delay, others - after several days of a delay in menstruation. In combination with other hormones (AFP and estriol), the level of concentration of this hubbub during pregnancy evaluates possible deviations in the development of the fetus. At the same time, trouble can be thought of both with an increase and a decrease in the content of the hormone in the blood. In the early stages, the amount of the hormone indicates the duration of pregnancy.
As already noted, the three hormones listed above are part of the triple test, which is carried out at 16-20 weeks of pregnancy to identify genetic pathology in the fetus.
Urinalysis for 17-ketosteroids (17-KS)
. 17-KS is a “processing product” of male sex hormones. By the amount of this substance in the urine, one can indirectly judge the amount of male sex hormones in the body. The most common condition in which the amount of 17-CS in the urine is increased is adrenogenital syndrome. Normally, male sexual hormones in a woman’s body are processed in the adrenal glands into female hormones. In the absence of one of the intermediaries of this processing, the amount of male sex hormones increases. Their increased concentration can lead to miscarriages or intrauterine fetal death, so it is important to promptly identify and eliminate this problem with the help of special medications.
Dehydroepiandrosterone sulfate (DEA-SO4)
. An analysis for the detection of this hormone is currently used instead of a urine test for 17-KS. This analysis is more accurate; it can be used to judge how much androgens are produced in the adrenal glands. During pregnancy, the concentration of this hormone in a woman's blood decreases. This is what is assessed if there is a suspicion of growth retardation (hypotrophy) of the fetus. Based on the results of the analysis, the state of the fetoplacental complex (function of the placenta, blood flow in the umbilical cord) is also assessed, starting from the 12-15th weeks of pregnancy.
Sex hormone binding globulin (SHBG)
. This protein is produced in the human liver. With a decrease in its amount in the blood, the activity of sex hormones increases, and male hormones (testosterone) are stronger. At the end of the third trimester of pregnancy, SHBG levels increase significantly; Accordingly, the activity of sex hormones decreases. With a large amount of male sex hormones, the level of SHBG will be significantly lower, since male hormones inhibit the formation of SHBG. The level of SHBG during pregnancy determines the presence of adrenogenital syndrome1 and the possibility of developing preeclampsia2.
1Adrenogenital syndrome is characterized by an increased content of male sex hormones-androgens in the body due to their production in the adrenal glands. During pregnancy, this condition leads to the threat of miscarriage. 2Preeclampsia is a series of pathological conditions that most often manifest themselves as edema, increased blood pressure, and the appearance of protein in the urine.
Testosterone
. A male sex hormone that is normally present in women, but in much smaller quantities. During pregnancy, the amount of testosterone increases by the third trimester of pregnancy, exceeding its concentration in a non-pregnant woman by almost 3 times. The amount of testosterone determines the presence of adrenogenital syndrome. A change in the amount of this hormone in a pregnant woman's blood may also indicate that the woman is fasting, following a low-fat diet, or is a vegetarian.
Prolactin
. This hormone is also produced in the brain by the pituitary gland. It stimulates the development of mammary glands and milk production, regulates calcium absorption, but it retains fluid and sodium. This hormone is also responsible for the formation of sexual behavior. The amount of prolactin is highly subject to daily fluctuations and depends on the stress experienced and the phase of the menstrual cycle. It also changes during pregnancy, increasing from the 8th week and decreasing from the 20-25th week. An increase in the amount of the hormone is observed after childbirth, when active lactation begins. During pregnancy, the level of prolactin is used to judge the functioning of the fetoplacental complex and the presence of a true post-term pregnancy.
In pregnant women with diabetes, attention is also paid to the amount of C-peptide, which is part of the hormone insulin. Its level is used to judge the amount of insulin produced, assessing the possibility of developing pathology in the fetus.
Thyroid hormones (T3, T4), thyroid-stimulating hormone of the pituitary gland (TSH)
. Throughout a person’s life, normal levels of thyroid hormones are a necessary condition for the harmonious functioning of the body. They influence metabolic processes in the body, growth and differentiation of tissues, stimulate protein synthesis, influence sexual development, menstrual function, ovulation (the release of an egg from the ovary), which precedes fertilization. Decreased thyroid function (hypothyroid state) increases the likelihood of miscarriage and stillbirth.
Normal values
The concentration of 17-ketosteroids in urine depends on age, as well as gender. Reference values for children under 5 years old – 0-2 mg/day, from 5 to 9 years old – 0-3 mg/day, from 9 to 12 years old – 1-5 mg/day, from 12 to 14 years old – 1-6 mg/day With the onset of puberty, differences in the level of 17-KS concentration in urine between men and women become significant. So, for boys from 14 to 16 years old the norm is 3-13 mg/day, for girls of the same age - 2-8 mg/day, for men from 16 years old - 10-25 mg/day, for women - 7-20 mg/day A physiological increase in indicators is determined in the third trimester of pregnancy, in people who are overweight, and also after physical or emotional stress. A slight decrease in the concentration of 17-KS in urine is possible during menopause.
Decoding
Only a qualified physician should decipher the result of urine test 17 KS. The normal content of ketosteroids in urine varies and depends not only on gender, but also on the age of the patient. This study is often prescribed to children and adolescents.
In a healthy patient under 9 years of age, the norm is 17 KS - up to 3 mg/day. This figure gradually increases with age. In adolescents, the norm is 2-13 mg/day, and in adult patients – 7-25 mg/day. Only a doctor can identify a deviation from the norm after a preliminary examination of the patient’s medical record.
Quite often, after studying the results of a 17 Ks urine test, it turns out that the patient has an increased concentration of ketosteroids. The reasons for such a deviation may be:
- The appearance of neoplasms producing androgens and ACTH;
- Tumor growths on the adrenal cortex;
- Congenital pathologies of the adrenal glands of the virile type;
- Polycystic formations on the ovaries;
- Neoplasms on the gonads in men;
- Long-term use of medications of the cephalosporin group (Ketoprofen, Dexamethasone, etc.).
There are also relatively harmless reasons for the development of such a disorder. For example, high concentrations of 17 CS are observed in overweight people or patients who have experienced severe and prolonged stress.
Insufficient levels of male sex hormone in urine are also considered a sign of a pathological disorder. The reason for this analysis result can be considered:
- Addison's disease;
- Improper functioning of the hypothalamus;
- Hypogonadism in the fair sex;
- Pathologies in the functioning of the thyroid gland;
- Kidney disease, organ prolapse;
- Disease of the reproductive gland in men, which leads to reproductive disorders;
- Long-term use of hormonal contraceptive pills.
Many doctors recommend that patients study steroid hormones through a 24-hour urine test rather than a blood test. In this liquid, the concentration of CS is much higher, which means deviations from the norm can be easily detected.
Level up
The cause of a pronounced increase in the level of 17-KS in the urine is often adrenal hyperplasia. With this disease, the production of hormones increases, which is manifested by reproductive dysfunction, increased hair growth in the groin and armpits, hirsutism and some other symptoms. Another reason for a sharp and pronounced increase in the level of 17-ketosteroids in the urine are benign and malignant neoplasms of the adrenal glands, testes, ovaries, as well as tumors with ectopic production of adrenocorticotropic hormone, for example those localized in the lungs. Among other diseases that can lead to an increase in the concentration of 17-CS in the urine, it is worth noting Stein-Leventhal syndrome, hypercortisolism, female pseudohermaphroditism, and hyperpituitarism. A temporary increase in indicators is possible due to surgical interventions, major injuries, infections, as well as taking certain antibiotics, hormonal drugs, and ascorbic acid.
When should I take it?
A test to assess the level of 17 CS in urine is taken to confirm the appearance of a neoplasm of the endocrine glands or adrenogenital syndrome, and for a comprehensive assessment of the activity of the endocrine apparatus. The study is also carried out if:
- cases of distorted puberty;
- reproductive dysfunctions;
- pronounced male sexual characteristics in women;
- frequent spontaneous miscarriages, intrauterine deaths, infertility, menstrual irregularities.
Return to contents
Level reduction
The reason for the decrease in the level of 17-ketosteroids in the urine is often endocrine pathologies, accompanied by a decrease in hormone production. A decrease in the concentration of 17-KS in the urine is determined in severe forms of hypothyroidism, Addison's disease - decreased adrenal function, hypopituitarism - decreased pituitary function, primary hypogonadism in men - decreased testicular function due to genetic pathology or castration. Other reasons for a decrease in the level of 17-ketosteroids in the urine may be liver diseases, in which the processes of hormone breakdown are disrupted, and kidney diseases with damage to the renal tubules (nephrosis). Among medications, corticosteroids, estrogens, oral contraceptives, and penicillin can lead to a decrease in test results.
What do 17 KS show?
The study of the steroid profile shows the exchange of male sex hormones synthesized in the gonads of men and the adrenal cortex in women. Biologically active metabolites are excreted in the urine. The test is most often prescribed by endocrinologists, less often by gynecologists and oncologists, to calculate the correct functioning of the adrenal cortex, identify endocrine dysfunctions and factors affecting infertility.
The urine steroid profile includes determination of the concentrations of etiocholanolone, androstenedione, dehydroepiandrosterone, androsterone and epiandrosterone.
Treatment of abnormalities
Analysis for the determination of KS-17 in urine is one of the most popular tests in diagnosing pathologies of the adrenal cortex, testicles, ovaries, as well as in establishing the causes of infertility and miscarriage. If the results of the study do not correspond to the norm, then you should contact an endocrinologist, gynecologist or andrologist to prescribe treatment. To avoid distortion of indicators when studying 17-ketosteroids in urine, it is necessary to adhere to the requirements for collecting biomaterial - eliminate the influence of physical and psychological stress, and, if necessary, stop taking medications.
What is the preparation and how to pass?
Before taking the test, you must adhere to a dietary diet.
Preparation includes following a diet for 3 days before urine collection. Alcoholic drinks, fatty and spicy foods, brightly colored foods (carrots, tomatoes, oranges, beets) are excluded. The level of mental and physical stress should be reduced as much as possible, including intense sports training. Smoking is prohibited. If you are taking medications, you should stop using them or warn your doctor and laboratory technician. Urine is collected over a 24-hour period. The substrate should be stored in the refrigerator, and before submitting for testing, the volume is mixed and about 100 ml is taken into a sterile container. The amount of urine excreted per day is measured and recorded.
Return to contents
17-KS above normal
- Neoplasms of endocrine organs: adrenal cancer, ACTH-producing tumors, testicular and ovarian tumors, arrhenoblastoma, etc.;
- Lungs' cancer;
- Cushing's syndrome (hypersecretion of adrenal hormones);
- Cushing's disease (with pituitary adenoma)
- Adrenal hyperplasia;
- Adrenogenital syndrome;
- Prolonged stress, depression;
- Polycystic ovary syndrome (dysfunction due to menstrual irregularities) and related syndromes (Stein-Leventhal);
- Hyperpituitarism (increased function of the hypothalamus and adrenal gland, which leads to overproduction of adrenocorticotropic hormone, gonadotropin);
- Pseudohermaphroditism in women (development of the male genital organs in the presence of the female reproductive system);
- Hirsutism (male pattern hair growth);
- Last trimester of pregnancy;
- Obesity of all types;
- Recent surgeries, injuries, generalized burns, infectious diseases, etc.
- Taking medications: ampicillin,
- ascorbic acid,
- hydralazine,
- dexamethasone,
- digitoxin,
- corticotropin,
- ketoprofen,
- cortisol,
- meprobamate,
- methicillin,
- morphine,
- nalidixic acid,
- oxacillin,
- piperidine,
- penicillin,
- salicylates,
- secobarbital,
- spironolactone,
- testosterone,
- phenazopyridine,
- phenothiazine,
- quinidine,
- quinine,
- chloramphenicol,
- chlordiazepoxide,
- chlorpromazine,
- cephalosporins,
- erythromycin.
Norms for steroid hormone concentrations in women
The content of steroids in the blood and urine of women varies individually and depends on age, weight, phase of the menstrual cycle, and lifestyle. The norm in women from 20 to 60 years of age for DHEA sulfate is constantly decreasing, as is the content of other hormones.
| Table of average norms for androgen concentrations in the blood of women | |||||
| Androgen | Norm | ||||
| Up to 30 years old | 30–40 years | 40–50 years | 50–60 years | After 60 years | |
| DHEA-S, µmol/l | 2,40–14,50 | 1,80–9,70 | 0,66–7,20 | 0,94–3,30 | 0,09–3,70 |
| Androstenedione glucuronide, nmol/l | 0,73–10,75 | 1,26–6,30 | |||
| Testosterone, nmol/l | General: 0.31–3.78 Free: 0–4.2 | General: 0.42–4.51 Free: 0.1–1.7 | |||
| DHT, pg/ml | 24–450 | 10–181 | |||
Norms for urine steroid profile obtained by chromatographic method:
| Hormone | Norm |
| Androstenedione, mcg/day | 10–60 |
| DHEA-S, mg/day | Up to 1,497 |
| Epiandrosterone, mcg/day | 0,9–1,5 |
| Androsterone, mg/day | 0,3–3 |
| Etiocholanolone, mg/day | 0, 87–4,292 |
The indicator norms are indicated in the analysis results form in a separate column. Values may vary from laboratory to laboratory due to the use of different testing methods. The results of the analysis are interpreted by the attending physician. He may additionally recommend donating blood or urine for biochemistry, or undergoing an ultrasound of the adrenal glands or internal genital organs. After a full examination, an adequate diagnosis can be made and optimal treatment can be prescribed.
The biological role of steroids in the female body
Scientists have determined that androgens in women are not only precursors to estrogens. They perform a number of other important functions that are still not fully understood.
Among the functions of male steroids in the female body, it is worth highlighting the following:
- increased anabolism (synthesis) of proteins,
- reducing the concentration of glucose in the blood by increasing its utilization by cells,
- reduction in subcutaneous fat volume,
- increased libido.
Both a shortage and an excess of male steroids are equally harmful to a woman’s body. An androgen test allows for the timely detection of many functional disorders.
What hormones are classified as steroids?
Steroid hormones include hormones of the adrenal glands and sex glands. All of them are derivatives of cholesterol, the path of their formation is called steroidogenesis.
Sex hormones are divided into male (androgens) and female (estrogens). Each person has both types of biologically active molecules in their blood. Estrogens are derivatives of androgens. Their transformation occurs in the ovaries, and male hormones are produced by the adrenal cortex and adipose tissue.
In women, androgens are always present in small quantities in the blood and urine; this is a physiological norm.
In some diseases, this indicator is consistently exceeded or, conversely, reduced. Classification of male steroids:
- Testosterone is the leading sex hormone in all men; it is a prohormone; its active form is dihydrotestosterone (DHT).
- Androsterone is a metabolite of testosterone, with hormonal activity reduced by 7 times.
- Ethiocholanolone is an isomeric form of androsterone.
- Dehydroepiandrosterone (DHEA hormone), the main androgen of the adrenal glands, is a precursor of androstenedione, from which testosterone is formed. The hormone dihydroepiandrosterone is converted into sulfate – DHEA – SO4.
- Epiandrosterone is a metabolite of testosterone, practically devoid of hormonal activity.
The production of estrogen after menopause decreases sharply, and the decrease in the synthesis of testosterone and its metabolites occurs gradually. In a woman after 40 years, the concentration of hormones in the blood will be 50% less than in a girl.