Vesicoureteral reflux
The bladder is a muscular hollow organ designed to store urine before urination. Three openings open into the bladder - two connect to the ureters, one to the urethra. The ureters are funnel-shaped tubes that enter the bladder at an acute angle and are equipped with valves. The valve system is needed to prevent urine from flowing back into the ureter and kidneys.
Vesicoureteral reflux (VUR, ICD-10 code No. 13.7) is a pathology in which retrograde urine flow from the bladder back into the ureter is observed.
In people with this condition, the mechanism to protect against backflow of urine does not function, so it flows in two directions. The result is stretching and deformation of the ureters. If reflux becomes severe, urine leaks into the kidneys. In the vast majority of cases, VUR is observed in children; it is less common in adults.
Formation of vesicoureteral reflux
Methods of treating the disease and preventive measures
Bilateral vesicoureteral reflux in children is common due to the immaturity of some body systems. It is fraught with defective renal structures, increased systolic and diastolic pressure and the development of reflux nephropathy.
The main cause of this pathology is a weakening of the sphincter between the bladder and ureter. Under these conditions, the closure valve is unable to retain biological fluid in the bladder and throws it in the opposite direction.
Experts cannot identify a clear and decisive factor that provokes the development of the disease. However, there are a number of reasons contributing to PMR, which are divided into:
- Congenital. There may be incomplete maturation of the ureteric orifices or their abnormal location, bifurcation of the ureteral orifice, as well as incorrect location of the bladder.
- Purchased. The history shows inflammatory processes in the renal parenchyma and bladder.
The listed factors are dominant when detecting PMR in children. It is noteworthy that reflux is also diagnosed with an anatomically correctly developed vesicoureteral canal.
Urological pathologies are fraught with the development of unwanted complications that greatly affect the quality of human life. By following preventive measures, it is possible to significantly reduce the risk of serious consequences. All you need to do is adhere to hygiene rules and regular examinations to diagnose pathologies.
If, during diagnosis, a child is diagnosed with kidney reflux, it is necessary to undergo timely treatment. The treatment method will be selected individually, depending on the complexity of the pathology. If there are no severe complications in the child’s general condition, then treatment will be carried out on an outpatient basis. In case of severe complications, hospitalization in a hospital may be required.
In most cases, the use of drug therapy in combination with physiotherapeutic methods is sufficient. For congenital pathologies, surgical intervention is used more often than usual, but only if drug therapy has not brought a positive result.
Treatment methods
- medicinal – elimination of pain, treatment of concomitant diseases, elimination of emerging infectious conditions;
- surgical – the use of an endoscopic method to restore the ureteral valve.
Parents should not despair if their child has been diagnosed with this defect. This is a natural condition that many children outgrow. According to unofficial statistics, the treatment of reflux has a positive trend with the use of medications. And only in the most severe cases, we are talking about the possibility of surgical intervention.
To prevent reflux from occurring as a complication of urological diseases, parents need to take preventive measures. If the first symptoms of a malfunction of the urinary system occur, it is necessary to promptly seek help from specialists. The prescribed diagnostics will help to easily identify urological diseases. Treatment of pathologies at an early stage of the disease significantly reduces the risk of developing serious complications.
- compliance with personal hygiene rules;
- reduction in the development of viral diseases;
- timely diagnosis of diseases.
Urological diseases are very serious complications that can greatly affect a person's quality of life. Compliance with simple preventive measures significantly reduces the risk of developing serious complications.
In children, congenital pathology, as a rule, has no symptoms until it is complicated by an acute inflammatory process in the kidneys and bladder.
Symptoms that suggest vesicoureteral reflux in a child:
- recurrent diseases of the urogenital tract;
- in newborns: irritability, fever and lethargy;
- in older children: frequent urination, urinary incontinence and dysuria with fever.
Common symptoms include increased blood pressure, muscle aches, and weakness. In the case of chronic renal failure, signs of uremia are noted.
Epidemiology
Incidence: ~1% of newborns
Secondary PMR
Obstruction of the ureteral orifice leads to increased intravesical pressure and reflux of urine through the valve.
Conditions leading to the development of secondary VUR:
- incompetence of the posterior urethral valve,
- stricture;
- dysfunction of the bladder of the hypotonic type;
- neoplasms;
- BPH;
- deformation of the bladder due to compression by tumors of the pelvis and colon;
- impaired tissue elasticity due to cystitis;
- congenital pathologies of ureteral development: duplication and ectopia;
- ureterocele;
- iatrogenic damage;
- diverticulum
First of all, eliminate the reason why the urine has reverse flow.
Depending on the diagnosis, endoscopic and open surgical interventions are performed.
To suppress bacterial microflora, an antibiotic is prescribed taking into account sensitivity.
Conservative therapy is ineffective.
Victoria Mishina, urologist, medical columnist
The bladder is a muscular hollow organ designed to store urine before urination. Three openings open into the bladder - two connect to the ureters, one to the urethra. The ureters are funnel-shaped tubes that enter the bladder at an acute angle and are equipped with valves. The valve system is needed to prevent urine from flowing back into the ureter and kidneys.
Vesicoureteral reflux (VUR, ICD-10 code No. 13.7) is a pathology in which retrograde urine flow from the bladder back into the ureter is observed.
In people with this condition, the mechanism to protect against backflow of urine does not function, so it flows in two directions. The result is stretching and deformation of the ureters. If reflux becomes severe, urine leaks into the kidneys. In the vast majority of cases, VUR is observed in children; it is less common in adults.
DETAILS: Novikov Andrey Ivanovich urology
Formation of vesicoureteral reflux
Classification
The classification divides the disease into two forms:
- Primary PMR. It occurs against the background of congenital anomalies in the structure and functioning of the urinary system, and is associated with intrauterine disorders in the development of the ureteric orifice or bladder wall. Found in children.
- Secondary PMR. Develops due to chronic or acute diseases of the urinary system (usually due to cystitis), as well as after operations. It can occur at any age and is mainly diagnosed in adults.
Another classification identifies the following types of vesicoureteral reflux:
- Passive. Backflow of urine occurs between and during urination.
- Active. Urine reflux is observed only during urination.
In most cases, reflux in children is unilateral, but sometimes it occurs on both sides. In adults, bilateral VUR is also rare.
According to the time of occurrence of PMR, it can be as follows:
- Transitional. It develops only during exacerbation of other diseases of the urinary system (often in women - with cystitis, in men - with prostatitis).
- Constant. Always present, characteristic of childhood.
Based on the severity of the decline in renal function, the following degrees of the disease are distinguished:
- PMR 1st degree (moderate) – function drops by 30%.
- PMR stage 2 (moderate) – function decreases by 60%.
- PMR grade 3 (severe) – function decreases by more than 60%.
Clinical guidelines
Special documents developed by specialists in the field of urology clearly define the rules for conducting diagnostic and therapeutic measures.
According to these regulations, a child suffering from VUR is subject to hospitalization (while adult patients are treated in a laboratory). In addition, it is important to choose the right treatment tactics. Based on the severity of the disease and other conditions.
Vesicoureteral reflux in children - clinical recommendations.
Causes
In children, the primary forms of pathology are congenital. Various anomalies in the development of the nervous system and muscular membrane of the ureter are prerequisites for the appearance of VUR from birth.
The reasons are the following deviations:
- Duplication of the ureter.
- Dystopia of the ureteric orifice (the orifice is located below or above the area where it enters the bladder).
- The intravesical ureteric tunnel is too short.
- Persistent gaping of the ureteral opening in the bladder (it looks like a funnel).
- Protrusion of the bladder wall (paraurethral diverticulum) and incomplete closure of the ureteric orifice.
All these anomalies in children lead to the early development of ureteral sphincter incompetence and the appearance of VUR. If they are mild, reflux may occur later, during adolescence.
In addition to these prerequisites, a disease of nervous etiology – an overactive bladder – can cause PMR in children.
In adults, the causes of the disease almost always lie in previous genitourinary pathologies. In men, the cause may be prostate adenoma, a benign tumor that compresses the urethra. In women, PMR often develops against the background of chronic cystitis. Urolithiasis can cause reflux in both women and men, because regularly passing stones can injure the ureter and disrupt the transmission of nerve impulses to its valve.
Other possible causes for secondary vesicoureteral reflux:
- Obstruction of the urethra - its stricture (narrowing), tumor, cyst, proliferation of connective tissue in the urethral area.
- Sclerosis of the bladder neck with thickening of the wall in the area of the ureteric orifice.
- Shrinkage of the bladder.
- Surgeries on the ureters and bladder.
- Other dysfunctions of the urinary system.
Forms and degrees of VUR in children
The disease can be primary or secondary . The cause of primary VUR is a congenital defect of the ureteric orifice or bladder wall. A secondary disease is a continuation of diseases of the urinary system, for example recurrent cystitis.
Also, the disease can be permanent or transient. Permanent PMR is always present, while transient PMR appears in other diseases - acute prostatitis, cystitis.
PMR degrees
| Degree | Description |
| I | Reflux of small volume of urine is limited to the pelvic ureter, which is not dilated. There are no symptoms, the risk of complications is minimal. |
| II | Backflow of urine along the entire length of the ureter, but without its expansion. Urine does not reach the kidneys and pelvicalyceal system. There are no obvious symptoms, there is a small risk of infection, and reflux progresses quickly. |
| III | Urine enters the kidneys, but the pelvis does not dilate. Kidney function may be reduced by 20%. The ureter expands, urine stagnates in the excretory system, which increases the risk of infectious complications. Moderate symptoms appear. |
| IV | The ureter is significantly dilated, the pyelocaliceal region is deformed, kidney function is reduced by 50%, and less urine is produced. Symptoms are pronounced, body temperature rises, and swelling appears. If VUR is bilateral, life-threatening conditions may develop for the child. |
| V | All the signs of the previous stages are preserved, the kidneys are severely affected, their parenchyma is thinned. The ureter acquires knee-shaped bends. Symptoms of renal failure increase - nausea, vomiting, decreased urination, itching. |
Stages and symptoms
Vesicoureteral reflux can occur with varying degrees of severity.
Objective data, depending on the degree of the disease, will be as follows:
- First degree. The expansion of the ureter is not visible; urine flows into its pelvic part, and no further.
- Second degree. Urine reflux occurs along the entire length of the ureter.
- Third degree. As urine flows back, it reaches the pyelocaliceal apparatus of the kidney, and it expands.
- Fourth degree. Both the ureter and the renal pelvis are dilated and deformed against the background of VUR.
- Fifth degree. Kidney function begins to decline.
Stages of vesicoureteral reflux
The clinical picture of vesicoureteral reflux in children is as follows:
- Developmental delay by age;
- Low body weight, head circumference, height;
- Sick, pale appearance of the child;
- Frequent restlessness, crying;
- Abdominal pain up to colic.
Typically, such signs occur if the pathology remains untreated for a long time. Often, parents are forced to see a doctor by an acute condition - elevated body temperature, abdominal pain, malaise, urinary retention. It means the addition of an infectious process - cystitis, pyelonephritis. During an examination in the hospital, the baby is diagnosed with VUR, if this was not done during a routine examination at 1 month.
In adults, specific symptoms of PMR have not been described. All of them are layered with signs of chronic or acute diseases of the urinary system.
The components of the clinical picture of vesicoureteral reflux in adults include:
- Increased body temperature (up to 39 degrees in case of acute illness or up to 37.2-37.5 with prolonged subfebrile condition);
- Aching pain in the lower abdomen and in the projection of the kidney;
- Bloody discharge in the urine;
- Frequent urge to urinate;
- Feeling of fullness in the bladder;
- Edema;
- Thirst.
With a long course of PMR, it leads to weakness, headaches, and chronic high blood pressure. Some people have dark spots, spots before their eyes, dizziness, and even fainting.
In the video about the causes, symptoms and diagnosis of vesicoureteral reflux:
Conservative methods of therapy
At the initial stages of the development of the disease, conservative treatment methods , in particular, taking medications prescribed by a doctor, following a special diet, and using traditional medicine recipes.
In addition, it is necessary to establish a bladder emptying routine (urination should occur every 2 hours).
Drugs for treatment
The tactics of drug treatment of the disease can be different , depending on the specific cause that provoked its development.
So, in most cases, of medications :
- Antibacterial agents to suppress the activity of pathogenic microflora if bacterial infection occurs.
- Antiseptics to prevent re-infection (prescribed after a course of antibiotic treatment).
- Silver solution, Chlorhexidine, Solcoseryl for administration into the bladder cavity.
- Medicines to lower blood pressure if the child has persistent hypertension.
- Antipyretics if hyperthermia occurs.
Traditional medicine
In addition to the main treatment, the use of time-tested folk recipes is often prescribed.
It is important to remember that they cannot be used as independent therapeutic measures, since such treatment will be ineffective.
It is known that many herbs (for example, chamomile, St. John's wort, coltsfoot) have a pronounced anti-inflammatory effect , so decoctions prepared on their basis help prevent the development of the inflammatory process that accompanies PMR.
It is also important to systematically strengthen the child’s body’s defenses in order to help him cope with the problem as quickly as possible. To do this, it is recommended to consume cranberries, lingonberries, and currants (both fresh and in the form of fruit drinks).
Diet therapy
There are no dietary restrictions in the early stages of the disease, however, if the disease progresses and leads to impaired renal function, certain rules must be followed .
In particular, they limit the amount of liquid the child consumes (this is not only water and drinks, but also liquid foods, for example, soups).
In addition, it is necessary to reduce the consumption of salt (avoid salty, pickled foods) and protein foods.
Diagnostics
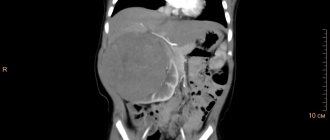
The most important method for diagnosing this pathology is cystography. During this procedure, a contrast agent is injected into the bladder through a catheter until the organ is filled. Then an x-ray is taken, the second one is taken directly during urination. This method allows not only to establish the type of PMR, but also to clarify its degree. Cystography also helps to identify the cause of reflux (for example, ureteral stricture, etc.).
Additionally, children and adults may be prescribed:
- Intravenous urography.
- Ultrasound of the kidneys and bladder.
- Cystoscopy.
- Scintigraphy or MRI.
- General urine analysis.
- Biochemistry of urine.
- Blood test for kidney parameters.
- Urine culture.
It is advisable to perform urine tests if an inflammatory process is suspected. Outside of inflammation, they do not show any abnormalities.
Treatment
At the initial stage, wait-and-see tactics are most often used. A sick child or adult is regularly examined by a urologist, and cystoscopy is performed to assess the dynamics of reflux. If the pathology progresses, surgery is usually recommended.
There are no special restrictions on diet and lifestyle, but if kidney function is impaired, you should follow a diet with limited fluid, salt, and protein.
Conservative treatment helps relieve inflammation and slow down the progression of pathology. For girls and women, treatment is carried out together with a gynecologist.
Medication
After a course of drug therapy, 70% of adults experience improvement. In children with primary VUR, this figure is lower.
Treatment may include the following types of drugs:
- Antibiotics - penicillins (Amoxiclav), cephalosporins (Cefuroxime, Cefixime).
- Uroantiseptics (after a course of antibiotics) – Nitrofurantoin, Nalidixic acid, Co-trimoxazole.
- Intravesical installations with silver solutions, Hydrocortisone, Solcoseryl, Chlorhexidine.
If the cause of vesicoureteral reflux in a child lies in a neurogenic (overactive) bladder, additional treatment methods are prescribed by a neurologist. In parallel with conservative therapy, the patient is recommended to undergo forced urination (every 2 hours), baths with sea salt, and electrophoresis. If hypertension develops, antihypertensive drugs are prescribed. Treatment in children is usually carried out in a hospital, in adults - on an outpatient basis.
Surgical
The operation is prescribed in the following cases:
- Lack of effect from medications and other types of conservative therapy.
- Serious decline in kidney function.
- 3-5 degree of vesicoureteral reflux.
- Frequent relapses of cystitis and pyelonephritis.
- Congenital anomalies of the structure of the urinary system.
The purpose of the operation is to eliminate the reverse reflux of urine by forming a new sphincter. There are several surgical and endoscopic techniques; the choice will depend entirely on the severity of the pathology, its form and the presence of additional anomalies and dysfunctions. Most often, a new valve is made in the form of a fold of the bladder, which will prevent urine from flowing back into the ureter.
Many experts consider the installation of an artificial valve to be the best method, but this operation has a high cost. Endoscopic correction is possible for grades 1-3 of VUR, taking into account the preservation of contractile activity of the ureteral orifice. Open operations are performed for grade 4-5 pathology and in the presence of severe anomalies in the structure of organs in children. Endoscopic injection correction of PMR:
Prevention
Preventing the occurrence of reflux in childhood is very problematic. Since the disease is congenital. But despite this, a number of specific recommendations can be identified, following which you can avoid the development of pathology:
- it is imperative to protect the child’s body from the occurrence of various types of inflammatory processes in the genitourinary system;
- if there is a possibility of such a disease, then you should adhere to a certain diet, which is drawn up directly with your doctor or nutritionist;
- If a child shows signs of urolithiasis, then it is necessary to immediately seek medical help to make a diagnosis and prescribe the necessary therapy.
By following certain rules, you can minimize the risk of developing this pathology. But if the disease is nevertheless diagnosed, then you should not panic, since today childhood vesicoureteral reflux is a completely curable disease. With timely diagnosis and professionally prescribed treatment, you can get rid of the pathology in a fairly short period of time without any harm to health. Treatment of the disease is currently carried out using several methods, as a result of which almost all patients completely get rid of the disease. Among other things, if you follow all the recommendations of your doctor, it is possible to prevent a relapse.
Prognosis and possible complications
Without treatment, a number of complications develop - acute and chronic pyelonephritis, hydronephrosis, urolithiasis, chronic renal failure. In children, PMR is the most common cause of secondary kidney shrinkage, impaired kidney function and the development of nephrosclerosis.
If the pathology is detected in a timely manner, the prognosis is positive. In 20-40% of children, the disease in its initial stages goes away on its own with age, but it can leave scar changes in the tissues. At 3 or more stages of PMR without treatment it threatens with the consequences described above. The operation gives excellent results - up to 75-98% of children and adults make a full recovery.