Irritable bladder syndrome (IBS) is a disease characterized by uncontrolled contraction of the muscle tissue of the organ, which causes increased urination.
Any person is susceptible to the syndrome, be it a child, an adult woman or a man.
In contact with
But mostly women are prone to the disease, because... their urinary system has clearer pathways for pathogens and germs.
Doctors say that the disease is often psychosomatic in nature rather than inflammatory in nature of the genitourinary system. This statement is explained by the fact that with frequent urges, neurosis develops.
Symptoms of the disease
First of all, irritable bladder syndrome is manifested by urinary incontinence and an increase in the number of acts of emptying the organ. It is complemented by pain, chronic inflammation of the bladder lining and neuropsychiatric problems. Symptoms that cannot be ignored include:
- nocturia – excessive urine discharge at night;
- feeling of bladder fullness;
- spasmodic pain accompanying the process of emptying;
- involuntary loss of urine due to sudden movements or sneezing.
The main task is to identify concomitant pathologies and organic lesions of the bladder, and the state of the microflora is also assessed. For this purpose, general clinical and instrumental examination methods are used, including:
- urine and blood analysis;
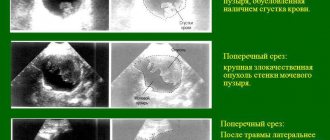
- Ultrasound of the abdominal organs;
- examination by a gynecologist and collection of biological material for bacteriological and cytological examination;
- cystoscopy is a diagnostic technique for visualizing an organ;
- X-ray;
- uroflowmetry;
- cystometry is a urodynamic study of the storage function of the bladder and the condition of the detrusor.
Due to the vague symptomatic picture, diagnosis presents certain difficulties and is based on clinical manifestations, nature and localization of pain. It is important to exclude from the anamnesis pathologies with similar symptoms, which include: urolithiasis, the presence of neoplasms, inflammatory processes and anatomical features of the structure of the organs of the urinary system.
Normally, a healthy person urinates 4-6 times a day. In some cases, an increase in frequency up to 7-8 times is allowed (but the latter happens rarely). The bladder can store up to 250 ml of liquid for 4-5 hours. Thus, a person has plenty of time to choose the right moment when he can go to the toilet.
Important! Irritable bladder syndrome (IBS) is most often not a disease, but just a symptom that can indicate a variety of pathologies.
It is necessary to distinguish SRMP from polyuria. In the first case, a person more often feels the urge to urinate, but the daily volume of urine remains normal (1-1.5 liters). In the second situation, the kidneys secrete up to 2-3 liters of urine per day or more.
The causes and treatment for this pathology can be completely different. More often, the etiological factor is mental, neurological, cancer, infectious diseases, and pathologies of the musculoskeletal system. Symptoms and treatment may vary in each case.
Causes of pathology
Depending on the causes, irritable bladder syndrome can be primary or secondary:
- Secondary. The pathology is caused by other diseases.
- Primary. The syndrome develops as an independent disease due to changes in the muscular wall of the bladder.
Secondary SRMP
There are many diseases that can lead to irritable bladder syndrome in women or men. Therefore, for convenience, they are divided into 3 groups: mental, neurogenic and others.
Mental causes - stress, psychosomatic pathologies, depressive states, neuroses. They lead to disruptions in the functioning of the autonomic nervous system, which is involved in regulating urination.
Neurogenic causes include Parkinson's disease and Alzheimer's disease, brain inflammation (meningitis, encephalitis), neuropathy resulting from diabetes, multiple sclerosis, and cancer. Various poisonings also lead to dysfunction of the bladder: alcohol, drugs, food.
This pathology can be a consequence of the development of tumors, obesity, muscle strain (during training), and surgical interventions. The syndrome also occurs with bladder cystitis, urolithiasis, prostatitis and other inflammatory or infectious pathologies of the urinary system.
Primary SRMP
Develops with age or with chronic urinary retention. During these processes, the blood supply to the muscular wall of the bladder is disrupted, which causes ischemia and, as a consequence, connective tissue dystrophy. All this leads to a decrease in the number of nerve endings of the postsynaptic cholinergic nervous system.
As a compensatory mechanism, increased sensitivity of muscle cells to acetylcholine (a chemical method of nerve stimulation) appears. In addition, the intercellular space decreases, due to which the myocyte membranes are in close contact. This condition is the cause of SRMP.
In such a situation, stretching of the bladder due to the accumulation of urine and irritation of its walls leads to a contraction of individual muscle fibers. This contraction stimulates neighboring myocytes. As a result, a cascade reaction is triggered, due to which the entire muscle wall contracts, which leads to urination.
Symptoms of SRMP
Irritable bladder syndrome is a complex of specific symptoms. Characteristic features:
- the desire to go to the toilet occurs 10-15 times a day;
- the daily amount of urine excreted remains normal;
- urination may occur uncontrollably;
- urges are spontaneous and occur abruptly;
- they are very strong, so that a person cannot stand it;
- urges interfere with sleep and force you to get up at night.
All these symptoms unambiguously indicate MSPS, but do not allow one to determine the underlying disease (the syndrome is not one).
| Diagnosis | Symptoms |
| Mental or neurological disorders | Panic attacks, pressing headaches, depression, irritability, severe fatigue, VSD disorders |
| Parkinson's disease | There is slight trembling, muscle rigidity, the person is not able to make precise movements, and remains in one position for a long time. |
| Alzheimer's disease | Violation of short-term and long-term memory, speech, consciousness, orientation. A person often does not understand what he is doing. |
| Meningitis | Headache, neck muscle spasms, fever, photophobia. |
| Encephalitis | Hyperthermia, headache, photophobia, nausea, epileptic seizures. |
| Multiple sclerosis | Uncontrollable or strong urge to urinate spontaneously. Incomplete emptying of the bladder, sexual dysfunction. |
| Alcohol intoxication | Headaches, dizziness, nausea. |
| Drug intoxication | Confusion, dry mucous membranes and skin. |
| Bladder cancer | Blood in urine. Incontinence gives way to urinary retention. Pain with frequent urination. |
| Cystitis | Strong and frequent urge. A feeling that the bladder is not completely emptied. Pain when urinating, which radiates to the rectum. When analyzing urine, red blood cells and protein are detected. |
| Prostatitis | General and local increase in body temperature, pain during bowel movements and urination, disturbances in urination. |
| Overactive bladder | Apart from frequent urination, there are no other manifestations. The urge occurs when palpating the lower abdomen, when bending backwards (from a standing position). |
The disease may be accompanied by depression, since frequent urination greatly deteriorates the quality of life. A person has problems at work, in the family, in relationships with other people. Patients usually have poor sleep due to nighttime urges.
Treatment methods
Symptomatic therapy for irritable bladder syndrome and treatment of the underlying disease are usually carried out.
An irritated bladder is treated mainly with medication; exercise and physiotherapeutic procedures are also recommended. Traditional methods of treatment are not recommended, since their clinical effectiveness has not been proven.
It is the main method of treatment. Medicines are used that eliminate uncontrolled contraction of the muscular wall of the bladder. In particular, this group includes anticholinergics (M-choline blockers), α-blockers, β-blockers.
From this list of drugs, anticholinergic drugs are primarily used for treatment. To eliminate mental disorders, sedatives and antidepressants are used.
Kegel exercise
This is a set of workouts to strengthen the pelvic muscles:
- They tighten the intimate muscles as if they are blocking urination. Hold them tense for 3 seconds, then relax them.
- Squeeze and release the pelvic floor muscles. The voltage is increased gradually. Each time the muscles are held for 3 seconds at the peak of the load.
- The same exercise, but squeezing and unclenching is done quickly, without delay.
- Lower abdominal tension.
Each exercise must be repeated 10 times. The whole complex must be performed 5 times a day.
A number of simple rules should be followed:
- You need to increase the amount of vegetables and fruits in your diet.
- It is advisable to eat oatmeal and buckwheat porridge more often.
- You cannot consume chocolate, coffee, or alcohol.
- You should not drink for several hours before bedtime.
- It is necessary to exclude from the diet foods that have a diuretic effect (rose hips, watermelon, juices).
Other treatment methods are also used:
- Electrical stimulation. It is used when the patient cannot perform Kegel exercises on his own.
- Establishing a urination routine. They go to the toilet strictly once every 2 hours. This is necessary to accustom the body to a certain regime.
- Operation. Used for bladder tumors and the need to change its volume. A complete organ replacement is also possible.
With secondary irritable bladder syndrome, how to treat the patient depends on the underlying disease. The decision about the type of therapy and the drugs used is made by the doctor. The most common treatment methods are:
- Mental disorders. Antidepressants, neuroleptics, sleeping pills, and sedatives can be used.
- Parkinson's disease. First of all, drug treatment is used with the use of anticholinergic drugs and dopaminergic drugs. In severe cases, surgery is recommended. Modern treatment methods include gene therapy.
- Alzheimer's disease. Cholinesterase inhibitors are used. Psychosocial training with a psychotherapist is widely used to help the patient adapt. Currently the disease is incurable.
- Meningitis. Particular attention is paid to antibiotic therapy, since the disease is often caused by bacteria. Anti-inflammatory drugs are used. Diuretics are used to reduce swelling.
- Encephalitis. Glucocorticoids are used to block the mechanism of disease development. Diuretics are used to reduce swelling. To eliminate the cause of the pathology and destroy the virus, the patient is given gamma globulins and immunoglobulins.
- Multiple sclerosis. For exacerbations, corticosteroids are used. Cytostatics are also prescribed. To slow down the development of the disease, interferons beta-1a are administered to the patient.
- Alcohol intoxication. First of all, detoxification therapy is carried out. Removing ethanol breakdown products from the body allows you to relieve headaches, dizziness and other symptoms of poisoning.
- Drug intoxication. The range of drugs used varies greatly depending on what drugs the patient was using.
- Bladder cancer. Depending on the type of tumor and stage of the disease, surgery, chemotherapy and radiation therapy are used. For large tumors that can grow into surrounding tissue, removal of the bladder is recommended.
- Cystitis. First of all, you need to exclude spicy and salty foods from your diet; diuretic decoctions of herbs are also used. To eliminate bladder spasms, antispasmodics are used.
- Prostatitis. Antibiotics and anti-inflammatory drugs are used. Antidepressants are prescribed to relieve stress and pain. To normalize urination, alpha-1-blockers are prescribed.
- Overactive bladder. Trospium chloride is the most popular and effective. Additionally, cholinergic drugs may be prescribed.
What are the symptoms of chronic cystitis and how to treat it?
Very often, chronic cystitis is detected in men and women in clinics across the country. This is a disease of a non-infectious or infectious nature, the symptoms, treatment and reviews of which are worth knowing in order to overcome the disease once and for all.
The chronic form of the disease most often occurs due to improper or untimely treatment of acute pathology. An inflammatory process gradually develops in the walls of the bladder and ureters, causing a lot of unpleasant symptoms. They can either fade or grow with renewed vigor, alternating a state of deterioration with periods of improvement.
Have you been fighting CYSTITIS for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure cystitis by taking it every day...
Read more "
How is cystitis classified?
The chronic form of the pathology has an ICD code of 10. Also, depending on the clinical picture, the following types of cystitis are distinguished:
- Interstitial nephritis (bladder syndrome) is a sluggish infectious process with minimal symptoms.
- Persistent is a disease with a wave-like character, when a period of remission is replaced by a sharp relapse.
- Latent - practically does not appear and does not particularly undermine health.
After a visual examination by a doctor and a comprehensive examination, the following type of cystitis can be identified:
- necrotic (organ tissues die);
- ulcerative (indentations form on damaged mucous membranes);
- polypous (papillae are formed on a thick or thin stalk, provoked by the papilloma virus);
- granular (granular rashes on the mucous membranes);
- cervical (the neck of the bladder becomes inflamed);
- infiltrative (allergic nature of the disease, when eosinophils and leukocytes accumulate on the mucous membrane);
- bullous (presence of pus and severe swelling of the mucous tissues);
- cystic (cysts of different sizes are formed, filled with fluid inside);
- catarrhal (mucous membranes swell, swell and turn red).
Only by determining the type of disease can the doctor prescribe the correct treatment, select good antibiotics and anti-inflammatory tablets.
From the very beginning, damage to the walls of the bladder occurs. In response, the immune system produces cells that provoke inflammatory reactions. Sensitive nerve endings are irritated, resulting in specific symptoms of the disease - itching, burning, pain. The permeability of vascular walls increases.
As a result, blood plasma enters the tissues and forms swelling and stagnation in the intercellular space. Sensitive nerve endings are compressed due to swelling, and the symptoms of the disease intensify.
Causes of chronic cystitis in women
Most often, urological problems occur in representatives of the weaker half of humanity. Candida, ureaplasma, chlamydia, E. coli or other pathogens enter the urethral mucosa. They begin to actively multiply and penetrate the ureters and bladder.
Chronic or acute cystitis in women also occurs due to:
- Cervicitis of the cervix.
- Colpitis or candidiasis.
- Urethritis.
- Constipation.
- Urolithiasis.
- Pyelonephritis.
- Sexually transmitted diseases.
In mature women, complex pathology often develops due to hormonal imbalance, that is, as a result of insufficient estrogen production. The disease provokes any weakening of the immune system, for example, due to hypothermia, lack of vitamins and minerals. Age-related changes, disorders of the endocrine system and diabetes mellitus also play a role.
Pathogenic bacteria enter the genitourinary system due to failure to comply with basic rules of personal hygiene and wearing tight and uncomfortable underwear. They affect the bladder, uterus, vagina, and rectum. An important predetermining factor in the appearance of chronic cystitis is unprotected sex and frequent changes of sexual partners. The consequences of this are sometimes the most dire.
Causes of chronic cystitis in men
Most often, elderly people suffer from this urological pathology. It is caused by serious internal pathologies, for example, prostatitis, adenoma, cancerous tumors of the pelvic organs, and the formation of large stones in the kidneys.
Most often, in men with inflammation of the prostate, incomplete emptying of urine occurs, and an infectious process begins in the urethra. Bacterial flora can also affect neighboring organs, so it is necessary to carry out therapy in a timely manner.
Symptoms in men and women
Common manifestations of both chronic and acute inflammation of the urinary system include:
- frequent urge to urinate (more than 10 times a day);
- burning, discomfort and pain when passing urine;
- intermittent urine flow, passing in small portions;
- pulling and painful sensations in the lower abdomen and lower back;
- bloody or mucous discharge in the urine, sometimes with an unpleasant odor;
- hyperthermia (up to 37-38 degrees).
Often recurrent cystitis is also characterized by general weakness and increased fatigue. Psychosomatics can also be involved - nervousness, increased excitability, decreased performance or, conversely, apathy and fatigue. Such signs should be a reason to immediately consult a doctor, as should lack of appetite, muscle and joint pain, and migraines.
In men, cystitis manifests itself almost equally in both the elderly and the young. Due to a violation of the outflow of urine and an old infection, problems with potency begin. It weakens or is completely absent during the period when there is an exacerbation.
Diagnostics
An experienced doctor, suspecting chronic inflammation in the genitourinary system, will prescribe a number of laboratory and clinical tests:
- Smear from the urethra and vagina.
- Culture and general urine analysis.
- Ultrasound of the pelvic organs.
- General and detailed blood test.
- Ultrasonography.
- Cystoscopy.
The last study is carried out using a cystoscope. It displays the status of the bladder and urethra on the monitor. It is used to determine the degree of tissue damage.
First of all, when a sexually transmitted infection is detected, PCR diagnostics are performed in order to more accurately determine which pathogen caused the disease and select the most effective drugs against it.
If the medical history is such that it was caused by viruses, then a different, not antibacterial, but antiviral therapy is selected. Clinical recommendations depend on the type of pathogen, the nature of the infection and the presence of certain symptoms.
Complex therapy of chronic cystitis
Treatment of urological pathology must be carried out at any stage. It is selected only by an experienced doctor based on a thorough diagnosis. It is almost impossible to restore the bladder mucosa with cystitis on your own and at home, and uncontrolled use of antibiotics only aggravates the situation, as do untested folk methods.
To cure chronic cystitis forever, use the following medications:
- antibiotics (up to 2 weeks);
- nitrofurans (up to several months);
- antiviral agents;
- immunomodulators (Wobenzym);
- antimicrobial drugs.
Physiotherapy and proper diet have worked well. Standards of treatment include vitamin and mineral supplements. In serious situations, for example, in the presence of necrosis, polyps, large cysts, surgical intervention will be required to cure the disease and prevent its recurrence.
Ketoconazole, Fluconazole and other antimycotic drugs are prescribed if chronic cystitis is caused by pathogenic fungal spores. If tests show that trichomoniasis is raging in the body, antiprotozoal medications with powerful antimicrobial properties are prescribed.
Antihistamine drops and syrups are also included in complex treatment if the pathological process provokes rashes on the body. The standard regimen is supplemented with diuretics to quickly remove all dangerous microflora from the urinary tract. Protracted pathology sometimes requires repeated treatment and prevention several times a year.
To treat cystitis, our readers successfully use Galina Savina’s method
This cheap odorous remedy will get rid of cystitis forever! Sold in every pharmacy, called...
If fever is present, antipyretic drugs are indicated. In a hospital setting, saline solutions are administered intravenously to get rid of intoxication. Blood supply to tissues and their healing are accelerated by venotonic drugs. They normalize the functioning of blood vessels in the pelvis.
For men suffering from cystitis, prostatitis or BPH (benign prostatic hyperplasia), it is important to use suppositories, gels and tablets that relieve the symptoms of prostate inflammation, for example, the Vitaprost complex. For women during menopause, to prevent a recurrence of a chronic disease, estrogen tablets are indicated. Reviews from doctors and patients about them are the most positive.
What antibiotics are used?
In most situations, chronic cystitis is treated with antibacterial medications. They are selected for a specific pathogen:
- Palin.
- Amoxiclav.
- Rulid.
- Nomitsin.
- Erythromycin.
- Nitroxoline.
- Furamag.
- Levomycetin.
- Monural.
- Ofloxacin.
- Norbactin.
- Ciprofloxacin.
These drugs quickly remove pathogenic microflora in the genitourinary organs, but they are contraindicated if cystitis has developed in a child. The treatment regimen for pregnant women is also selected individually. In parallel with the use of antibiotics, drugs with bifidobacteria are prescribed, which protect the gastrointestinal tract from dysbacteriosis. For a lasting therapeutic effect, antibacterial agents are changed every 5-7 days.
To normalize kidney function and urine outflow, the standard regimen is supplemented with Furagin, Cyston, Canephron, Monural. The modern drug Urovaxone has a good anti-inflammatory and diuretic effect. To get rid of pain and relieve inflammation of the gallbladder, drugs with analgesic and decongestant effects are used.
Additional Treatments
Chronic cystitis is dangerous due to its consequences. As additional methods of treating it, experienced urologists offer:
- ozokerite therapy;
- physiotherapy;
- microenemas;
- mud applications;
- paraffin therapy;
- acupuncture;
- iontophoresis;
- sea baths;
- therapeutic exercises;
- hydrogen sulfide or chloride baths.
Physiotherapy procedures have a quick therapeutic result, which allows the therapeutic components to penetrate faster into the foci of infection. This can be UHF or electrophoresis, which improve blood microcirculation in the peritoneal organs and accelerate tissue regeneration. Special gymnastics helps restore the function of the genitourinary system. It tones the entire body and strengthens the immune system.
Special diet for prolonged cystitis
When diagnosing chronic bladder inflammation, it is important to eat properly and include the following foods in your diet:
- Olive oil.
- Lean fish and meat.
- Natural honey or propolis.
- Mumiyo.
- Whole grain cereals.
- Lingonberries and cranberries.
- Dairy products.
- Unsweetened fruits and fresh vegetables.
- Herbs with a diuretic effect.
A special diet helps improve digestion and relieve inflammation, normalize the flow of bile and urine, and remove toxic compounds. Doctors recommend that all patients with cystitis adhere to the drinking regime, and also exclude pickles, marinades, spices, smoked meats, and coffee from the menu.
Video: cystitis.
Herbal medicine against bladder inflammation
If nothing helps against cystitis, it is worth trying recipes used by traditional healers for centuries. Healing herbs help get rid of infection and normalize urination. This:
- fennel;
- horsetail;
- cowberry;
- celandine;
- St. John's wort;
- cornflower.
Decoctions and tinctures are prepared from them. Those who don’t have time choose ready-made herbal preparations - Canephron, Phytolysin. Such treatment methods are contraindicated if there is renal failure, pregnancy, cystitis in children under 10 years of age. In such situations, urology provides individual therapeutic regimens, developed jointly with a gynecologist and pediatrician.
Irritable bladder syndrome in women - symptoms
The main symptom of the disease is a violation of the frequency and act of urination. Women complain of a constant desire to empty the bladder. The number of urges per day can reach 8 times during the day and more than 2 times at night.
However, the diagnosis of irritable bladder cannot be made solely by the frequency of urination, the symptoms of which may include the following:
- sudden urge to urinate even with an empty bladder;
- development of urinary incontinence, discharge in small portions when laughing, sneezing;
- reducing the amount of urine excreted during one visit to the toilet.
To make a diagnosis, doctors perform a comprehensive diagnosis of the bladder. It all starts with taking an anamnesis. The doctor finds out information regarding the number of urinations per day, the volume of one portion of urine. To do this, the patient needs to carefully monitor herself for 3-4 days.
After this, to identify an irritated bladder in women, a laboratory and hardware examination is carried out, which includes:
- general blood analysis;
- general urine analysis;
- Ultrasound of the pelvic organs;
- determination of residual urine;
- urodynamic study.
The body produces about 2 liters of urine per day, this volume is consumed in a person as a result of 8 or less urinations. If you have to go to the toilet more than 10 times a day, then you have irritable bladder syndrome. The sick person develops such a strong desire to urinate immediately that if there is no toilet nearby, he is unable to hold in his urine.
Involuntary urination can begin with the sound of dripping water.
An indirect symptom can be a person’s lifestyle: he tries to leave the house less often or visit only those places where it is possible to quickly visit the toilet stall. Here are more symptoms of the disease:
- Inability to hold urine on the way to the toilet.
- Once urination has started, it cannot be stopped.
- When your bladder is full, you cannot start urinating.
- When trying to laugh, involuntary urination occurs.
- Urine is released when you hear the sound of water dripping from a faucet or the sound of rain.
- A small amount of urine is passed.
- Feeling of incomplete emptying of the bladder.
The clinical picture of irritable bladder syndrome makes it possible to differentiate it from infectious cystitis, accompanied by cutting pain when urinating.
Symptoms of irritable bladder in women:
- A sudden, frequent feeling of the need to urinate;
- Increased urge to urinate more than eight times a day and more than twice at night;
- An imperative urge to urinate – occurs when the bladder is not full;
- Urinary incontinence, etc.
These symptoms may be present in all or only a few. But not only these symptoms create the clinical picture of the disease. With irritable bladder syndrome, patients often experience sleep disturbances and a high incidence of depression. Often, inflammatory diseases of the genitourinary system are associated with a hyperreactive bladder. In any case, there is a need to consult a specialist with subsequent diagnosis and treatment of the condition.
Irritable bladder syndrome in women depresses them, they are embarrassed about their disease, do not tell their loved ones, and withdraw. If you contact a specialist, there are options for a complete cure or achieving control of the disease, which in any case is a good outcome for the patient.
A healthy urinary system works unnoticed: 4-8 times a day signals are sent to the brain about the need to empty the bladder. Up to 250 ml of urine accumulates there, but it can retain this liquid for 2-5 hours.
This time is enough to find the right moment and “relieve your need.” The situation is completely different with irritable bladder syndrome (IBS).
- The need for emptying occurs much more often (10-15 times);
- The attacks occur suddenly and with great force, so that it is impossible to endure;
- Urine may be released involuntarily, the process is uncontrollable;
- Unexpected attacks disrupt night sleep;
- During the day, the possibility of sudden attacks keeps you in constant tension, stress arises, and performance decreases.
The quality of life deteriorates sharply. Although the organs of the urinary system can be absolutely healthy and function normally. The kidneys filter the usual daily volume of urine (2 liters), the ureters have good patency, and the bladder itself is not inflamed or clogged with stones.
Where then do these sudden and painful attacks of urination come from? They are associated with overactivity of the muscles surrounding the walls of the bladder. This muscle layer is called the detrusor; under normal conditions, in response to a signal from the central nervous system, it contracts and compresses the bladder. The sphincter that holds urine, on the contrary, relaxes - the act of urination occurs.
In irritable bladder syndrome, the sphincter and detrusor receptors act spontaneously, not obeying brain signals. Irritation of the receptors is not associated with the accumulation of urine - with frequent emptying, very small portions are released.
The problem that defines irritable bladder syndrome is that the process of urination is out of the control of the central nervous system.
Reasons for deviations
There may be several reasons for unbalanced functioning of the urinary organs.
First.
Systemic, infectious diseases, changes in the body, which are accompanied by frequent and painful urination:
- Infections of the genitourinary organs, urolithiasis;
- Prostatitis;
- Tumors: benign and oncological;
- Changes in the pelvic organs associated with muscle strain (sports, heavy lifting), operations, progressive obesity;
- Old age: sprained ligaments and muscle fibers of the pelvic organs, hormonal changes cause urinary incontinence.
Second.
Neurogenic causes - pathologies of the central and autonomic nervous system:
- Parkinson's and Alzheimer's diseases, multiple sclerosis;
- Inflammation of the brain and spinal cord (meningitis, encephalitis);
- The effects of alcohol, drugs, strong medications;
- A complication of diabetes is diabetic neuropathy.
Third.
Irritable bladder syndrome as a psychosomatic disease.
As an independent disease not associated with other pathologies, MSPS is of a psychosomatic nature. The cause of such diseases is mental disorders, prolonged stress, depression, and traumatic situations.
They form neurosis - a pathology of the autonomic nervous system (ANS), which controls the functioning of internal organs. Their functions are disrupted, and a somatic (physical) disease occurs, which is based on a mental disorder.
Functional disorders of internal organs that have a mental cause are called organ neuroses. The signs of MSPS as an organ neurosis are characterized by:
- Chronic, persistent nature of attacks;
- Cystolgia (a complex of causes characteristic of cystitis) - a feeling of pain in the urinary organs, a strong urge to urinate, a feeling of incomplete emptying of the bladder, a small amount of urine excreted;
- Nervous excitability, depression, insomnia, etc.
- The presence of concomitant neurosis of another internal organ (irritable bowel syndrome)
Signs of irritable bladder syndrome in women are many times more common, especially during menopause.
Attempts to heal on your own are unsuccessful. It is impossible to get rid of a disease whose causes are unknown. The most practical solution is to make an appointment with a urologist and establish a diagnosis of your disease.
Diagnosis of SRMP
Diagnosing irritable bladder syndrome is not easy. The patient will undergo a number of studies.
Anamnesis - survey.
During which the possibility of underlying diseases of a systemic and neurogenic nature, which can provoke frequent urination, is established. In addition, you will have to answer in detail:
- Under what circumstances do seizures most often occur?
- What kind of liquid and in what quantity does the patient consume;
- Is the volume of liquid drunk comparable to the amount of urine excreted?
Visual inspection.
To exclude pathologies of the genital area, women are examined by a gynecologist, and men are prescribed a prostate examination.
Conducted: general blood and urine analysis.
To exclude infectious diseases; cytological examination of urine (whether there are cancer cells); biochemical tests for the presence of sexually transmitted infections.
Uroflowmetry and cytometry.
The functional state of the detrusor is checked using uroflowmetry (speed and volume of urination) and cytometry (measuring the pressure of urine flow using a catheter).
Ultrasound of the pelvic organs.
Determines the presence or absence of tumors. Computed tomography is sometimes used to clarify the diagnosis.
Only after excluding infections and inflammations (especially cystitis), urolithiasis and tumors does the urologist make an assumption about irritable bladder syndrome.
For neuroses of internal organs, consultation with a psychotherapist is mandatory. Only it will help overcome mental disorders that cause organ dysfunction.
- First of all, drugs that block involuntary contraction of the detrusor muscles are used for the treatment of MSPS: M-choline blockers, alpha1-blockers;
- Botulinum toxin successfully treats this neurosis. 20-30 Botox injections into the bladder wall cause a decrease in muscle tone for up to a year. During this time, training and special exercises can restore the normal rhythm of urination;
- Taking sedatives is necessary to relieve the negative effects of stress.
Kegel exercises
An effective set of 4 exercises strengthens the pelvic muscles.
- Tension of the bladder muscles is an imitation of stopping urination. The state of tension is delayed by slowly counting to three, then the muscles relax;
- Gradual tension of the pelvic floor muscles: first light, then stronger, and finally maximum. At each stage, the position is fixed and delayed. Then the same gradual relaxation is performed;
- Fast and strong movements to tense and relax the pelvic muscles;
- Imitating attempts to push.
Treatment methods
Additional signs of the disease
The signs of the presented syndrome are very similar to the symptoms of cystitis in acute and chronic forms, especially when it comes to an infectious nature.
In this regard, it is very important to diagnose these diseases at the initial stage, because this is what will prevent the spread of infectious lesions and serious damage to the internal organs.
An indirect manifestation may well be a person’s lifestyle, as a result of which he tries to leave the apartment less often or stay exclusively in such premises or locations where he can easily visit the toilet room.
At this stage of the disease, a person is tormented by such manifestations as the inability to hold urine, for example, on the way to the toilet.
Irritable bladder syndrome is characterized by the following symptoms of the disease:
- the beginning of spontaneous urination when laughing;
- discharge of urine with the echo of a falling drop of water from a tap or with a drop or the sound of rain;
- a feeling of pain in the area of the irritated organ, causing psychological problems.
Taking all this into account, experts emphasize that in the case of irritable bladder syndrome and symptoms, treatment should begin as early as possible. This is what will allow you to avoid the development of complications and critical consequences.
Diagnostics: examination and tests
A patient's visit to a specialist involves collecting complaints, a history of life and illness, and gives the doctor the opportunity to decide on the need for prescriptions and what additional research methods to use. The need for laboratory and instrumental tests is associated not only with diagnostic criteria, but also to exclude diseases that cause the clinical picture of irritable bladder in women and are life-threatening.
Laboratory research methods include a general clinical analysis of blood and urine, a biochemical study (creatinine, urea, uric acid, etc.), urine analysis according to Zimnitsky, Nechiporenko, Rehberg test, etc.
Instrumental diagnostic methods, the need for which arises in case of hyperreactive bladder syndrome:
- Ultrasound examination of the abdominal organs, retroperitoneal space and pelvis;
- Magnetic resonance imaging;
- CT scan;
- Electromyography, etc.
An exact plan of diagnostic measures can be drawn up during a consultation with a specialist at the Yusupov Hospital, which you can sign up for by phone or online.
When contacting a doctor, you must provide a medical card with a list of possible diseases in your medical history. Based on the records of specialists at this stage, it is possible to assume the cause of irritable bladder syndrome. The doctor also asks you to describe the symptoms in detail: frequency of trips to the toilet, approximate volume of urine excreted, sensations when urinating. The following biochemical tests will be required:
- General blood and urine analysis.
- Urine analysis for cytological examination to detect cancer cells.
- Testing for sexually transmitted diseases.
To determine the condition of the bladder, a urodynamic study is performed using uroflowmetry or cystometry using a small-diameter catheter.
Ultrasound is used in the diagnosis of irritable bladder syndrome
If necessary, an ultrasound examination of the genitourinary system will be required. Before the procedure, the patient empties his bladder, and an ultrasound scan determines how much urine is left and whether this amount is normal. Sonography can also detect benign or malignant tumors that may cause irritable bladder syndrome.
A computed tomography scan may be required to clarify the diagnosis. If you have diseases of the endocrine glands, you will need to consult an endocrinologist. If the doctor suspects that the underlying etiology of the disease is a dysfunction of the nervous system, it is necessary to treat the disease with the participation of a neurologist.
CT is used to determine the causes of irritable bladder syndrome
Features of the male genitourinary system
The bladder in men communicates with the narrow and long urethra, which passes through the penis. The urea is adjacent to many organs of the reproductive and excretory system:
- ureters;
- seminal vesicles;
- prostate;
- rectum;
- vas deferens;
- urethra.
Injuries and infectious inflammation of any of them are fraught with damage to the urinary tract. Untimely treatment of diseases leads to complications - sexual impotence, infertility.
Several treatment options
If irritable bladder syndrome is an independent disease, then the cause of its occurrence is neurogenic in nature. Treatment is based on bladder training: the patient should go to the toilet no more than once every two hours. At the same time, he keeps a diary, where he records the indicators by which the doctor evaluates the effectiveness of this technique.
Medications for urinary incontinence in older women
An important component of the treatment of the disease is performing a certain set of exercises to strengthen the pelvic muscles. Such exercises have been used for more than a hundred years to treat urinary incontinence, and Arnold Kegel was the first to systematize them and give them a scientific basis in 1948. A positive result occurs after just a few weeks of regular exercise.
Treatment of irritable bladder syndrome is carried out using a physiotherapeutic procedure - electromagnetic stimulation of the bladder. The patient is also recommended to eat foods high in coarse fiber (bran, cereals). The diet can eliminate the symptomatic manifestations of irritable bowel syndrome that accompanies the underlying disease.
When treating irritable bladder syndrome, it is necessary to keep notes in a diary.
Pharmacological therapy is used in patients with urge urinary incontinence, which occurs due to bladder weakness. Treatment begins with the use of tricyclic antidepressants and mild sedatives: irritable bladder syndrome exposes patients to constant stress.
There are three types of drugs, the use of which successfully cures the disease:
- M-anticholinergics and (or) alpha1-blockers that reduce stimulation of the muscular lining of the bladder (detrusor). They are used as the first line of treatment for the syndrome and are highly effective and safe.
- Botulinum toxin (Botox). Intravesical Botox injections (25-30 pieces) normalize muscle tone, slowing down the release of acetylcholine from the nerve ending. The duration of action of the drug is about 12 months, then the procedure will have to be repeated.
- One of the analogues of vasopressin. The medicine reduces the formation of urine and shifts the urination cycle to the night.
Research is currently being conducted on the use of estrogens to treat older women with irritable bladder syndrome.
Treatment with folk remedies helps reduce symptoms of irritable bladder syndrome
You can treat the syndrome with folk remedies using the following infusions:
- 2 tbsp. l. orthosiphon staminate, pour 0.5 liters of boiling water and leave for 3 hours. Drink the infusion throughout the day.
- 3 tbsp. l. St. John's wort and 3 tbsp. l. Pour 1 cup of boiling water over bear ears and leave for 5-6 hours. Take 50 ml 3 times a day after meals.
- 2 tbsp. l. elecampane and 1 tbsp. l. pour thyme into 1 liter of boiling water and leave for 3 hours. Drink in small portions throughout the day.
Medicines
Doctors prescribe medications that affect the nervous system. The dose and type of drug are determined by a specialist individually in accordance with the degree of development of the disease.
Commonly used medications include:
- M-anticholinergics (Detrol, Detrusitol, Driptan);
- sedatives (Novo-passit, Afobazol, Tenoten);
- tricyclic antidepressants (imipramine).
If the disease is infectious, antibacterial, antifungal or antiviral drugs are prescribed (in accordance with the nature of the infectious agent).
If necessary, antispasmodics and antihistamines are included in the therapeutic regimen.
In women of menopausal age, treatment can, if necessary, be supplemented with hormonal drugs. They are selected for patients exclusively by a gynecologist.
What you need to know about prevention
An excellent way to prevent irritable bladder syndrome is to have a regular annual physical examination. Pathologies cured in time will not become a source of other, often more unpleasant diseases.
If the first symptoms appear, you need to reconsider your diet and completely exclude from it:
- Products containing caffeine.
- Citrus.
- Alcohol.
They negatively affect the condition of the mucous wall of the bladder, increase its sensitivity, and lead to frequent contractions.
Stressful situations, neuroses, and depression will not be cured on their own, but can cause serious physiological disorders in the body. They provoke sleep disturbances, irritation, increased nervous excitability, and anxiety. This condition will inevitably lead to irritable bladder syndrome, so an urgent consultation with a neurologist is required.
Causes
The occurrence of the syndrome can be associated with both physiological manifestations and neurogenic factors:
- Heredity. A predisposition to this pathology is often passed on from parents to children.
- Age. Aging leads to changes in hormonal levels and reduced production of biologically active steroids. For this reason, the structure of the vascular walls, ligaments and muscles changes.
- Congenital developmental pathologies.
- Prostate adenoma in men. The appearance of nodes in the prostate is fraught with compression of the urethra. The walls of the bladder become less elastic, blood flow deteriorates, and an increased urge to urinate appears.
- Urogenital infections, urolithiasis.
- Osteochondrosis.
- Strokes. As a result, brain damage occurs.
- Traumatic brain injuries.
- Anatomical disorders. They occur as a result of intense sports training or professional activities that involve heavy lifting. People who are overweight and who have undergone surgery on the pelvic organs are at risk.
- Impaired functioning of the nervous system. Frequent urination occurs due to an inflammatory process in the spinal cord, benign and malignant neoplasms, and malfunction of the endocrine glands (due to diabetes mellitus).
- Use of medications that increase diuresis.
- Abuse of caffeinated drinks.
Important! The disease can be diagnosed in patients who do not have a history of any of the listed causes. Studies have been conducted on such patients in an attempt to find similar symptoms in them. It was found that the majority suffered from sleep inversions, nervous disorders, and irritable bowel syndrome.
How to make it easier to function?
Two small kidneys are the strongest protection against germs, toxins, and infections. They are the ones who remove harmful substances by dispersing all the blood several times a day. This is a very serious load. Therefore, it is extremely important to facilitate the functioning of these organs. In addition, understanding what is good for a person’s kidneys can even help them cleanse the blood of harmful impurities.
Every day the body faces the threat of infection. To protect yourself from the development of pathology, you should be careful about your health. To do this, it is recommended to start with simple rules:
- Exercise stress. It is not only dietary nutrition that will have a beneficial effect (we will discuss below what is good for the kidneys to eat and drink). Exercises performed daily will protect against poor circulation and stagnation. And, as is known, such phenomena lead to the accumulation of fat in the lumbar region, which significantly impairs the functioning of not only the kidneys, but also many systems. The beneficial loads will increase blood flow. This activates the removal of toxins from the body.
- Protection against infection and inflammation. Always dress for the weather. Don't forget to insulate your lower back. It is forbidden to sit on cold surfaces. Unfortunately, very often such advice is ignored. As a result, kidney diseases occur in a chronic form. In the initial stages, symptoms usually go unnoticed. Slight aching pain in the lumbar region, slight aches, low temperature - these are signs that few people pay attention to. However, ignoring the pathological process can lead to exacerbation.
Kidneys are quite vulnerable organs. Their work can be disrupted by drinking (bad) water, unhealthy food, or medicine. An infection that enters any part of the body will again be carried through the bloodstream to these organs. That is why it is so important to understand what is good for the kidneys and what is contraindicated.
In addition to the above recommendations, diet occupies a special place. The choice of food should be approached very carefully. After all, some products can expel sand, dissolve stones, and effectively cleanse the body.