Renal hypertension - what is it?
The disease is diagnosed with high diastolic pressure of 140/90, which cannot be reduced by conventional medications. Renal arterial hypertension is pathological changes in the tissues and blood vessels of the organ that cause kidney disease.
The disease may be caused by:
- immunoinflammatory nature of the renal glomeruli - glomerulonephritis;
- kidney dystonia (movement of the organ from the pelvis to the lumbar region);
- damage to the tubular system, usually of an infectious nature - pyelonephritis;
- expansion of the pelvis and calyces caused by compression of the ureter and disruption of the outflow of urine - hydronephrosis;
- nephrosclerosis (wrinkling, with the kidney tissue being replaced by connective tissue).
Pathophysiology. The function of the kidneys is related to filtering the bloodstream and removing excess fluid and toxins from the human body. Cleansing occurs in the renal glomeruli, where arterial blood is cleansed and released further into the bloodstream. The pathogenesis of the development of renal hypertension raises many questions among specialists. Today, the formation of organ pathology is influenced by several factors leading to disease.
Disorders caused by kidney dysfunction lead to the retention of water and ions of the element Na (sodium). The walls of the blood vessels begin to enlarge, which leads to increased sensitivity to substances that help narrow the arterial vessels. The kidneys continue to secrete a substance (enzyme) that combines with the protein. It prevents the removal of sodium from the body.
Important! In the organ itself, the deficiency of components that lower blood pressure continues to increase. All these disorders lead to renal hypertension.
Therapeutic measures
Nephrogenic arterial hypertension develops quickly, affecting the brain, heart and disabling the kidneys , so therapeutic methods are ineffective. It is important for the patient to provide assistance immediately after determining the cause of PG and direct maximum efforts to eliminate it. Unconditional priority goes to invasive and surgical methods.
Balloon angioplasty: The stenotic areas are widened by inflating a balloon at the end of a catheter inserted into the renal artery. The combination with strengthening the wall with a microprosthesis (stent) will protect the vessel from re-narrowing.
Operations: possible only with preserved kidney functionality. They are used for complex stenosis, blockage of the artery lumen, and ineffectiveness of balloon angioplasty. According to indications, removal of the affected kidney.
Therapy: treatment of renal hypertension combines means to influence the underlying disease (in the parenchymal form), as well as drugs that block the formation of angiotensin-II (Captopril) and reduce the activity of renin production (Propanolol).
Read also: Nocturnal arterial hypertension
Prognosis: favorable if after the operation the pressure begins to decrease and atherosclerosis does not develop in the kidneys. Unfavorable – if there is a problem with both kidneys, complications such as heart failure, kidney failure, or stroke.
Classification
Impaired functioning of the renal arteries appears in all its pathologies. Modern medicine classifies three groups.
Renoparenchymatous
The disease is based on disturbances in the functioning of the cells of the outer and inner layer and dysfunction of homeostasis. The renal membrane, which is responsible for the accumulation and outflow of liquid products, is affected and loses its functionality. Reverse blood flow appears, swelling occurs, and protein appears in the blood and urine. Parenchymal lesions are associated with:
- with the presence of stones,
- tuberculosis of a paired organ;
- diabetes mellitus;
- pyelonephritis (ICD code 10);
- glomerulonephritis;
- anomalies of the paired organ.
Renovascular
Vasoconstriction of arteries. Pathology may affect one or more vessels. The lumen narrows by 70 percent or more, which causes kidney failure.
The reasons may be:
- for older people – atherosclerosis;
- emerging tumors, cysts, hematomas.
Important! There is little effectiveness of the prescribed drugs to lower blood pressure.
The last in the classification of disorders are mixed combinations of damage to the parenchyma and arteries. This may include vascular abnormalities, benign and malignant tumors, and a number of others.
What varieties are there?
Depending on the causes of development and symptoms characteristic of this disease, the following types of renal hypertension :
- Parenchymatous. This form is characterized by pathological damage to organ tissue, developing as a result of diseases such as glomerulonephritis, pyelonephritis, ischemic kidney disease, cystic formations in the kidneys, and kidney dysfunction during pregnancy;
- The renovascular form occurs against the background of damage to the blood vessels of the kidney (thrombi, aneurysms, sclerotic plaques). This variety is typical for representatives of the younger generation (children under 10 years old); in adulthood, the pathology is somewhat less common;
- The mixed form is characterized by signs of parenchymal and renovascular forms. This pathology occurs when the kidneys prolapse and there are abnormalities in their development.
Causes
The disease has causes that are congenital and acquired.
Congenital:
- improper tissue development, thrombosis and blockage of blood vessels;
- arteriovenous shunt - a direct connection between an artery and a vein;
- damage to a vascular organ;
- defect of the aorta, urinary system.
Acquired factors include:
- vascular atherosclerosis;
- organ prolapse;
- venous-arterial fistula;
- inflammation in the artery;
- mechanical compression by a tumor;
- the presence of urolithiasis.
Therapy
Treatment of renal hypertension should be carried out under the strict supervision of a physician. Having diagnosed the disease, he prescribes medications taking into account the individual sensitivity of the microflora. Arterial hypertension is treated based on two principles: treatment of kidney disease and therapeutic measures to reduce blood pressure. When arterial hypertension is severe, surgical intervention is indispensable.
Treatment of a disease such as arterial hypertension is carried out with the help of special medications. The following medications are effective here:
- Etamzilata;
- Contrikal;
- Gordoks;
- Aminomethylbenzoic acid.
Aminomethylbenzoic acid
Etamzilata
Gordoks
Contrikal
The use of antifibrinolytics in this case is risky. Such treatment is fraught with bleeding, which cannot be stopped quickly. The choice of drug and its dosage is determined by the doctor, taking into account individual characteristics and the course of the disease.
Operation
When the cause of renal hypertension is arterial stenosis, treatment includes surgery. Its goal is to normalize renal hemodynamics and prevent the development of nephrosclerosis, prevent and treat infertility, and stop bleeding.
Signs and symptoms
The symptoms of the disease are varied. The clinical nature of hypertension consists of symptoms of pathology of the paired organ and the presence of elevated blood pressure. The degree of severity depends on the severity of the disease.
Benign forms progress slowly and their manifestations are erased. Common symptoms include palpitations, shortness of breath, weakness, fatigue, headaches and fatigue. In benign forms, stable pressure is observed. This increases the upper and lower pressure. Malignant forms progress, and their manifestation is vivid. Accompanied by panic attacks.
Important! The patient does not remember events well and does not assimilate the material read. He is plagued by headaches and constant dizziness. The kidney area is painful.
The patient experiences:
- lumbar pain;
- frequent urge to urinate and increased fluid output;
- high temperature.
For reference! Signs of the disease are directly related to internal pathologies and depend on the genesis of the disease (diabetes, tuberculosis, etc.). The clinical picture depends on concomitant diseases: heart attack, heart disease.
Malignant arterial hypertension: treatment and prevention in hypertensive patients
To prevent renal arterial genesis, you need to listen to the following recommendations:
- Monitor blood pressure;
- At the first signs of renal arterial origin, go to the doctor;
- Lose extra pounds;
- Consume less salt;
- Quit smoking;
- Do physical exercise.
Arterial hypertension is a dangerous disease that causes a lot of complications. Avoiding such a pathology is possible only with careful adherence to all preventive measures and a routine examination by a doctor. After all, as you know, it is better to prevent the occurrence of a disease than to treat it later.
Prevention of the disease is aimed not only at normalizing blood pressure, but also at preventing the development of renal pathology. For chronic diseases, medications are recommended to keep internal organs in working order and to restore normal metabolism.
For patients with renal failure, it is important to closely monitor the symptoms of renal hypertension and avoid inappropriate exercise and hypothermia. Modern medicine methods allow you to maintain normal blood pressure.
Arterial hypertension (AH) is a disease characterized by a persistent, constant, long-term increase in blood (arterial) pressure numbers, systolic over 140, diastolic over 90. Arterial hypertension is one of the most widespread chronic cardiovascular pathologies. Many people who encounter it are interested in what it is and how to treat this pathology.
People of all races and all walks of life are prone to the disease. The incidence rate is lower in third world countries, which confirms the theory of the “stressful” origin of the disease.
Despite the fact that this disease is characterized by a chronic course, sudden surges or a malignant course are not uncommon for it. Malignant hypertension is a pathological condition for which retinopathy (pathology of the retina) and necrosis of nephron arterioles are pathognomic. Of course, treatment of malignant hypertension is carried out under the strict supervision of a physician.
An informative and main diagnostic method used to determine malignant arterial hypertension is measuring blood pressure using the Korotkoff method. To do this, the patient must have a tonometer with him. It can be electronic or mechanical. The tonometer must be properly calibrated, checked by a specialist and compared with the indicators of other tonometers.
It is important to conduct the study 10-15 minutes after a quiet rest. In no case should you start measuring after stress, climbing stairs or other unusual physical activity of the patient.
Diagnostics
Diagnosis is carried out in stages:
- First, anamnesis is collected: time of occurrence, drug therapy, hereditary factors, and connections with renal pathologies are determined.
- Perform correct blood pressure measurements. With hypertension, the pulse rate decreases and the pressure on the vessel walls (diastolic) increases. Blood pressure is measured on the right and left arms. If they differ significantly, aortoarteritis is observed.
- One of the manifestations of the disease during listening will be stenotic noise in the navel area. They are associated with narrowing of the arteries. Blood flow, passing through areas of compression, will make specific noises. Systodiastolic listening will indicate aneurysmal protrusion of arterial vessels.
- Examine the fundus. It is especially indicated if the patient loses vision. Hypertensive pathology of arterial lesions leads to atrophy of the retinal vessels. On examination, hemorrhages and swelling are visible.
- An ultrasound examination of the kidneys (ultrasound) is performed. It gives a clear picture of the size of the lesion: abnormalities of the organ and blood vessels, the presence of concomitant renal diseases.
- Excretory urography is performed. It will show whether increased blood pressure is associated with a malfunction of the paired organ.
- A Doppler angiographic study will show developing vascular pathology and circulatory disorders in the renal tissues. It will easily determine atherosclerosis and the presence of abnormal vessels.
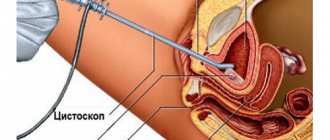
- An angiography method is used using a contrast agent. This is the most effective way to recognize vascular pathology. With its help, the following are determined: vessel sizes, configuration, areas of narrowing. For the procedure, a puncture of the femoral artery is made and a catheter with contrast is inserted.
- I can use radioisotope scintigraphy. A radioisotope substance is injected into a vein. But this method does not allow determining the extent of the pathology.
- Computer diagnostics and MRI (magnetic resonance imaging) are most often used.
- In laboratory conditions, the quantitative content of renin in the bloodstream that leaves the kidney is determined. The mechanism of organ damage can be determined by assessing a biopsy (examination of damaged tissue samples under a microscope).
Note! In severe forms, the patient experiences loss of some visual fields.
How is it diagnosed?
To make an accurate diagnosis, it is not enough just to evaluate the symptoms of the disease. It is necessary to conduct numerous laboratory and instrumental studies , such as:
- Blood test for the content of the hormone renin. An increase in the level of this hormone indicates an increased salt content in the body, which indicates a violation of the kidneys.
The level of the hormone can change throughout the day, so the study is carried out several times to obtain the necessary information. In addition, the intake of certain medications contributes to an increase in renin levels, therefore, before taking the test, it is necessary to stop taking them (at least 2 weeks in advance);
Read also: Arterial hypertension treatment pills
- A complete blood count can detect an increase in the level of red blood cells and hemoglobin in the blood. This study is not sufficiently informative, since erythrocytosis in renal hypertension occurs in rare cases;
- A biochemical blood test can detect increased levels of cholesterol and low-density lipoproteins. This is typical for the renovascular form of renal hypertension;
- The Rehberg test is prescribed to patients with hypertension to detect nephrogenic hypertension;
- A general urine test allows you to detect red blood cells and white blood cells in the test material, which indicates a pathological process affecting the organs of the urinary system;
- Urography (survey or excretory) allows you to evaluate the structure of organ tissue and its functionality. It is important to remember that the use of this diagnostic method at moments of critical increase in pressure can be dangerous for the patient;
- Ultrasound in combination with duplex scanning is necessary to determine the size of the affected kidney, assess the condition of the organ’s blood vessels and determine the speed of blood flow;
- Radioisotope scintigraphy of the kidneys is necessary to determine violations of the secretory function of the proximal tubules, functional, anatomical or structural features of the kidney structure;
- Renal angiography (x-ray of the kidney using a contrast agent) is the most informative diagnostic method that allows you to identify damage to the blood vessels of the organ, determine the scale and localization of these damage.
Forecast
The disease is characterized by a sudden, persistent increase in blood pressure, which in 60% of cases quickly causes deterioration in the functioning of target organs and life-threatening pathologies.
If the diagnosis is made in the early stages of development, then in more than 80% of patients the disease can be completely eliminated. Surgical treatment and the recovery process after it take up to three months.
The prognosis for renal arterial hypertension syndrome depends on the advanced stage of the disease, timeliness, and the correct choice of treatment methods. It worsens significantly with bilateral kidney damage.
Adelina Pavlova
General nurse. More than 40 years of working experience. Retired copywriter.
More about the author
Last updated: August 22, 2019
Blood pressure self-monitoring diary
| date | Time | Arterial pressure | Medicines | Notes |
| Morning, 07:30 | ||||
| Evening, 21:00 |
In the meantime, we listen to the sensations: is there any discomfort or pain in the lower back, painful or frequent urination, etc., as discussed above. We turn to a therapist with a self-monitoring diary and a list of complaints.
a general urine test at the clinic (regular urine is taken during the day), a urine test according to Nechiporenko (an average portion of morning urine), a urine test for microalbuminuria (detects protein at an early stage of kidney damage) and an ultrasound of the kidneys . It is better to conduct such an examination annually to keep arterial hypertension under control and not to miss kidney damage, even if it was not detected initially.
If the kidneys are proven to be responsible for the increase in blood pressure, they need to be treated while taking blood pressure medications. It often happens: the inflammatory process in the urinary system is stopped (in the initial stage of the disease), and the pressure decreases significantly, even returning to normal.
If the changes in the kidneys are chronic, the drugs are taken constantly - even when the pressure is normalized. Their use is aimed at protecting blood vessels from excessive stress and restoring their former elasticity. I think it would be useful to remind you: the pills are prescribed by a doctor . It is he who selects groups of drugs that take into account the functioning of the kidneys and the associated mechanisms of increasing blood pressure.
What is the danger of the disease?
An increase in intravascular pressure is dangerous due to a significant increase in the risk of developing damage to the so-called target organs. These include the vessels of the brain, heart muscle, lungs and even retinal arteries. If hypertension is not properly treated, pulmonary edema, hemorrhagic cerebral stroke, myocardial infarction, or retinal hemorrhage may occur. Renal hypertension has a greater risk of such complications, since it is more permanent in nature, and if it is present, not only the systolic value increases, but also the diastolic value.
Due to various pathologies in the kidneys, there is a decrease in the normal flow of blood to this organ.