Kidney amyloidosis is a disease during which an abnormal protein - amyloid - accumulates in the tissues and thereby disrupts the normal functioning of the organ. Often, with the primary form of the disease, the patient does not even suspect the development of pathology, because it does not manifest itself at all and has vague symptoms. But the secondary form manifests itself as a complication from the underlying disease. The protein that is deposited in the tissues of the organ can be of several types. Depending on this, the following forms of the disease are distinguished: Primary renal amyloidosis - occurs as an independent disease. Experts do not find any causes in the form of a chronic disease, etc. In this case, damage occurs to the lungs, heart, kidneys, liver, thyroid gland, skin and tongue. Secondary renal amyloidosis is more common. Appears against the background of chronic diseases, especially Crohn's disease, rheumatoid arthritis, osteomelitis, and so on. The most common areas affected are the lymphatic and blood vessels, liver, kidneys and spleen. Some experts also tend to distinguish senile and congenital forms of the disease . The first affects only elderly people, the second is genetically determined.
With amyloidosis, abnormal protein accumulates in the kidney tissue, which leads to serious changes in the organ
Classification of forms of renal amyloidosis
In accordance with etiopathogenetic mechanisms, five forms of renal amyloidosis are distinguished: idiopathic, familial, acquired, senile, local tumor. In primary (idiopathic) renal amyloidosis, the causes and mechanisms remain unknown. Family (hereditary) forms are caused by a genetic defect in the formation of fibrillar proteins in the body. Secondary (acquired) renal amyloidosis develops in immunological disorders (chronic infections, rheumatic diseases, malignant tumors, etc.). The basis of senile amyloidosis is an involutive change in protein metabolism. The nature of local tumor-like renal amyloidosis is unclear.
Depending on the type of fibrillar protein contained in amyloid, various forms of amyloidosis (“A”) are usually designated by the following abbreviations: AA type (secondary, amyloid contains serum a-globulin); AL-type (idiopathic, in amyloid - Ig light chains); ATTR type (familial, senile; in amyloid – transthyretin protein); A2M type (dialysis; in amyloid - β2-microglobulin), etc. Idiopathic, familial, senile and local tumor forms of amyloidosis are distinguished into independent nosological units. Secondary renal amyloidosis is considered as a complication of the underlying disease.
Taking into account the predominant damage to any organ and the development of its failure, nephropathic (renal amyloidosis), epinephropathic, neuropathic, hepapathic, enteropathic, cardiopathic, pancreatic, mixed and generalized variants of amyloidosis are distinguished. Regardless of the form and type, amyloidosis occurs when specific structural elements of tissue are displaced by the amyloid substance, reducing, and ultimately losing, the functions of the corresponding organs. Systemic (generalized) amyloidoses include AL-, AA-, ATTR-, A2M amyloidoses; to local – amyloidosis of the kidneys, atria, pancreatic islets, cerebral, etc.
Systemic amyloidosis - features
The disease belongs to the category of dysproteinoses, accompanied by disruptions of protein metabolism. The disease occurs in the event of a failure of the immune system, for this reason, to represent the essence of the disease processes occurring in the patient’s body, certain knowledge in the section of immunology and physiology is required.
Amyloid is a whole complex, including 95% fibrillar protein and 5% nucleoproteins of blood and cells.
Normally, amyloid protein is not formed in the body, but it is formed in the event of amyloidosis.
The appearance of pathology is characterized by:
- formation of amyloidoblasts. The first stage of the disease is accompanied by mutational changes occurring in different immune cells. Cells of the macrophage category, monocytes, and lymphocytes undergo mutation, transforming into a new type of cell - amyloidoblasts. With the development of pathology, their volumes grow, and they settle in various internal organs;
- synthesis of fibrillar protein in amyloidoblasts in the form of thin and elongated structures (filaments). They subsequently combine to form the basis of amyloid. Fibrillar protein is foreign to the body. Amyloidoblasts are surrounded by other cells that absorb and destroy their protein, preventing it from entering the body's tissues. The process can last for a long period (the latent stage of the disease), as a result, immunological tolerance is constantly created (the body’s adaptation to the new protein and the cessation of “protection” against it), which causes the entry of a large volume of fibrillar protein into the tissues.
- amyloid deposits in tissues. Amyloid is formed in the intercellular space after the combination of fibrillar protein with proteins and blood nucleoproteins. The relationship between substances is so strong that it cannot be destroyed. As a result, the formed amyloid accumulates in tissues, eventually displacing healthy cells.
In the case of certain forms of the disease, amyloidoblasts are able to transform into cells of other organs, which is accompanied by the manifestation of symptoms.
Causes of renal amyloidosis
The etiology of idiopathic renal amyloidosis remains unknown in most cases; Sometimes the disease develops with multiple myeloma. In addition to the kidneys, primary amyloidosis can affect the tongue, skin, thyroid gland, liver, lungs, intestines, spleen, and heart.
Secondary amyloidosis is usually associated with chronic infections (syphilis, tuberculosis, malaria), purulent-destructive processes (brochiectasis, pleural empyema, osteomyelitis, prolonged septic endocarditis), systemic diseases (rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis), intestinal diseases (ulcerative colitis, Crohn's disease), tumors (lymphogranulomatosis, meningioma, kidney tumors), etc. Secondary amyloidosis affects the kidneys, blood vessels, lymph nodes, liver and other organs.
The cause of dialysis renal amyloidosis is the patient's prolonged hemodialysis. Familial hereditary amyloidosis occurs with periodic illness, often in Mediterranean countries (in particular, the Portuguese variant). Senile amyloidosis is considered a sign of aging, occurring after 80 years in 80% of people. Local forms of amyloidosis can be caused by tumors of the endocrine system, Alzheimer's disease, type 2 diabetes mellitus and other reasons.
Among the theories of the pathogenesis of renal amyloidosis, the immunological, mutational and local cellular synthesis hypotheses are considered. Renal amyloidosis is characterized by extracellular deposition in the renal tissue, mainly in the glomeruli, of amyloid, a special glycoprotein with a high content of insoluble fibrillar protein.
General information
As a result of metabolic disorders in the body, excessive formation and accumulation of amyloid in the tissues of the organ begins. The presence of this substance is in itself a pathology, since it is absent in a healthy body. Once in the tissue, amyloid quickly grows and fills a lot of space, due to which the substances necessary for the tissue are displaced, and organ degeneration occurs. Therefore, this phenomenon is called amyloid dystrophy. Kidney performance decreases and then stops, leading to kidney loss. The pathology is considered rare and accounts for 2% of the total number of kidney diseases. There are two cases per 100 thousand people.
Amyloidosis provokes severe complications and is a dangerous disease both for human health and for life in general. The level of amyloid in the blood sometimes increases in the presence of concomitant pathologies: tuberculosis, syphilis. Inflammation of any tissue also contributes to its formation. At the same time, it can damage the liver and blood vessels. Scientists have managed to study the structure of this substance, but the factors of its occurrence have not yet been fully established.
Classification of forms
Amyloidosis has several forms, differing in the factors for the development of pathology:
- Primary amyloid dystrophy. Does not depend on concomitant pathologies. Rare form.
- Secondary amyloid dystrophy. Arises as a consequence of other
pathologies. The most common form.
- Amyloidosis provoked by extrarenal blood purification.
- Congenital amyloid dystrophy. Passed on from parents to children.
- Senile amyloidosis. Occurs in people over 80 years of age.
The structural features of amyloid divide the pathology into several types:
- Primary AL amyloidosis. Protein synthesis is provoked by genetic abnormalities.
- Secondary AA amyloidosis. Refers to the form that arose against the background of inflammatory processes, since these are optimal conditions for the formation of AA amyloid. If inflammation is not treated, the protein accumulates in large quantities, settles in the kidney parenchyma and causes organ degeneration.
- Hereditary familial ATTR amyloidosis. A rare type, which includes the senile form and polyneuropathy - a pathology of the nervous system transmitted at the gene level.
Symptoms of kidney amyloidosis
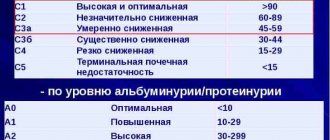
In renal amyloidosis, renal and extrarenal manifestations are combined, causing a polymorphic picture of the disease. During renal amyloidosis, 4 stages are distinguished (latent, proteinuric, nephrotic, azotemic), which have characteristic clinical symptoms.
In the latent stage, despite the presence of amyloid in the kidneys, clinical manifestations of amyloidosis are not observed. During this period, the symptoms of the primary disease (infections, purulent processes, rheumatic diseases, etc.) predominate. The latent stage can last up to 3-5 years or more.
In the proteinuric (albuminuric) stage, an increasing loss of protein in the urine, microhematuria, leukocytes, and an increase in ESR appears. Due to sclerosis and atrophy of the nephrons, lymphostasis and hyperemia, the kidneys enlarge, become dense, and acquire a matte gray-pink color.
The nephrotic (edematous) stage is characterized by sclerosis and amyloidosis of the renal medulla and, as a consequence, the development of nephrotic syndrome with a typical tetrad of symptoms - massive proteinuria, hypercholesterolemia, hypoproteinemia, edema, resistant to diuretics. Arterial hypertension may be present, but more often blood pressure is normal or low. Hepato- and splenomegaly are often observed.
In the azotemic (terminal, uremic) stage, the kidneys are scar-wrinkled, dense, and reduced in size (amyloid kidney). The azotemic stage corresponds to the development of chronic renal failure. Unlike glomerulonephritis, persistent edema persists with renal amyloidosis. Renal amyloidosis can be complicated by renal vein thrombosis with anuria and pain. The outcome of this stage is often the death of the patient from azotemic uremia.
Systemic manifestations of renal amyloidosis may include dizziness, weakness, shortness of breath, arrhythmia, anemia, etc. In the case of intestinal amyloidosis, persistent diarrhea develops.
Symptoms of the disease
Kidney damage in amyloidosis is often asymptomatic until the onset of stage 3 or 4 of the disease. The primary form of the disease is more common in patients over 40 years of age. This form is the most dangerous because of its transience. Primary amyloidosis is often fatal.
The secondary type of the disease, which appears against the background of the development of some other disease, most often occurs in patients over the age of 60 years. The symptoms in this case are also not clearly expressed due to the fact that the patient is tormented by manifestations of another disease.
Secondary amyloidosis is divided into types, each of which has its own set of symptomatic features.
Preclinical stage
During this period, although amyloid is produced in the kidneys, it is not in such quantities that can seriously disrupt their functioning or lead to the development of pronounced symptoms. Usually the patient does not feel anything. This condition can last up to 5 years. It is impossible to detect the disease at the preclinical stage using ultrasound.
Proteinuric stage
May last from 10 to 15 years. At the same time, large amounts of amyloid accumulate in the kidneys. It has a destructive effect on the walls of kidney cells and increases their permeability significantly. When tested, the results show an excess of protein in the urine. At the proteinuric stage, there are also no symptoms.
The only way to diagnose the disease is to conduct a laboratory test of the samples taken. In the affected kidneys, the changes are already irreversible; it is not possible to see it externally.
Nephrotic stage
For the patient, it is characterized by the most severe symptoms, which are due to the fact that the protein is practically no longer contained in the blood, but is completely eliminated from the body. The kidney filter does not cope with its function:
- sudden weight loss;
- dry mouth, a person is constantly thirsty;
- the amount of urine excreted constantly decreases until it stops completely;
- weakness in which a person is no longer able to perform his usual daily duties;
- decreased appetite up to its complete loss;
- when you try to get out of bed into a sitting or standing position, your blood pressure drops sharply;
- characteristic swelling. First - on the face, legs. Further, the swelling begins to spread to other parts of the body, including organs;
- nausea.
Uremic stage
Characterized by painful, severe symptoms. At this stage, the kidneys cease to fully perform their functions and lose their original appearance (the structure is completely changed, wrinkled).
The swelling is pronounced. The person suffers from nausea and vomiting, constant abdominal pain, and elevated body temperature. The patient is in a severely weakened state, periods of improvement no longer occur. At this stage, urine completely stops being excreted. When palpating, the pulse is difficult to hear, blood pressure is very low.
Modern medicine does not have the means to remove amyloids from the body. This stage leads to death. In this case, in addition to the kidneys, other vital organs and systems are damaged.
Diagnosis of renal amyloidosis
In the early preclinical period, diagnosing renal amyloidosis is extremely difficult. At this stage, priority is given to laboratory methods - the study of urine and blood. In a general urine analysis, proteinuria is noted early, which tends to steadily increase, leukocyturia (in the absence of signs of pyelonephritis), microhematuria, and cylindruria.
Biochemical blood parameters are characterized by hypoalbuminemia, hyperglobulinemia, hypercholesterolemia, increased activity of alkaline phosphatase, hyperbilirubinemia, electrolyte imbalance (hyponatremia and hypocalcemia), increased fibrinogen and b-lipoproteins. A general blood test revealed leukocytosis, anemia, increased ESR. When examining a coprogram, a pronounced degree of steatorrhea (“fatty stool”), creatorrhoea (a significant content of muscle fibers in the stool), and amilorrhea (the presence of a large amount of starch in the stool) are often revealed.
Due to severe metabolic disorders in renal amyloidosis, arrhythmia and conduction disturbances may be recorded on the ECG; EchoCG shows cardiomyopathy and diastolic dysfunction. An abdominal ultrasound reveals an enlarged spleen and liver. X-ray of the gastrointestinal tract reveals hypotension of the esophagus, weakened gastric peristalsis, acceleration or deceleration of the passage of barium through the intestines. An ultrasound of the kidneys shows their enlargement (large fatty kidneys).
A reliable method for diagnosing amyloidosis is a kidney biopsy. Morphological examination of the biopsy after staining with Congo red and subsequent electron microscopy in polarized light reveals a green glow, characteristic of renal amyloidosis. Amyloid can be detected along the vessels, tubules, and in the glomeruli. In some cases, a biopsy of the rectal mucosa, skin, gums, and liver is performed.
Detection of the disease: description of procedures
To check for amyloidosis, the doctor usually prescribes the following diagnostic methods: physical examination, blood and urine tests. If the result reveals unusually high levels of protein, the doctor may order a biopsy (sampling) to directly examine the tissue.
If the doctor suspects that amyloidosis is present in 3-4 organs, several tissue samples should be taken. These include abdominal fat, bone marrow, jaw, salivary glands, skin and rectum. If removal must be made from internal organs - heart, liver or kidney - surgical intervention is necessary. Differential diagnosis with autoimmune diseases and other pathologies should be carried out by a qualified specialist.
Laboratory diagnostics
It is recommended to avoid intravenous pyelography in patients with suspected amyloidosis because contrast media exposure is associated with increased renal impairment. Ultrasonography (ultrasound) is useful in determining the size of the kidneys, but in patients with amyloidosis the organs may be large, small, or normal.
Single photon emission computed tomography (SPECT) may also be useful because technetium is sometimes associated with soft tissue amyloid deposits. However, SPECT does not provide much sensitivity, and reports of its specificity compared with CT vary widely. If the results are positive, SPECT can be used to monitor the overall progression of deposition in a given organ.
MRI may play a role in the diagnosis of amyloidosis in the future, but currently no formal study has reported its use in a large series of patients.
Instrumental research methods
To detect amyloid, a biopsy of the affected organ is the most sensitive method. It is also able to identify concomitant pathologies. However, tissue removal carries the risk of complications, particularly bleeding. If amyloidosis is clinically suspected, a less invasive procedure will be required. In the early 1970s, scientists demonstrated that amyloid could be found in subcutaneous fat. For decades, subcutaneous fat biopsy obtained by fine-needle aspiration has been safe, cheap, and rapid and has been introduced as a screening test for amyloidosis.
Rectal biopsy is more useful than subcutaneous fat aspiration for type AA amyloidosis. It has been found to produce positive results (provided that the submucosal portion is included in the biopsy specimen) in 80-85% of patients who are eventually found to have tissue amyloid in a clinically significant location. Biopsies from either subcutaneous fat aspiration or rectal tissue can be studied for the presence and nature of amyloid precursor.
Occasionally, patients have positive results on subcutaneous fat aspiration when they are negative on rectal biopsy. Using both procedures can increase the accuracy of pathology detection by up to 90%. Abdominal subcutaneous tissue data are not very sensitive to FMF-induced AA amyloidosis or dialysis-associated amyloidosis. Findings are usually negative, probably because beta2-microglobulin does not accumulate in this tissue.
In the past, liver biopsy was a common procedure in the study of AA amyloidosis. Several reports of fatal rupture or bleeding in the organ, as well as the presence of sampling procedures with little or no morbidity and mortality, have led to its decreased use.
The tissue is stained with Congo red alkaline solution and examined under polarized light, where positive (green) refraction is detected in the presence of any type of amyloidosis. The nature of the fibril precursor can be determined by immunohistochemical staining with antibodies specific for the major amyloid precursors.
Once the histological characteristics of amyloidosis have been established, the type is determined based on immunohistochemical analysis and genetic testing. Immunoelectron microscopy marks amyloid deposits by colocalizing specific proteins with fibrils and can be performed on abdominal fat samples.
Infiltrated tissues show homogeneous eosinophilic hematoxylin and eosin staining. The earliest deposits are usually vascular. In the kidneys they can be mesangial, but at the end of the course the entire glomeruli gradually disappear.
Treatment of renal amyloidosis
In the treatment of secondary renal amyloidosis, the success of treatment of the underlying disease plays a significant role. In the case of complete and permanent cure of the primary pathology, the symptoms of renal amyloidosis often regress. Patients with renal amyloidosis require a change in diet: long-term, for 1.5-2 years, consumption of raw liver (80-120 mg/day), protein and salt restriction (especially in case of renal and heart failure); increased carbohydrate intake; foods rich in vitamins (especially vitamin C) and potassium salts.
Pathogenetic drugs for the treatment of renal amyloidosis are 4-aminoquinoline derivatives (chloroquine), desensitizing agents (chloropyramine, promethazine, diphenhydramine), colchicine, unithiol, etc. Symptomatic therapy for renal amyloidosis includes the prescription of diuretics, antihypertensive drugs, plasma transfusion, albumin, etc. d. The advisability of using corticosteroids and cytostatics is debated. End-stage renal amyloidosis may require chronic renal dialysis or kidney transplantation.
Effective methods and rules of treatment
The main goal of treating amyloidosis is to reduce the formation of amyloid and protect organs from its effects. The process is quite long and complex, depending on the form of the disease, its root cause and the stage of the process. Treatment, unfortunately, is ineffective, especially in the later stages. But eliminating the pathogenesis factors of amyloidosis makes it possible to slow down the process of accumulation of defective protein in the kidneys.
For secondary amyloid dystrophy, drugs are used that are aimed at curing the underlying disease. This can be drug therapy and radical (surgical) methods.
Medications
Pathogenetic therapy involves taking several groups of drugs.
4-aminoquinolines:
- Rezokhin,
- Delagil,
- Chloroquine.
They inhibit the synthesis of polysaccharides and nucleic acids and influence the pathogenesis of amyloid. These drugs are taken for a long time, 0.25-0.5 g per day.
Taking the above medications may cause side effects, including an allergic reaction. At the same time, you need to take vitamins B, C, and desensitizing drugs:
- Suprastin,
- Tavegil,
- Cetirizine.
To inhibit amyloid aggregation, Unithiol 5% is administered intramuscularly once a day for 30-40 days. A good effect is noted in various forms of amyloidosis from the use of the plant cytostatic Colchicine. It is taken for 4-6 months at a dosage of 0.2-0.5 mg per day.
Anabolic steroids affect nitrogen metabolism, improve appetite, and increase body weight:
- Dianabol,
- Nerobol.
For amyloidosis, it is recommended to take raw liver or liver preparations (Sirepar) for a long time. Symptomatic treatment also includes the use of diuretics, antihypertensive drugs, and plasma transfusions.
At a late stage of the disease, conservative methods are ineffective. Hemodialysis becomes vitally important. In some cases, hemodialysis helps prolong the patient's life by several years. But the most effective treatment is kidney transplantation.
How to determine whether your kidneys or back hurt? What is the difference in symptoms? We have the answer!
Read about the symptoms and treatment of hydronephrosis of the right kidney in newborns at this address.
Follow the link https://elesto.ru/lechenie/narodnye/mochegonnye-travy.html and learn about the rules for using diuretic herbs for leg swelling and kidney diseases.
Diet and nutrition rules
Proper nutrition is an integral part of complex therapy for amyloidosis. At the onset of the disease, a low-protein diet is prescribed (0.7 g of protein per 1 kg of weight). Food should be rich in vitamins and complex carbohydrates. The diet should include berries, fruits high in ascorbic acid, as well as dishes with potassium salts (rice, cabbage, raisins, oranges, figs). It is useful to eat watermelon, melon, zucchini, and carrots.
To increase your calorie intake, you can consume marmalade, marshmallows, and vegetable oil. Limit legumes, meat, halva, cheese. In case of edema, reduce the consumption of salt (up to 2-3 g) and liquid (up to 1 liter, including liquid dishes). Your diet must include raw liver.
Forecast and prevention of renal almyloidosis
The prognosis is largely determined by the course of the underlying disease and the rate of progression of renal amyloidosis. The prognosis is worsened by the development of thrombosis, hemorrhages, intercurrent infections, and advanced age. If heart or kidney failure develops, survival is less than 1 year. The conditions for recovery are timely contact with a nephrologist and early diagnosis of renal amyloidosis, active treatment and complete elimination of the underlying disease.
Prevention of renal amyloidosis requires timely treatment of any chronic pathology that can cause the development of amyloid nephrosis.
Treatment approaches
Although there is no etiotropic therapy for amyloidosis, symptomatic drugs can alleviate the course of the disease. Treatment for the primary form often includes chemotherapy, which is used for certain types of cancer. The drugs disrupt the growth of abnormal cells that produce the causative protein. New treatments are studied in a series of tests on different people. Another possibility is stem cell transplantation to replace atypical ones. The procedure is complex and side effects can be very serious (death).
Treatment for secondary amyloidosis is aimed at treating the underlying disease (for example, with an anti-inflammatory medication for arthritis). For inherited disorders, liver transplantation may be a potential therapy, since the responsible proteins for this disorder are often produced in hepatocytes. Again, there is possible drug therapy.
Since amyloidosis can have a number of secondary effects, treatment will be required against them. For example, a low-salt diet if the heart or liver is affected, or prescription of painkillers.
It is important to know! If the liver cells are seriously damaged, an organ transplant is possible. The surgery does not cure the disease, but it can significantly prolong the average life expectancy.
Use of medications
Drug therapy consists of diuretics, antianemic, antihypertensive and other symptomatic drugs. The decision to prescribe drugs, as well as the choice of dose, depends on the medical specialist. In many ways, the duration of therapy is determined by the stage of the incurable disease and the number of years of the patient (different drugs are indicated in old age and childhood). Medicines are often combined to achieve maximum therapeutic effect.
The use of colchicine slows the progression of the idiopathic disorder, but the mechanism of action of the drug is unknown to medicine. It is prohibited to independently treat the pathological condition and clinical manifestations.
Unithiol is able to reduce the formation of amyloids and improve the condition of both children and adult patients. However, it often causes vertigo syndrome, intestinal disorders, tachycardia and other pathologies. The drug can be taken only on the recommendation of a specialist.
Diet and folk remedies
The diet should consist of low-protein foods and low-fat foods. Patients with an established diagnosis need to limit the amount of casein, as it aggravates the course of the disease. All patients should also reduce the concentration of sodium chloride in their diet.
Advice! Patients with morphological kidney damage should avoid using untested medicinal herbs. They can have unpredictable effects and cause a lot of harm if used incorrectly or thoughtlessly. Before use, consult a doctor.
There is no need to follow a specific diet for a pathological condition unless the causative disease requires it.
Surgical intervention
Some men and women may require a surgical procedure. During open surgery, a qualified doctor removes diseased tissue. The doctor is attempting to create new membranes that do not allow beta2-microglobulin to pass through. In most cases, the operation is aimed at treating inflammatory foci and preventing further spread of the infectious disease.
Main reasons
Nephrosis is a multifactorial disease. The most common causes of various forms of the disease:
- Intestinal obstruction;
- Severe injuries;
- Extensive burns;
- Infectious diseases (dysentery, diphtheria, cholera, malaria);
- Heavy metal poisoning (chrome, gold, mercury, lead);
- Chemical intoxication (methyl alcohol, brake fluid, antifreeze);
- Incompatibility of blood during transfusion;
- Compression of tissues.
Causes of primary and secondary nephrosis
Another common name for the disease in medical circles is “toxic-infectious kidney,” which reflects the causal essence of the disease. It is formed against the background of various kinds of poisoning and intoxication. In most patients, it develops against the background of ethylene glycol (antifreeze) poisoning, which is a common substance encountered by motorists. It fills the inside of the battery.
Intoxication with sulfonamide drugs was common 15-20 years ago, when these drugs were used to treat dangerous sexually transmitted infections (syphilis, gonorrhea).
Some bacteria are capable of independently causing necrotic kidney damage. These types include cholera, plague, malaria, and diphtheria.
In some women, the cause of nephrosis is avascular necrosis that occurs after childbirth.
We must not forget about the genetic causes of nephrotic syndrome. If both parents have nephrosis, there is a high probability of the disease developing in children.
Introduction
Kidney amyloidosis is a disease characterized by the accumulation in the kidneys of a special type of insoluble protein that is not produced by the body in healthy people - amyloid. The reason for the deposition of this protein is a violation of protein-carbohydrate metabolism in tissues. This disease often leads to the development of kidney nephrosis and disruption of their functions. Amyloid nephrosis can also trigger the formation of chronic renal failure. The first records of amyloidosis were made more than 150 years ago, but to this day the disease is classified as incurable.
Diagnostics
There are various diagnostic methods for this disease, the most reliable of which is considered to be a patient’s blood test. This method can be used at any stage of renal amyloidosis. It is a blood test that will help identify a sharp increase in the number of platelets with a concomitant decrease in the amount of proteins and hemoglobin. At the same time, an increased level of liver enzyme is observed in the blood serum.
A doctor with extensive experience always begins the diagnostic process by studying the life history of his patient. This helps him determine whether the person suffers from any chronic diseases that could cause further inflammation, and whether the patient's working or living conditions are associated with constant exposure to toxic substances.
Electrocardiogram
Another fairly effective method is an electrocardiogram. Thanks to it, it is possible to detect a slow heartbeat, which is a characteristic sign of renal amyloidosis. If the doctor makes a differential diagnosis, it becomes possible to begin treatment of the disease that provoked amyloidosis.
Another effective diagnostic method is a kidney biopsy, which helps to easily and very accurately determine the amount of amyloid in the tissues of various organs, as well as blood vessels. When carrying out this type of diagnosis, a small piece of tissue is removed through a microscopic puncture for examination under a microscope (the so-called “histological examination”).
The most informative method of these is considered to be microscopy. An examination of various organs using radiography is often prescribed. In addition, in recent years it has become possible to perform computed tomography of the kidneys, which makes it possible to study their structure layer by layer. Unfortunately, even this does not always make it possible to establish the exact causes of the development of amyloidosis in healthy kidneys.
Diet for amyloidosis
All renal pathologies require a diet with reduced consumption of table salt, as well as protein foods.
The diet is designed so that it does not contain red meat and products containing casein. The following are prohibited:
- cheeses;
- cottage cheese and its derivatives;
- milk;
- beef;
- veal.
It is not recommended to include spicy dishes, smoked foods, foods with a high content of dyes and preservatives in the menu. If you are overweight, doctors categorically prohibit baked goods that increase cholesterol levels in the circulatory system.
Despite the restrictions, the patient menu should be varied and nutritious. A serving of meat is calculated based on the amount of protein in it: per 1 kg of a person’s weight, it is permissible to consume no more than 1 g of protein. Cereal products are allowed in large quantities.
Vegetables, fruits and dishes made from them should be consumed raw, steamed or stewed. They are considered a source of vitamins and minerals for people with kidney amyloidosis. To enhance the taste of food, it is allowed to use seasonings: garlic, basil, peppers.
Following simple nutritional rules helps patients improve kidney function and restore good health.