About stenting
A ureteral stent is a special medical device used to remove urine from the lumen of the urinary canal, deformed by a tumor process or blocked by stones. A common cause is also the acute course of an infectious and inflammatory process in the organs and tissues of the urinary tract.
Ureteral stents are made of silicone or polyurethane. The cross-sectional diameter and length depend on the individual characteristics of the patient (age and anthropometric data). Due to the characteristics of the material used, the product bends easily and takes an anatomical shape, which ensures relatively painless installation of the structure. The absolute smoothness of the inner coating ensures the unimpeded flow of urine and neutralizes the negative effect of aggressive urea salts and acids on it.
A silicone stent located in the kidney is less susceptible to destruction and stone deposits, but excessive flexibility complicates the process of installing a system for removing urine. On one edge the product is equipped with a special spiral - a “pig tail”. This structural element provides fixation to prevent accidental migration or prolapse of the stent. Stenting of the right or left ureter occurs through the use of a specialized urological instrument - a ureteroscope or cytoscope.
Attention! Blockage of the ureter and blockage of the unimpeded drainage of urine is life-threatening for the patient. Therefore, renal stenting is often the only effective treatment tactic for certain pathological conditions localized in the urinary system.
Indications
Among the reasons why this treatment tactic is indicated for a patient, there are two main groups. Urological pathologies:
- Urolithiasis (including during pregnancy), with localization of stones in the structure of the kidney or the lumen of the ureter.
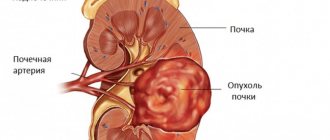
- Malignant processes and benign neoplasms that are located in the organs and tissues of the urinary tract.
- Benign adenoma, oncological pathologies, hyperplastic changes in the prostate gland in men.
- A rare nonspecific inflammatory process in fibro-adipose tissue - Ormond's disease.
- Infectious kidney diseases.
The second group includes all factors not related to urology. These include:
- Metastases or progressive growth of cancer tumors located outside the genitourinary system;
- Consequences of hematological diseases (lymphoma or lymphadenopathy);
- Iatrogenic factors caused by medical personnel. For example, accidental mechanical damage to tissue during surgical interventions on the pelvic organs;
- Postoperative adhesions;
- extensive abdominal surgery;
- Complications of radiotherapy of the pelvic organs.
Contraindications
Before the ureteral stenting procedure, the attending physician carefully studies the data of laboratory tests and additional diagnostic examinations (ultrasound diagnostics, MRI). If the patient has an acute inflammatory or infectious process, the installation of a stent in the kidney should be temporarily postponed. This is a necessary measure to prevent the spread of infection.
Sometimes it is impossible to perform an intervention due to the general severity of the patient’s condition. In this case, after stabilizing the patient, it is possible to install a drainage system to normalize urine output.
There are absolute contraindications to this treatment method:
- Irreversible pathological changes in the ureteropelvic segment;
- Expressed infiltrative - inflammatory reactions in the tissues of the walls of the ureter or kidneys, caused by the presence of impacted or strangulated stones.
The final decision regarding the advisability of installing a stent in each individual case is made solely by the attending physician, taking into account possible risks and complications.
During pregnancy
The wonderful time of pregnancy does not exclude overshadowing influencing factors, and pyelonephritis, unfortunately, is no exception. If a woman has developed problems with the urinary tract before, then under the pressure of the uterus and fetus they only get worse. Therefore, doctors even recommend installing a stent in the ureter during pregnancy.
We advise you to read: Strelnikova gymnastics for nasal swelling
The procedure is performed in the supine position, which is completely safe for the fetus. Under these conditions, stents with antireflux valves are recommended.
A woman can walk throughout her pregnancy and give birth with him. They are usually removed a few weeks after this. This is decided individually with a specific patient.
Women have a stent installed while expecting a child only if indicated. Stenting is temporary and is removed 2-4 weeks after birth. The purpose of the tube during pregnancy is to relieve symptoms and delay surgery.
After stenting the ureter, the urologist needs to monitor the patient throughout the entire period of gestation. The material of the tube plays an important role: it must be hypoallergenic and guarantee 4 to 6 months of safe wearing. If necessary, the device should be replaced. After installation, the pregnant woman is scheduled for monthly ultrasound examinations to monitor the tube.
Kinds
Installation of a renal stent in the urinary tract occurs after a thorough diagnosis, precise determination of the location of narrowing or obstruction of the canal, the location of the tumor or stone. The procedure is performed under aseptic conditions, under anesthesia. Surgery usually lasts no more than 30 minutes.
Depending on the equipment of the clinic, navigation control of the process is possible by displaying images on a monitor, or using X-ray control techniques. In the worst case, the intervention is carried out blindly. Depending on the individual characteristics of the clinical situation, it is possible to perform stenting using one of the methods.
Retrograde introduction
To perform this technique, local anesthesia must be adequate. During the procedure, a special cylindrical design with a small-sized balloon inside is introduced into the urinary canal. The use of a cytoscope provides control over the movement of the stent.
When the optimal position of the drainage system is reached, the doctor levels the mesh, with the help of which it opens and carefully restores anatomical patency. Upon completion of the surgical procedure, the dilating balloon is removed from the urethra, and the stent remains to fix the restored lumen of the ureter.
For diagnostic purposes in the postoperative period, the patient is shown catheterization of the bladder to monitor the characteristics of the discharged urine. Retrograde stenting is indicated for the following pathological conditions:
- urolithiasis disease;
- compaction or adhesions in the tissues of the ureter;
- neoplasms of various etiologies.
Antegrade tactics
In difficult cases, when a non-invasive technique is impossible, stent installation is carried out in a hospital setting through a surgical approach on the anterior surface of the peritoneum. When using this method, the patient makes an incision on the surface of the skin in the area of the projection of the ureter. One end of the stent is inserted directly into the kidney, and the other into a special urine receptacle. In this way, medical personnel can control the amount, shade and composition of urine.
This procedure is performed under x-ray control and using general anesthesia. Often specialists use contrast for better positioning.
It is important to know! At the end of this stage, the stent remains closed for an average of 3 days, after which it is opened. This is necessary for the prevention and timely detection of postoperative complications.
Indications for antegrade administration:
- absolute obstruction of the urethra;
- traumatic injury to the urinary tract;
- complete collapse of the walls of the ureter.
Removing a stent from the ureter
In the absence of undesirable reactions and inflammation, the drainage system is removed after two weeks, but no later than six months from the date of installation.
On average, the tube is replaced after two months.
If lifelong stenting is indicated, the device is changed every 120 days.
Frequent tube changes are necessary to avoid salt occlusions, organ infections, and damage to the ureteral mucosa.
The maximum duration of action of the stent is set by the manufacturer. The doctor takes into account the patient’s age and related factors.
The urinary structure is removed on an outpatient basis in 5 minutes under local anesthesia. This quick process is performed with a cystoscope.
A gel is placed into the urethra to facilitate passage of the device.
Under the control of X-ray equipment, the guide wire is inserted as deep as possible and the tube is straightened.
The outer end of the expander is grabbed and pulled out. The drainage system must be changed every 3–4 months. In people prone to stone formation, the tube is replaced after 3-4 weeks.
When the system is removed, the patient may experience a short-term burning sensation and tolerable pain. After the tube is removed, diagnostics are carried out for four days in order to select further treatment tactics. The patient feels discomfort when urinating for several days after removing the dilator.
Sometimes the stent needs to be removed and reinserted. But basically, while wearing the device, doctors remove the causes of blockage of the canal, and the patient can return to normal life.
Duration of stenting
Regardless of the quality of the materials used for the manufacture of stents, the average service life of this product does not exceed 6 months. After this time, doctors remove the urine drainage system. The procedure for removing a stent from the ureteral canal is carried out without the use of general anesthesia.
If this procedure is not carried out in a timely manner, a secondary ascending infection may occur. This process is characterized by a sharp deterioration in the patient’s well-being, a rise in body temperature to febrile levels. If adequate anti-inflammatory therapy is prescribed, the patient's condition normalizes within 3-5 days.
It is important to know! The stent must be removed strictly within the time frame recommended by the doctor! Delay can be fraught with irreversible necrotic changes in tissues.
Preparing for surgery
In preparation for stenting, the optimal model of the ureteral dilator is determined. For this purpose, ultrasound, excretory urography, and MRI of the excretory system are prescribed.
Features of preparation for stenting:
- 2-3 days before the procedure, avoid alcohol and fried foods;
- on the eve of the operation, an enema is performed to cleanse the intestines of feces;
- To avoid inflammation of the urethra and ureter, antibacterial drugs are prescribed - Furagin, Furadonin.
The procedure is carried out strictly on an empty stomach. If there is increased anxiety, the patient is prescribed sedatives.
Possible complications of the procedure
In some cases, immediately after stenting, patients complain of pain when urinating, frequent urges, accompanied by difficulties in the process of urination.
An intraoperative complication is injury to the tissues of the ureter or bladder. This condition is diagnosed by the presence of blood in the urine.
A rare but possible adverse reaction to the procedure is vesicoureteral reflux, characterized by the reverse flow of urine from the bladder cavity. The development of pyelonephritis is a consequence of this disorder.
Destruction of the stent by urea salts is a consequence of untimely removal of the system. With this disorder, the likelihood of mucosal erosion or the formation of a ureteral fistula increases, which is dangerous for the development of purulent-septic processes.
If the installation technique is not followed or low-quality materials and components are used, the stent may spontaneously migrate and fall out, requiring repeated surgery.
conclusions
Ureteral stenting is often the only chance for a full life in patients with complex pathologies of the genitourinary system. The effectiveness of the procedure directly depends on the implementation of all medical prescriptions.
One of these recommendations is the inclusion of a variety of plant-based products in the patient’s diet and strict adherence to the optimal drinking regime. It is recommended to drink clean water in an amount of at least 2000 ml per day. It is advisable to limit smoked meats and pickles.
In case of a sharp deterioration in the general condition, changes in the color, quantity or smell of urine, you must urgently seek qualified medical help in a specialized urological department. Uncontrolled progression of the inflammatory process is dangerous due to the development of sepsis and possible death.