Modern medicine implies a huge number of nosological forms, which are optimally systematized using the international classification of diseases generally accepted by all WHO countries. This applies to all diseases without exception, so the pathology of the urinary system necessarily has its own subclass within it. A common recurrent problem is chronic cystitis, which many doctors around the world code using the ICD. This facilitates the continuity of medical care, since any doctor, looking at this code, understands what pathology we are talking about. For chronic cystitis, the ICD 10 code is defined in the chapter on diseases of the urinary system.
Classification of diseases at the international level and its tasks
Each of us, at least sometimes, has had to deal with such a procedure as registration of temporary disability. Having recovered from an illness and received sick leave, not everyone pays attention to the fact that in the column in which the cause of incapacity is indicated, there are some incomprehensible designations. They are a disease code that contains the International Classification of Diseases (ICD).
The ICD is a regulation compiled by the World Health Organization. The first attempts to create such a directory were made back in the 18th century, but the first document that was used internationally was developed in 1855.
Since then it has been revised several times. This procedure usually occurs after a ten-year period. Today, medicine is guided by the International Classification of Diseases, 10th revision (ICD 10).
The goals of the ICD are:
- bringing to a unified system of data on morbidity and mortality in the world;
- unification of the process of accumulating knowledge about diseases, as well as their storage, analysis, comparison and interpretation.
These goals are realized by translating verbal definitions of diseases, their causative agents, and other human health problems into a unified system of codes. This way, doctors all over the world understand each other much more easily and develop a unified approach to diagnosing and treating diseases.
How to treat genitourinary disease
Special treatment for cystitis involves an integrated approach, including:
- antimicrobial medical therapy (taking antibiotics);
- taking painkillers and anti-inflammatory drugs;
- immunotherapy (immunity enhancement);
- observing important hygiene rules.
Drug therapy in the fight against cystitis involves taking antibiotics.
The most popular and effective antibiotics in this case are Flemoklav, Levofloxacin, Erythromycin and some others. They have an antibacterial effect on the body and contribute to the complete destruction of pathogenic bacteria.
Along with antibiotics, anti-inflammatory drugs are prescribed. Among them, the most effective are Urolesan, Cyston, etc. They eliminate pain and help relieve the disease.
Doctors often prescribe vitamins along with these medications. They are able to increase a person’s immunity, which means that the body will be able to cope with the illness that arises much faster.
Remember, cystitis is a disease that, if left untreated, can cause serious damage to the bladder and kidneys.
Structure of ICD 10
In the current ICD 10, all information is presented in the form of a tree. All data contained in the document is grouped into 22 classes.
It looks like this:
- classes 1-18 - diseases and all kinds of pathologies;
- class 19 - injuries and other health disorders caused by external factors;
- class 20 - causes leading to morbidity and mortality;
- class 21 - factors that affect human health;
- class 22 - contains codes used for other purposes.
Classes, in turn, are divided into blocks, and the blocks contain disease codes. The disease code may also have several digits separated by a dot. They are used to display the type of disease. If necessary, a special code can be used to designate the causative agent of the disease.
ICD 10 is recognized throughout the world. Its codes are used by doctors from all countries, which allows them to use uniform methods in the treatment of various pathologies.
Is there chronic cystitis?
ICD-10 “dedicates” two separate categories to chronic cystitis. But many doctors say that this form of inflammation is only a signal about the presence of a certain pathology in the body that constantly “stimulates” the infection. In this case we are talking about No. 30.2 - another chronic cystitis.
For example, a woman suffers from seizures for years. She took all possible antibiotics, did rinses, used folk remedies... But cystitis still returns, and the doctor puts a note on the medical card as “chronic”. As practice shows, often behind such a diagnosis lies either a hidden sexually transmitted infection or some anatomical feature, which is why the disease regularly worsens. Therefore, for those to whom the doctor does not offer any “alternative” other than chronic cystitis, it is recommended to change the specialist.
A new doctor will be able to look at the situation from a different angle and prescribe examinations that will help establish the real cause of regular exacerbations. When it is eliminated, you can forget about chronic cystitis.
The classification of diseases undoubtedly makes the work of doctors much easier, but sometimes it turns out to be incomprehensible to patients. Therefore, everyone should have at least basic knowledge about the ICD. At a minimum, you need to understand that the code is easy to decipher: fortunately, it is very easy to find its description on the Internet.
Positioning of cystitis in ICD 10
Class 14 according to the International Classification of Diseases contains information about diseases of the genitourinary system. Since cystitis is essentially an inflammation of the bladder, information about it should be sought here.
Block N30-N39 contains information about diseases of the urinary system. For cystitis, the ICD 10 code is N30. Types of disease are indicated in the next digit of the code after the period.
For cystitis, the encoding is as follows:
- acute cystitis – 0;
- chronic cystitis – 1;
- other cystitis – 8;
- unspecified cystitis – 9.
Such types of diseases as radiation cystitis and trigonitis are excluded from the classification. Since cystitis can be caused by different pathogens, the classification provides the opportunity to indicate them using an additional code. They are combined in block B95-98. But usually they are not indicated during the initial encoding.
Thus, using ICD 10 codes, it is possible to describe in detail the patient’s diagnosis, which can be easily read in a clinic in any country in the world.
What is cystitis?
IF
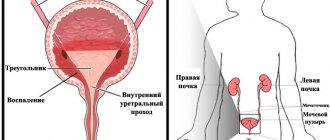
Cystitis is an inflammatory disease that affects the mucous membrane of the bladder. The disease can develop either independently (primary form) or act as a complication of other pathologies of the genitourinary system (secondary form). Cystitis often appears against the background of:
- pyelonephritis (kidney inflammation);
- urethritis (inflammation of the urethra);
- prostatitis (inflammation of the prostate gland in men);
- urolithiasis associated with the presence of stones in the urinary system.
The disease occurs in patients of both sexes, but women encounter it much more often than men due to the peculiarities of the anatomical structure of the body.
Initially, cystitis develops in an acute form. It manifests itself through the following main symptoms:
- Frequent urination both during the day and at night.
- Cutting and burning during urination.
- Inability to completely empty the bladder, constant heaviness in it.
- Changes in the nature of urine (turbidity, the appearance of an unpleasant odor, the presence of impurities in the form of blood, pus or mucus).
If the disease is not treated, it can become complicated. Most often, the disease becomes chronic - then the signs of the disease appear periodically (up to 3-4 times a year), the rest of the time practically without bothering the patient.
Diagnostics
II. METHODS, APPROACHES AND PROCEDURES FOR DIAGNOSIS AND TREATMENT
List of basic and additional diagnostic measures
List of main diagnostic measures: 1. General blood test 2. General urine test 3. Bacteriological culture of urine before, after treatment and during clinical observation with determination of the degree of bacteriuria and sensitivity to antibacterial drugs.
List of additional diagnostic measures: 1. Ultrasound of the kidneys and bladder 2. Cystoscopy 3. Urodynamic studies (uroflowmetry and cystotonometry) 4. Descending and ascending cystography 5. Consultation with a nephrologist
Diagnostic criteria
Complaints and anamnesis: Acute cystitis develops suddenly (over a few hours), manifesting itself in typical cases as burning and/or pain when urinating (dysuria), frequent urgency, pain above the pubis, a slight increase in temperature and nocturia (increased urination at night). Low back pain often occurs, as well as, especially in women, gross hematuria (the appearance of blood in the urine). Acute cystitis recurs quite often, when weeks and months can pass between attacks.
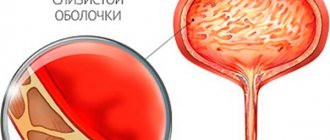
Chronic cystitis refers to a form of the disease in which symptoms persist continuously for many weeks. Chronic cystitis is most often based on deeper (interstitial) inflammation of the bladder tissue. Cystitis often develops within 24 hours after sexual intercourse.
Treatment of exacerbation of the disease
If the recurrence of cystitis is severe, with high fever and severe abdominal pain, the patient is sent to the hospital. After diagnosis and necessary tests, bed rest and antibiotics are prescribed.
In the treatment of acute cystitis, antibiotic therapy is of paramount importance. They are usually prescribed in a course of three to seven days . These are “Norfloxacin”, “Tsiprolet”.
In addition, the following drugs are used:
- Anti-inflammatory drugs. "Diclofenac" in injections or tablets, "Nimulid";
- Antispasmodics. “No-shpa”, “Ketorol”, “Papaverine”.
- Medicinal herbs are actively used in the treatment of the disease. These are preparations from celandine, bearberry, as well as herbal tablets, for example, “Canephron”, “Cyston”.
In children, cystitis is treated with caution. Antibiotics Amoxilav, Cefuroxime, Suprax are prescribed. It is necessary to monitor the manifestation of allergic reactions. To combat the disease, baths are carried out with medicinal herbs: sage, St. John's wort, chamomile. To normalize the color of the baby’s urine, actively give him something to drink (tea, juice, fruit drink).
Remember, it is better to feed less and drink more than vice versa.
The patient must raise the affected immunity. And this can be done by adjusting your lifestyle : eat right, exercise, stop getting nervous over trifles, and take care of hygiene. Adults should carefully choose a sexual partner and use protection, as well as treat infectious diseases in a timely manner.
Classification
Clinical classification:
1. According to the course of the disease: - acute; - chronic.
2. By origin: - primary; - secondary.
3. According to etiology and pathogenesis: - infectious; - chemical; - radial; - parasitic; - for diabetes mellitus; - in spinal patients; - allergic; - exchange; - iatrogenic; - neurogenic.
4. According to the localization and prevalence of the inflammatory process: - diffuse; - cervical; - trigonite.
5. According to the nature of morphological changes: - catarrhal; - hemorrhagic; - ulcerative and fibrous-ulcerative; - gangrenous; - encrusting; - tumor; - interstitial.
Routes of penetration
According to the classification, there are three ways for an infectious agent to enter the body:
- ascending - through the urethra;
- descending - through the kidneys and ureters;
- contact - through blood and lymph.
Most cases are caused by hypothermia, so the disease develops ascending through the urethra. In childhood, contact type of infection is almost impossible.
Acute cystitis and its treatment
Acute cystitis is a form of inflammation of the mucous membrane of the bladder. It is practically not accompanied by disruption of tissue structure and changes in organ function. Women and girls suffer more. In men it is observed less frequently due to the anatomical features of the structure of the urethra.
The main reason is infection on the inner shell, which lacks protective properties. To cure the disease, it is necessary to know exactly which microorganism caused cystitis. This information is obtained by the attending physician after examining the patient’s urine and bacteriological culture.
Differences in anatomical structure and features of pathogenesis
Bladder infection occurs in three ways:
- ascending - from the urethra upward;
- descending - with the development of pyelonephritis in the kidneys in the direction of urine flow;
- hematogenous - with blood from old or untreated foci of infection.
In severe forms, inflammation is not limited only to the internal epithelium, but also affects the submucosal layer, the detrusor.
In adults, inflammatory diseases of the nasopharynx, carious teeth, cholecystitis, genital infectious diseases, furunculosis, and tonsillitis become chronic foci. For children, it is more typical to be accompanied by tonsillitis, measles, enterocolitis, and helminthic infestation.
To treat cystitis, our readers successfully use Galina Savina’s method
This cheap odorous remedy will get rid of cystitis forever! Sold in every pharmacy, called...
Male cystitis (including boys and adolescents) occurs less frequently because the longer urethral canal protects the bladder from pathogenic microorganisms.
The course and treatment of the disease is complicated by any processes that compress the urinary tract and lead to stagnation of urine. In pregnant women, this organ becomes an enlarged uterus. For men, obstruction to the flow of urine creates swelling and growth of the prostate. The greater the degree of adenoma, the narrower the urethral meatus becomes.
For persons of both sexes the following are important:
- urolithiasis disease;
- congenital anomalies of the urethra and bladder;
- formation of reflux urine flow against the main direction;
- bladder hyperactivity;
- disruption of nerve connections and interactions at the level of the spinal nodes in the sacral region.
The outflow of urine not only removes unnecessary substances and waste, but also washes the inner lining of the bladder. It is strengthened by mucopolysaccharide secretion, forming a thin protective layer. It is called glycocalis. The most important function is to prevent microorganisms from attaching to the wall and retaining them. The production of cells in this layer is controlled by the hormones estrogen and progesterone.
Varieties
According to the statistical classification of ICD-10, acute cystitis is included in diseases of the urinary organ with code N30.0. For cystitis of radiation etiology, code 30.4 is provided.
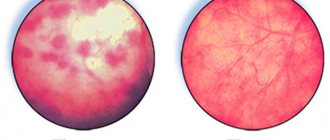
An endoscopic study of the condition of the mucous membrane during cystitis made it possible to identify the following forms:
- catarrhal - there is swelling, hyperemia, dilated blood vessels;
- hemorrhagic - the permeability of blood vessels is impaired, red blood cells sweat through them;
- granular and bullous - inflammation penetrates the muscle layer, disrupts the nutrition of the bladder wall;
- encrusting - expressed in mechanical damage to the epithelium by various crystals.
It is customary to distinguish:
- primary inflammation - there is no mention of earlier pathology of the bladder;
- secondary - before cystitis there were already other diseases of the urinary system.
Depending on the prevalence of the process, acute cystitis can:
- remain focal, for example, cervical localization;
- have a diffuse nature (total damage to the entire bladder).
Causes of the disease
The causes of acute inflammation of the bladder in childhood often lie in:
- violation of hygiene rules, failure to clean the anus after defecation, washing the child, changing linen;
- boys more often have vesicourethral congenital changes (phimosis, urethral stenosis, bladder wall diverticulum, cervical sclerosis);
- in girls, vaginal dysbiosis occurs when treated with various medications;
- neurogenic dysfunction.
The main and immediate cause of inflammation is pathogenic microorganisms. They are divided according to coloring methods into:
- gram-negative (Escherichia coli, Klebsiella, Proteus);
- gram-positive (staphylococci, streptococci, enterococci).
Associations of microorganisms that enhance the inflammatory response are often found.
Acute cystitis in men and women is associated with promiscuous intimate life. Among the pathogens are:
- gonococci,
- Trichomonas,
- chlamydia,
- uroplasma.
Such acute cystitis is called specific. For their therapy, agents with particular sensitivity to sexually transmitted infections are used. Specific inflammation is caused by the causative agent of tuberculosis - mycobacterium. It enters the bladder secondarily from a source in the lungs and kidneys.
Hemorrhagic forms can be caused by:
- adenoviruses,
- herpes,
- parainfluenza.
Viruses typically involve disruption of blood microcirculation, destruction of innervation, followed by a bacterial infection or fungi.
Other causes and factors for the development of acute cystitis:
- injury to the inner membrane of the bladder during cystoscopy, catheterization, ureteroscopy;
- frequent viral diseases and radiation therapy significantly reduce local immunity (cells in the submucosal layer are inhibited);
- the influence of the irritating effect of toxic substances on the urinary organs in case of poisoning;
- the disturbance of blood circulation in the bladder wall is facilitated by general stagnation of blood, in particular in the pelvis;
- metabolic changes cause the deposition of salt crystals with the formation of stones, which constantly irritate the mucous membrane.
Clinical manifestations of different forms
Symptoms of acute cystitis depend on:
- prevalence of the inflammatory process;
- depth of damage to the submucosal layer;
- degree of vascular involvement.
Classic manifestations are:
- frequent, unbearable urge to urinate - the normal frequency is considered to be up to 8 during the daytime and 2 at night; with acute cystitis, patients literally have to run to the toilet 2-3 times an hour;
- release of small portions of urine due to increased reflex excitability of the detrusor muscle;
- cramps and pain at the end of urination;
- the appearance of blood at the final stage of urine excretion;
- impaired transparency (cloudness) of urine, formation of clots such as “meat slop”.
Pain in the suprapubic region radiates to the groin, perineum, anus, and in men - to the penis and scrotum. Constant pain is caused by the cervical form. The intensity reaches the clinical picture of an attack of cystitis. At the same time, a sharp spasm of the external sphincter in the urethra together with the pelvic floor muscles is caused.
Not all symptoms are always present:
- damage to the bladder neck is accompanied by urinary incontinence;
- in severe cases, with a diffuse process, body temperature rises, chills appear, this serves as a sign of ascending infection of the kidneys and the onset of pyelonephritis;
- hemorrhagic form or acute cystitis with blood not only at the end of urination occurs with a viral etiology, when disturbances in the vascular wall cause the release of red blood cells into the urine;
- granular and bullous cystitis - severe suppuration is accompanied by an unpleasant putrid odor of urine, intoxication, and severe constant pain.
Features during pregnancy
Acute cystitis is experienced by up to 10% of pregnant women. Its occurrence is facilitated by:
- dysbacteriosis of the vaginal flora;
- the presence of chronic foci of infection;
- hormonal changes;
- mechanical compressive effect of the growing uterus on the bladder.
In case of a short pregnancy, the cause of cystitis can be allergens from cosmetics, hygiene sprays, shower gels, bath foam, food (cabbage, nuts, legumes, chocolate). Allergic manifestations occur against the background of significant suppression of the immune system due to the physiological state of the woman. Even overwork can cause acute cystitis.
The causative agents of cystitis and clinical manifestations do not differ from the classical course. There is an opinion among young women that increased frequency of urination is always associated with cystitis, but this is not true. In the early stages of pregnancy, when the fetus is implanted into the wall, the uterus becomes more excitable. It is connected by nerve fibers to the bladder and transmits its tension to it. Therefore, urination becomes more frequent.
If there is no pain or stinging, then the symptom cannot be considered cystitis, much less begin treating the woman on her own. Usually urination returns to normal by the twelfth week.
On the contrary, if pain or cutting occurs simultaneously with urination at any stage of pregnancy, you must tell your obstetrician-gynecologist about it. Such symptoms are more likely to indicate the onset of inflammation. The development of diffuse cystitis must not be allowed; at home, therapy with herbal remedies should be started as prescribed by a doctor.
Features of manifestations in children
Acute cystitis is more common among girls under 7–8 years of age. In the first year of life, children of both sexes are affected with equal frequency. Anatomical changes and routes of infection are important.
A significant role in the loss of bladder protection in childhood is played by:
- insufficient local immunity (decrease in the level of substances involved in local immune reactions, immunoglobulin A, interferon, lysozyme);
- neurogenic dysfunction between the detrusor muscle and sphincters, which contributes to an increase in pressure inside the urethra and the occurrence of infection in the bladder.
For young children, the more typical pathogens are Klebsiella and Proteus. The importance of microbial associations such as:
- E. coli + staphylococcus;
- Escherichia coli + streptococcus;
- chlamydia + bacteria.
Infection of a child with chlamydia occurs in families that do not observe basic hygiene rules (one towel, bathing and sleeping with adults), when visiting a swimming pool or bathhouse.
Children with congenital defects of the urinary organs suffer from cystitis more often. If a child suffers from systemic lupus erythematosus, then cystitis is regarded as part of a general lesion of the serous membranes (polyserositis).
Eosinophilic cystitis occurs in children with parasitic diseases (helminthic infection). This form is characterized by pain and a decrease in bladder volume. Clinically manifested by hematuria and urinary incontinence.
In young children, the symptoms of acute cystitis can be judged by:
- I cry while urinating;
- increased irritability;
- refusal to eat;
- increase in body temperature.
How is acute cystitis diagnosed?
Typically, diagnosis is not difficult for a doctor. Having identified the characteristic set of symptoms, it is highly likely that inflammation of the bladder can be assumed. Additional studies should confirm or refute the doctor’s opinion and help establish the form of the disease. This will prompt the optimal choice of treatment for acute cystitis.
Laboratory indicators of inflammation are combined into urinary syndrome. This includes:
- growth of leukocytes in the field of view due to neutrophils, can cover the entire observed space;
- red blood cells for hematuria;
- the sediment contains a large number of transitional epithelial cells in mucus and bacteria.
Protein (proteinuria) with isolated cystitis is absent or a small increase is manifested. A significant increase indicates damage to the tubular apparatus of the kidneys - pyelonephritis.
To identify a specific infectious pathogen, a bacteriological study is carried out by inoculation on nutrient media. If a sexually transmitted infection is suspected, the polymerase chain reaction may be used.
An important point in urine testing is preparation. Before collecting urine, men and women should wash themselves well with soap, women and girls from front to back, and men and boys should thoroughly wash the preputial fold. Only morning urine is suitable for analysis.
To diagnose the level of bacteriuria, a two-glass test is done, Nechiporenko analysis.
Taking urine with a catheter is undesirable due to the provocation of inflammation. The bladder puncture method is used only for acute urinary retention.
Cystoscopy and cystography are performed after acute cystitis has subsided.
Women need to consult a gynecologist to identify chronic infection in the genitals.
In men, prostate secretions are examined and a smear from the urethra is cultured.
What diseases are used for differential diagnosis?
In differential diagnosis, the doctor must exclude:
- acute pyelonephritis;
- appendicitis (taking into account the possibility of atypical localization of the appendix);
- paraproctitis;
- formation of stones in the bladder;
- tumor process.
Treatment of acute cystitis
Only a specialist doctor can determine how to treat acute cystitis, taking into account the patient’s age, concomitant diseases, and the presence of pregnancy.
Most often, treatment is carried out at home (outpatient). Cases of severe disease, severe intoxication, and suspected cases of acute pyelonephritis are subject to hospitalization. The attending physician will advise the patient what to do. Necessary:
- lie down more;
- drink up to 2.5 liters of liquid;
- Avoid foods that irritate the urinary tract (spicy foods, smoked foods, alcohol, coffee, fried meats);
- eat vegetable and dairy dishes, boiled meat;
- during the period of therapy you will have to abstain from intimacy;
- pay attention to regular bowel movements.
Drugs to treat acute bladder inflammation include:
- antibacterial agents (antibiotics, sulfonamides, nitrofurans, fluoroquinolones);
- antispasmodics (Platifillin, No-shpa);
- non-steroidal drugs (Diclofenac, Ibuprofen);
- corticosteroids for eosinophilic cystitis;
- herbal remedies.
Of the antibiotics, cephalosporins have an advantage; they exhibit a wide-ranging effect on various microorganisms. If it is ineffective, you have to change the drug to another.
The course of therapy usually lasts 7–10 days. There is a medicine with a rapid anti-inflammatory effect - Monural. It is taken once, rarely the doctor prescribes a second dose after 2 days. The drug helps relieve the symptoms of cystitis in one day.
Physiotherapy procedures are not prescribed immediately, but after the acute phenomena have subsided. Effective:
- UHF therapy,
- electrophoresis,
- exposure to ultrasound,
- magnetotherapy.
Warming home treatments are limited to temperatures no higher than 38 degrees; hot baths are contraindicated. You can place a heating pad on the suprapubic area.
For herbal medicine, herbal decoctions with diuretic and antiseptic properties are used:
- bear ears,
- lingonberry leaves,
- kidney collection.
There are ready-made preparations from plant materials in combination with vitamins such as Phytolysin, Monurel, Canephron. Their use should be discussed with your doctor.
How to help with pain?
Acute inflammation is accompanied by pain. When it moves to the neck of the bladder, the pain can be spastic and intense, manifesting itself in attacks. Dysuric phenomena recede into the background.
If symptoms increase, the patient should go home. You need to call a doctor or an ambulance. Before arriving, you should try to give yourself first aid:
- try to lie down;
- to warm up, take foot baths and sit in warm water;
- put warm socks on your feet and cover yourself with a blanket;
- Brew and drink tea with medicinal herbs, or, if they are unavailable, use plain warm water.
The ambulance doctor will help relieve the attack by intramuscular injection of a solution of Platiphylline, Atropine, and sometimes Baralgin is used. You cannot take antibiotics on your own.
Features of treatment for pregnant women and children
For pregnant women, there are many restrictions on medications due to toxic effects on the fetus. Treatment of cystitis requires caution.
Usually safe herbal medicines and diet are prescribed. If the symptoms disappear, then herbal treatment continues until urine tests normalize. Antibacterial agents are prescribed if pyelonephritis is suspected, and the woman is hospitalized in the pathology department.
It is necessary to comply with strict requirements for a dairy-vegetable diet, increase drinking through cranberry juice, warm mineral water.
Antispasmodics are prescribed in rectal suppositories. Cephalosporins, fluoroquinolones, and Co-trimoxazole are used as antibacterial therapy in pediatrics.
What to do for prevention?
People who have once suffered acute cystitis should think about their protection from infection and the disease becoming chronic. For this:
- do not overload the body with unhealthy food and alcohol;
- consume more vitamins, fruits and vegetables;
- engage in physical exercises to strengthen the pelvic floor muscles;
- cure different foci of infection;
- be selective about your sexual partners;
- dress warmly in the cold season;
- take care of personal hygiene and underwear.
To prevent acute cystitis, you should promptly get rid of any infectious process in the throat, intestines, or mouth. If a doctor prescribes a course of treatment, then it cannot be interrupted or violated. The risk of transition to a chronic form of the disease depends on this.