Pseudomonas aeruginosa infection is quite dangerous and aggressive, with a high incidence among the population. Up to 20% of all hospital-acquired or nasocomial infections are caused by Pseudomonas aeruginosa. Up to 35% of urinary system infections are caused by this stick, as well as 25% of purulent surgical processes. A quarter of cases of primary bacteremia are also caused by P. aeruginosa.
Pseudomonas infection is an acute infectious disease caused by microorganisms of the genus Pseudomonas, affecting the respiratory system, gastrointestinal tract, soft tissues, nervous and other systems of the body.
Pseudomonas aeruginosa (Pseudomonas aeruginosa) is an opportunistic microorganism of the genus Pseudomonas (pseudomonas). It is a gram-negative (Gram stain does not produce a purple stain) rod-shaped bacterium with rounded ends, 0.5 to 1 µm in size.
Pseudomonas aeruginosa
It is mobile, does not have a dense capsule, does not form spores. It is an obligate aerobe (reproduces with access to oxygen and high humidity). During bacteriological examination, it grows on special nutrient media (meat-peptone agar - MPA, meat-peptone broth - MPB and others), where, as it grows, bluish-greenish colonies with a glow (fluorescent) appear, smelling of jasmine. It has somatic O- and flagellar H-antigens, as well as a capsular K-antigen. The H-antigen (flagellate) allows the isolation of about 60 serovars of Pseudomonas aeruginosa. It is quite resistant to the action of many disinfecting solutions, in some of which it can multiply. Only a 5% solution of chloramine, a 3% solution of hydrogen peroxide and a 2% solution of phenol (carbolic acid) have a detrimental effect on it. In nature, it is found in soil, open water, and on plants. The optimal growth temperature is 37°C.
Pseudomonas aeruginosa can be pathogenic for humans. It often occurs in inflammatory processes (purulent wounds, abscesses), and often causes urinary tract and intestinal infections. It causes nosocomial infections with a high frequency due to its prevalence in people with immunodeficiencies (chronic diseases, surgical interventions, infections and others). Pseudomonas aeruginosa can be found in the human respiratory tract, large intestine, external auditory canal, as well as on the surface of the skin in the folds (axillary, inguinal). With normal immunity, Pseudomonas aeruginosa encounters competitive resistance from representatives of normal flora, which suppress its growth and cause death (for example, in the intestines).
The pathogenicity factors of Pseudomonas aeruginosa are: 1) motility due to flagella; 2) the ability to produce toxins (endotoxin, exotoxin, endohemolysin, leukocidin enzyme), which cause damage to red blood cells, liver cells, triggering intoxication, and death of leukocytes in foci; 3) high resistance to a number of antibacterial agents due to the ability to form a mucus-like capsule around its colonies - glycocalyx (in particular, it is resistant to beta-lactams, aminoglycosides, fluoroquinolones), which complicates the effectiveness of therapeutic measures in such patients.
Pseudomonas aeruginosa (pseudomonas infection)
Pseudomonas aeruginosa infection is quite dangerous and aggressive, with a high incidence among the population. Up to 20% of all hospital-acquired or nasocomial infections are caused by Pseudomonas aeruginosa. Up to 35% of urinary system infections are caused by this stick, as well as 25% of purulent surgical processes. A quarter of cases of primary bacteremia are also caused by P. aeruginosa.
Pseudomonas infection is an acute infectious disease caused by microorganisms of the genus Pseudomonas, affecting the respiratory system, gastrointestinal tract, soft tissues, nervous and other systems of the body.
Pseudomonas aeruginosa (Pseudomonas aeruginosa) is an opportunistic microorganism of the genus Pseudomonas (pseudomonas). It is a gram-negative (Gram stain does not produce a purple stain) rod-shaped bacterium with rounded ends, 0.5 to 1 µm in size.
Pseudomonas aeruginosa
It is mobile, does not have a dense capsule, does not form spores. It is an obligate aerobe (reproduces with access to oxygen and high humidity). During bacteriological examination, it grows on special nutrient media (meat-peptone agar - MPA, meat-peptone broth - MPB and others), where, as it grows, bluish-greenish colonies with a glow (fluorescent) appear, smelling of jasmine. It has somatic O- and flagellar H-antigens, as well as a capsular K-antigen. The H-antigen (flagellate) allows the isolation of about 60 serovars of Pseudomonas aeruginosa. It is quite resistant to the action of many disinfecting solutions, in some of which it can multiply. Only a 5% solution of chloramine, a 3% solution of hydrogen peroxide and a 2% solution of phenol (carbolic acid) have a detrimental effect on it. In nature, it is found in soil, open water, and on plants. The optimal growth temperature is 37°C.
Pseudomonas aeruginosa can be pathogenic for humans. It often occurs in inflammatory processes (purulent wounds, abscesses), and often causes urinary tract and intestinal infections. It causes nosocomial infections with a high frequency due to its prevalence in people with immunodeficiencies (chronic diseases, surgical interventions, infections and others). Pseudomonas aeruginosa can be found in the human respiratory tract, large intestine, external auditory canal, as well as on the surface of the skin in the folds (axillary, inguinal). With normal immunity, Pseudomonas aeruginosa encounters competitive resistance from representatives of normal flora, which suppress its growth and cause death (for example, in the intestines).
The pathogenicity factors of Pseudomonas aeruginosa are:
1) motility due to flagella;
2) the ability to produce toxins (endotoxin, exotoxin, endohemolysin, leukocidin enzyme), which cause damage to red blood cells, liver cells, triggering intoxication, and death of leukocytes in foci;
3) high resistance to a number of antibacterial agents due to the ability to form a mucus-like capsule around its colonies - glycocalyx (in particular, it is resistant to beta-lactams, aminoglycosides, fluoroquinolones), which complicates the effectiveness of therapeutic measures in such patients.
When and which doctor to contact
If the test result is positive for Pseudomonas aeruginosa, you should consult a doctor in any case to prescribe medications that prevent or suppress the growth of the bacterium.
What results require treatment?
You can understand that urgent treatment is needed by the following indicators of the content of Pseudomonas aeruginosa in the samples:
- in sputum – more than 105;
- in wound discharge – more than 104;
- in urine – 105;
- in vaginal discharge – 103;
- in the blood - in any quantity.
If a bacterium is detected in the blood, and not antibodies to it, this indicates blood poisoning, or sepsis. This condition is very dangerous and requires immediate treatment.
Which specialists should I contact?
An infectious disease specialist is involved in the diagnosis and treatment of a patient in whom the presence of Pseudomonas aeruginosa has been detected. It is he who prescribes drugs selected taking into account the bacteriological tests carried out.
However, in some cases, it may be necessary to consult other specialists who will prescribe concomitant treatment:
- if the gastrointestinal tract is affected, you should contact a gastroenterologist to improve digestion;
- to treat pathologies of the genitourinary system, you will need a consultation with a urologist or gynecologist, who, after a series of tests, will prescribe appropriate treatment;
- for diseases of the ENT organs, an examination by an otolaryngologist is necessary;
- To clean purulent wounds and speed up epithelization of tissues without scarring, in addition to systemic treatment, antibacterial solutions and ointments are used, which are prescribed by a dermatologist.
In addition, in severe cases, consultation and treatment with a cardiologist, neurologist and other specialized specialists may be necessary.
Symptoms of Pseudomonas Infection
Pseudomonas aeruginosa can cause inflammation of many organs and systems; we will consider only its most frequent manifestations.
Pseudomonas aeruginosa infection of the gastrointestinal tract is characterized by the appearance of acute enterocolitis or gastroenterocolitis. The severity of the manifestations depends both on the patient’s age and on the initial state of the immune system and the intestines themselves. Thus, in older children and adults, an acute onset with vomiting, pain in the stomach (epigastric region), and then throughout the abdomen, weakness, poor appetite, nausea, temperature is often low-grade (up to 38°), stool up to 5-7 times. per day, mushy, with pathological impurities (mucus, blood), brownish-greenish in color. The duration of the illness is no more than 3-4 days. Children of early childhood experience a more severe infection - a higher temperature (up to 39°), frequent regurgitation or vomiting, refusal to eat, lethargy, frequent loose stools up to 6, and sometimes up to 10-15 times a day, stools are also greenish with pathological impurities (mucus, blood), has a characteristic fetid odor, bloating, loud rumbling. Along with the acute course, there are variants with mild symptoms, but the disease itself lasts up to 4 weeks. A peculiarity in early childhood is the risk of developing intestinal bleeding, dehydration, and at an older age – appendicitis and cholecystitis. A concomitant disease with intestinal damage is the development of dysbiosis, which requires long-term therapy during the rehabilitation period.
Pseudomonas aeruginosa urinary tract infection (UPI) is manifested by the occurrence of cystitis, urethritis, and pyelonephritis. Infection occurs in the urinary system more often during catheterization of the bladder. Symptoms of specific diseases are similar to those of other infections. In most cases, UTI infection occurs chronically over several months or even years. In rare cases, infection from this primary focus spreads to other organs and tissues.
Pseudomonas aeruginosa infection of the respiratory system often develops against the background of chronic bronchopulmonary disease (bronchitis, cystic fibrosis, bronchiectasis); patients in intensive care units (on artificial ventilation, after endotracheal intubation) are also at risk. It is possible to develop both primary pneumonia and secondary pneumonia, which is characterized by a protracted course, poor effectiveness of antibacterial therapy, and a tendency to destructive processes. Symptoms of pneumonia are similar to those of other lung infections.
Pseudomonas aeruginosa infection of soft tissues and skin occurs in places of open wounds, burn surfaces, wounds after surgical interventions, trophic ulcers on the extremities. You can understand that a pseudomonas infection is developing by the discharge from the wound, which becomes blue-green in color. This is the color the patient’s wound dressing will be.
Also, with wounds, the development of pseudomonas osteomyelitis (bone tissue damage) is possible.
Pseudomonas aeruginosa infection manifests itself in the form of purulent external otitis, in which there is pain in the ear, purulent discharge mixed with blood, and less commonly, otitis media and mastoiditis (inflammation of the mastoid process) develop.
Pseudomonas aeruginosa eye infection develops as a result of eye surgery or traumatic injury. Purulent conjunctivitis may develop, and damage to the cornea and the eyeball itself may occur. At the same time, patients have a feeling of a “foreign body” in the eye, pain, blurred vision, and purulent discharge.
Pseudomonas aeruginosa infection of the nervous system occurs in neglected patients and is one of the severe manifestations of this disease. Meningitis (inflammation of the pia mater), meningoencephalitis (damage to the brain substance) may develop. In most cases, the infection is introduced from the primary focus during a septic process. Primary reproduction of Pseudomonas aeruginosa in the central nervous system is possible after injuries and surgical interventions. A typical picture is purulent meningitis or meningoencephalitis, which is practically no different from other infections. With lumbar puncture - a high content of cells in the cerebrospinal fluid (pleocytosis) up to several thousand per ml, a predominance of neutrophils over lymphocytes, a high protein content, the liquid when flowing out is cloudy with greenish flakes. The prognosis is often unfavorable.
Other manifestations of Pseudomonas aeruginosa infection include endocarditis (damage to the cardiovascular system), arthritis, sinusitis, frontal sinusitis, sinusitis and, finally, sepsis - a generalized Pseudomonas aeruginosa infection affecting many organs and systems.
Summarizing the above, we can highlight the important features of Pseudomonas aeruginosa infection:
— In acute cases, there is a high frequency of unfavorable outcomes due to the high resistance of P. aeruginosa to a number of antibacterial drugs, which creates difficulties in treatment and causes lost time.
— Tendency to a protracted and chronic course of infection with frequent relapses of varying severity, which requires long-term treatment.
Indications for analysis
Pseudomonas aeruginosa can exist in the body for years without manifesting itself. According to statistics, approximately 15% of people were carriers of Pseudomonas aeruginosa, but did not suspect it until a certain moment. As soon as local or general immunity decreases, pseudomonas begins to actively reproduce, leading to extremely dangerous consequences for health.
A test for Pseudomonas aeruginosa must be taken if certain signs appear. To do this, you should contact an infectious disease doctor, who will prescribe treatment if necessary.
There are categories of people who are tested for the presence of Pseudomonas aeruginosa bacteria, regardless of whether they have any characteristic signs. This includes people with immunodeficiencies and reduced immunity. These are patients diagnosed with diabetes mellitus, cystic fibrosis, chronic diseases in the acute stage, HIV-infected people, and cancer patients.
An analysis for Pseudomonas aeruginosa is mandatory so that, if necessary, treatment can be started immediately, since the body cannot cope with the bacteria on its own; they begin to multiply much faster. This leads to a rapid progression of the disease and more serious complications.
Diagnosis of Pseudomonas aeruginosa infection
1) Preliminary diagnosis is difficult, since clinically specific symptoms for
There is no Pseudomonas infection. Warning factors regarding P. aeruginosa are the protracted course of the infection despite the ongoing antibacterial therapy, which is not successful, as well as the connection between the occurrence of the infection and medical procedures in hospitals, surgical interventions, and injuries.
2) The final diagnosis is made after a laboratory examination. Lead method
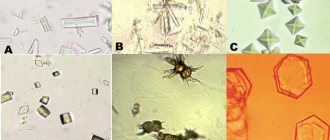
examination - bacteriological followed by bacterioscopy. The material for research can be anything depending on the clinical form - from nasopharyngeal mucus and feces to urine, cerebrospinal fluid, discharge from wounds. It is advisable to collect the material before the start of the antibacterial study. The material is inoculated on a special nutrient medium, where blue-green colonies with fluorescence are grown, and then they are examined under a microscope.
P. aeruginosa colonies
Pseudomonas aeruginosa during bacterioscopy
Usually, another study is immediately carried out - an antibiogram (determination of sensitivity to certain antibacterial drugs).
An additional research method is serological blood testing for antibodies to P. aeruginosa, which is used mainly retrospectively (that is, to confirm infection).
General clinical methods (urinalysis, blood analysis, biochemistry, and so on), as well as instrumental research methods, help the doctor to diagnose only the clinical form of Pseudomonas aeruginosa infection.
1) Organizational and routine measures are reduced to hospitalization of patients with severe manifestations of infection in any hospital according to the profile. Bed rest for the entire period of intoxication.
2) Drug treatment.
Etiotropic therapy is quite complex for Pseudomonas aeruginosa infection.
The frequency of occurrence of antibiotic-resistant strains of P. aeruginosa is high. Despite this, there are certain groups of antibacterial drugs or their individual representatives within the group, which have retained their effectiveness for Pseudomonas aeruginosa infection. These include some cephalosporins (ceftazidime, cefepime), carbapenems (imipinem, carbapinem), a modern aminoglycoside (amikacin), and some fluoroquinolones (ciprofloxacin). P. aeruginosa has been proven to be resistant to tetracyclines and rapidly develop resistance to fluoroquinolones (levofloxacin and others).
Pathogenetic therapy and syndromic therapy are prescribed depending on the clinical manifestation of Pseudomonas aeruginosa infection.
Treatment
Etiotropic treatment of Pseudomonas aeruginosa infection in children: the drugs of choice are carboxy- and ureidopenicillins (carbenicillin, ticarcillin, piperacillin, mezlocillin), cephalosporins of III and IV generations (cefoperazone, ceftazidime, ceftizoxime, cefepime) and aminoglycosides of II-III generations (gentamicin, tobramycin, amikacin , netilmicin).
For mild intestinal infections, polymyxin M sulfate and nitrofurans are prescribed for treatment; for sepsis and pneumonia, a combination of penicillins, cephalosporins with aminoglycosides is indicated. Reserve drugs are monobactams (aztreonam), carbapenems (thienam, meropenem), fluoroquinolones (ciprofloxacin, lomefloxacin, rufloxacin, etc.). An effective remedy in the fight against Pseudomonas aeruginosa infection is hyperimmune anti-pseudomonas donor plasma. Treatment includes stimulants (immunoglobulin, methyluracil), probiotics, bacteriophages (pyocyoneus, pyobacteriophage, intestibacteriophage) and enzyme preparations.
Treatment prognosis
. In severe intestinal infections, meningitis, pneumonia, sepsis, mortality reaches 75% or more.
Prevention
Pseudomonas aeruginosa infection consists of carefully observing the anti-epidemic regime, especially in hospital conditions, using modern antiseptics for disinfection and changing them regularly.
Prevention of Pseudomonas aeruginosa infection
The main preventive measures come down to the prevention of immunodeficiencies (timely treatment of chronic diseases, chronic infections), the prevention of colds. Prevention of infection in children, for which the parents themselves are sometimes to blame (promoting the baby’s health, monitoring nutrition, water consumption, swimming in open water). Prevention of nosocomial transmission of infection usually depends only on medical personnel.
Infectious disease doctor N.I. Bykova
Source: https://www.medicalj.ru/diseases/infectious/1044-sinegnoinaya-palochka
Pseudomonas aeruginosa - the cause of Pseudomonas aeruginosa infection
Pseudomonas aeruginosa
(Pseudomonas aeruginosa) is a mobile microbe that requires the presence of oxygen for its development, has a capsule (it protects the microbe from absorption by leukocytes), and does not form spores.
The bacterium
is particularly resistant to a large number of antimicrobial drugs.
This is a conditionally pathogenic microorganism for humans, i.e. living in the body and capable of causing an infectious disease under certain conditions. Pseudomonas aeruginosa can be found in the normal microflora of some areas of the skin (groin and axillary area, parotid area, etc.). The bacterium causes disease in weakened people with massive contamination of the body and with impaired immunity.
Pseudomonas aeruginosa secretes exotoxins (released during the life of the microbe) and endotoxins (formed when the bacterium dies). In addition, Pseudomonas aeruginosa produces a number of enzymes. Toxins and enzymes cause pathological changes in the human body during the development of an infectious process: destruction of erythrocytes and leukocytes, necrosis of liver cells, vascular damage and others.
Pseudomonas aeruginosa causes Pseudomonas aeruginosa infection
with damage to various organs and systems. The localization of the lesion depends, first of all, on the route of penetration of the microbe into the human body. The causative agent of Pseudomonas aeruginosa infection can be found in open water bodies (contaminated with sewage), in soil, and in the gastrointestinal tract of animals, birds and humans.
Pathogenicity
The risk of developing pathologies caused by Pseudomonas aeruginosa is especially high in patients with weakened immune systems. The bacterium is considered opportunistic. If the body's resistance is sufficiently high, its reproduction is competitively blocked by normal microflora.
The pathogenicity of the bacterium is due to factors such as its high mobility and the production of a number of toxins, leading to disruption of the functions of blood cells (erythrocytes), damage to hepatocytes (liver cells) and the destruction of leukocytes that accumulate in areas of inflammation. Resistance to many antibiotics is explained by the fact that bacterial colonies can form a special protective capsule around themselves.
Routes of transmission of Pseudomonas aeruginosa
Source of infection
are humans and some animals sick with Pseudomonas aeruginosa infection, or carriers of bacteria (Pseudomonas aeruginosa). Patients with pneumonia are especially at risk. caused by Pseudomonas aeruginosa, and patients with purulent wounds.
Infection with Pseudomonas aeruginosa can occur through household contact, food and airborne routes.
The predominant route of infection is domestic
. In this case, household items can serve as factors for transmitting infection. The main ones are: towels, door handles, sinks and taps, toilets, shaving brushes. Rarely encountered factors: instruments, equipment, hands of medical personnel, insufficiently disinfected or treated with disinfectant solutions that turned out to be ineffective against Pseudomonas aeruginosa.
By food route
infection with Pseudomonas aeruginosa is associated with consumption of food products (meat, milk) or water that contain the microbe.
By airborne droplets
infection occurs when inhaling air containing the pathogen (if sanitary and hygienic standards are not observed or if the bacteria is insensitive to disinfectant solutions).
Entrance gate
for Pseudomonas aeruginosa can be the skin, gastrointestinal tract, umbilical wound, urinary system, respiratory organs and conjunctiva of the eyes.
Pseudomonas aeruginosa infection does not have seasonality. The greatest susceptibility is observed in persons with immune disorders, as well as in the elderly and children.
Biological properties
Pyoverdine fluorescence
Production of the blue-green pigment pyocyanin (left) is the most important diagnostic feature.
Straight or curved rod with rounded ends, 1-5 × 0.5-1.0 µm, monotrich or lophotrich[6]. Chemoorganoheterotroph, obligate aerobe (denitrifier). Grows on MPA (the medium turns blue-green), MPB (there is cloudiness and film in the medium, also blue-green). Grows at 42 °C (optimum - 37 °C), selective medium - CPC-agar (nutrient agar with cetylperidinium chloride). Forms proteases. On solid nutrient media it dissociates into three forms - R-, S- and M-form [7]. Produces characteristic pigments: pyocyanin (phenazine pigment, colors the nutrient medium blue-green, extracted with chloroform), pyoverdine (yellow-green pigment that fluoresces in ultraviolet rays) and pyorubin (brown). Some strains carry out the biodestruction of hydrocarbons and formaldehyde[8].
Pseudomonas aeruginosa and nosocomial infection
So-called hospital-acquired or nosocomial infections are recorded all over the world. Most often they develop in intensive care units, burns, general surgery, and cardiac surgery departments.
The emergence of hospital infections is associated not only with poor organization of the sanitary and anti-epidemic regime in the hospital, but also with the constant increase in the resistance of pathogens to antibiotics and disinfectants. Nosocomial infections can occur as isolated cases or as outbreaks.
Up to 50% of hospital-acquired infections are caused by Pseudomonas aeruginosa. This microorganism is often isolated from door handles, hand brushes, water taps, soap, baby scales, changing tables, anesthesia machines, and from the hands of medical staff. But bacteria from the internal foci of the patient himself can also become active when the body’s resistance decreases and immune disorders occur.
There are risk factors
development of nosocomial Pseudomonas aeruginosa infection. These include:
Editor
Update date: 07/28/2018, next update date: 07/28/2021
If you find an error, please select a piece of text and press Ctrl+Enter.
Pseudomonas aeruginosa found in urine means that an infectious pathogen has entered the urinary tract. The symptoms of infection depend on the location, since the bacterium can affect not only the genitourinary system, but also the respiratory tract, bones and joints, skin, ears, digestive tract and other tissues or organs. A feature of Pseudomonas aeruginosa infection is that it is difficult to respond to standard antibacterial therapy.