If left untreated, obstruction can lead to kidney dysfunction.
What kind of pathology is this?
Ureteral problems are less common in men, but a serious risk factor is prostate disease, which affects 65% of men.
Ureteral obstruction is a partial or complete cessation of urine flow between the kidney and bladder. The cause of the obstruction is abnormal narrowing of the pathways and blockage caused by inflammatory or mechanical damage. The work of the genitourinary system is to promptly remove fluid and metabolic products from the body.
When the genitourinary system is healthy, after the formation of urine in the paired organs (kidneys), it is freely discharged through 2 connecting tubes (ureters) into the bladder, and then out through the urinary tube (urethra). The flow of urine is disrupted due to obstruction, which can happen in any part of the ureter. The disease responds well to treatment, but if the disease is left unattended, the symptoms quickly increase and lead to serious complications: hydronephrosis, hydrouronephrosis, kidney dysfunction.
The types of anomalies determine the causes of occurrence
Blockage of the ureter can be unilateral, less often bilateral. There are 2 main groups of obstruction:
One of the acquired causes of pathology may be cancer.
Both groups of obstruction can occur against the background of a genetic predisposition to cancer, the formation of cysts or stones.
Complications
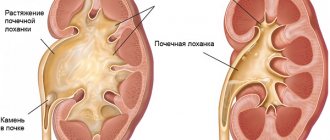
Blockage of the ureter by a stone causes a change in the flow of urine. Initially, moderate expansion of the renal pelvis and calyces (pyelectasia, hydrocalycosis), progressing, leads to degeneration of the renal tissue (hydronephrosis).
If inflammation begins (pyelonephritis, cystitis), the disease can be complicated by pyonephrosis and sepsis.
With long-term pathology, strictures, bedsores, and damage to the ureteral wall are likely to occur.
Acute renal failure may occur.
How to suspect and confirm the diagnosis?
Symptoms of ureteral obstruction
One of the first symptoms of pathology may be a rise in blood pressure.
In the early stages, the clinical picture does not appear or produces minor symptoms. Doctors identify such manifestations as:
As the disease progresses, symptoms intensify. The clinical picture is complemented by manifestations of the primary cause of ureteral obstruction; they depend on the etiology of the disease itself. In advanced or acute phases, manifestations such as:
Diagnostic procedures
Obstruction is often diagnosed based on ultrasound results. Such an examination allows you to identify defects in the early stages. Diagnosis is carried out during pregnancy. Thus, an early diagnosis of the fetus allows timely treatment to begin after birth. The list of examinations for both primary and secondary development of the anomaly involves the following list of diagnostic methods:
Cystoureteroscopy is one of the studies that a patient needs to undergo to make a diagnosis.
Return to contents
Bladder bladder obstruction
Urine is not released constantly. In a hollow muscular organ - the bladder, a certain volume of it accumulates and is then excreted. On average it is 300 ml, although the urea is able to hold up to 700 ml of liquid.
The flow of urine is regulated by the circular muscles - sphincters, and the detrusor muscle of the bladder. The accumulated fluid puts pressure on the walls of the organ. They stretch, and receptors in the muscle layer transmit a signal to the brain. As a result, the urge to urinate appears.
Normal urine output is ensured by the coordinated work of the urinary tract and sphincters. When emptying, the sphincter relaxes and stops blocking the canal. The bladder muscles, on the contrary, contract and form the flow of urine. Other muscles are also involved in the process, but their role is not so significant.
Violation of this mechanism is possible for a variety of reasons and in different ways. Thus, bladder outlet obstruction involves some obstruction to the outflow of fluid at the level of the cervix or urethra.
The cause may include birth anomalies, hypertrophy, and other factors. All of them lead to disruption of normal urine output, or even to complete delay.
In most cases, the cause of obstruction is anomalies in the development of the organ. Therefore, this disease is much more often observed in children, sometimes from birth. Boys get it much more often, since girls, due to their anatomical structure, have fewer reasons for the formation of infravesical obstruction. In men and women, the pathology is extremely rare.
Difficulties with urine output lead to distension of the bladder, atony and. In addition, unremoved urine residues are an excellent breeding ground for bacteria, which provokes the development of many infectious diseases.
Stones in the kidneys
Kidney stones are a sign of kidney stones or nephrolithiasis. Practical urology quite often encounters kidney stones, and kidney stones can form in both children and adults. Among patients with nephrolithiasis, men predominate; stones are more often detected in the right kidney; in 15% of cases, bilateral localization of stones occurs.
For urolithiasis. In addition to the kidneys, stones can be detected in the bladder (cystolithiasis), ureters (ureterolithiasis) or urethra (urethrolithiasis). Almost always, stones initially form in the kidneys and from there descend into the lower parts of the urinary tract. There are single and multiple stones; small kidney stones (up to 3 mm) and large ones (up to 15 cm).
Locations of the disease
Acquired pathology can affect some organs of the genitourinary system. Let's look at the main ones.
Ureter
This is the most common type of disease, which provokes an increase in pressure in the pyelocaliceal segment. As a result of such obstruction, renal failure and hydronephrosis may develop. Congenital pathology of ureteral obstruction can be determined by:
- by stenosis of segments in the ureter;
- along the retrocaval ureter;
- ureterocele.
Acquired obstruction can be caused by:
- tumor of the ureter or organs located next to it;
- an inflammatory disease that causes swelling and thickening of the walls;
- movement of stones from the renal pelvis to the ureter;
- deposits of urate crystals;
- uterine pressure during pregnancy;
- pressure from a uterine tumor;
- aortic aneurysm;
- unintentional ligation of the ureter during surgery on the pelvic organs, as well as a number of other cases.
Bladder neck
With obstruction of this organ, the outflow of urine from the bladder worsens, and there is also an increase in pressure on the kidneys. Pathology occurs as a result of the following congenital anomalies:
- ureterocele;
- obstruction in the bladder neck.
Pathology of obstruction of the bladder neck can be detected when a patient has:
- prostate adenoma;
- benign or malignant tumor affecting the bladder or neighboring organs;
- stones in the bladder.
Urethra
Pathology in this organ may be congenital. In this case, the following defects are identified:
- blocking the back and front of the urethra with valves;
- urethral stricture;
- stenosis.
The development of urinary tract obstruction may be associated with the following diseases:
- strictures formed as a result of the inflammatory process in the urethra;
- the entry of kidney stones and bladder stones into urine;
- consequences of traumatic events;
- urethral tumor;
- acquired phimosis.
The process of stone formation and types of stones
The formation of kidney stones occurs as a result of a complex physicochemical process due to disturbances in colloid balance and changes in the renal parenchyma.
Under certain conditions, a so-called elementary cell is formed from a group of molecules - a micelle, which serves as the initial core of the future calculus. The “building” material for the nucleus can be amorphous sediments, fibrin threads, bacteria, cellular detritus, and foreign bodies present in the urine. The further development of the stone formation process depends on the concentration and ratio of salts in the urine, urine pH, and the qualitative and quantitative composition of urinary colloids.
Most often, stone formation begins in the renal papillae. Initially, microliths form inside the collecting ducts, most of which are not retained in the kidneys and are freely washed out in the urine. When the chemical properties of urine change (high concentration, pH shift, etc.), crystallization processes occur, leading to retention of microliths in the tubules and encrustation of the papillae. In the future, the stone may continue to “grow” in the kidney or descend into the urinary tract.
Based on their chemical composition, there are several types of stones found in the kidneys: oxalate, phosphate, urate, carbonate, cystine, protein, cholesterol, xanthine. Oxalates consist of calcium salts of oxalic acid. They have a dense structure, black-gray color, and a spiky, uneven surface. Oxalate kidney stones can form due to both acidic and alkaline urine.
Phosphates are stones consisting of calcium salts of phosphoric acid. Their consistency is soft, crumbly, with a smooth or slightly rough surface, and a whitish-grayish color. Phosphate kidney stones are formed in alkaline urine and grow quite quickly, especially in the presence of infection (pyelonephritis).
Urates are represented by crystals of uric acid salts. Their structure is dense, color ranges from light yellow to brick-red, surface is smooth or finely pinpointed. Urate stones in the kidneys occur when urine is acidic. Carbonate stones are formed by the precipitation of calcium salts of carbonic acid. They are soft, light, smooth, and can have different shapes.
Cystine stones contain sulfur compounds of the amino acid cystine. The stones have a soft consistency, a smooth surface, a round shape, and a yellowish-white color. Protein stones are formed mainly by fibrin with an admixture of bacteria and salts. These kidney stones are soft, flat, small in size, and white in color. Cholesterol kidney stones are rare; formed from cholesterol, have a soft crumbly consistency, black color.
Sometimes kidney stones form not of a homogeneous, but of a mixed composition. One of the most difficult types of kidney stones are coral kidney stones, which account for 3-5% of all stones. Coral-shaped kidney stones grow in the pelvis and in appearance represent its cast, almost completely repeating the size and shape.
Causes of kidney stones
Stone formation is based on the processes of crystallization of urine saturated with various salts and the deposition of crystals onto the protein matrix-core. Kidney stones can develop in the presence of a number of concomitant factors.
Disorders of mineral metabolism leading to the formation of kidney stones may be genetically determined. Therefore, people with a family history of nephrolithiasis are recommended to pay attention to the prevention of stone formation and early detection of stones by monitoring a general urine test. undergoing an ultrasound of the kidneys and an ultrasound of the bladder. observations from a urologist.
Acquired disorders of salt metabolism, leading to the formation of kidney stones, can be caused by external (exogenous) and internal (endogenous) reasons.
Among external factors, the greatest importance is given to climatic conditions and drinking regime and diet. It is known that in hot climates with increased sweating and a certain degree of dehydration, the concentration of salts in the urine increases, which leads to the formation of kidney stones. Dehydration can be caused by poisoning or an infectious disease that occurs with vomiting and diarrhea.
In the northern regions, stone formation factors may include a deficiency of vitamins A and D, a lack of ultraviolet radiation, and a predominance of fish and meat in the diet. Consumption of drinking water with a high content of lime salts, food addiction to spicy, sour, salty foods also leads to alkalization or acidification of urine and precipitation of salts.
Among the internal factors that contribute to the formation of kidney stones, the first to be distinguished are hyperfunction of the parathyroid glands - hyperparathyroidism. Increased work of the parathyroid glands increases the phosphate content in the urine and the leaching of calcium from bone tissue. At the same time, the concentration of calcium phosphate salts in the urine increases significantly. Similar disorders of mineral metabolism can occur with osteoporosis. osteomyelitis. bone fractures, spinal injuries, spinal cord injuries. accompanied by prolonged immobility of the patient, loss of bone tissue, and disruption of the dynamics of urinary tract emptying.
Endogenous factors for the formation of kidney stones also include gastrointestinal diseases - gastritis. peptic ulcer. colitis. leading to disruption of the acid-base balance, increased excretion of calcium salts, weakening of the barrier functions of the liver and changes in the composition of urine.
In the pathogenesis of the formation of kidney stones, a known role belongs to unfavorable local conditions in the urinary tract - infections (pyelonephritis, nephrotuberculosis, cystitis, urethritis), prostatitis. kidney abnormalities. hydronephrosis. prostate adenoma. diverticulitis and other pathological processes that disrupt the passage of urine.
Slowing the outflow of urine from the kidney causes stagnation in the pyelocaliceal system, oversaturation of urine with various salts and their precipitation, and delayed passage of sand and microliths into the urine. In turn, the infectious process developing against the background of urostasis leads to the entry of inflammatory substrates into the urine - bacteria, mucus, pus, protein. These substances participate in the formation of the primary core of the future calculus, around which salts, which are present in excess in the urine, crystallize.
Symptoms of kidney stones
Depending on their size, quantity and composition, kidney stones can cause symptoms of varying severity. A typical clinical picture of nephrolithiasis includes lower back pain and the development of renal colic. hematuria, pyuria, and sometimes spontaneous passage of kidney stones in the urine.
Pain in the lower back develops as a result of a violation of the outflow of urine, can be aching, dull, and with sudden urostasis, when a stone blocks the renal pelvis or ureter, progress to renal colic. Coral kidney stones are usually accompanied by a mild dull pain, while small and dense ones give a sharp, paroxysmal pain.
A typical attack of renal colic is accompanied by sudden sharp pain in the lumbar region, spreading along the ureter to the perineum and genitals. Reflexively, against the background of renal colic, frequent painful urination, nausea and vomiting, and flatulence occur. The patient is agitated, restless, and cannot find a position that alleviates the condition. The pain attack in renal colic is so severe that it is often stopped only by the administration of narcotic drugs. Sometimes with renal colic, oliguria and anuria and fever develop.
At the end of an attack of renal colic, sand and kidney stones often pass out in the urine. When passed, stones can injure the urinary tract mucosa, causing hematuria. More often, damage to the mucosa is caused by pointed oxalate stones. With kidney stones, the intensity of hematuria can vary - from slight erythrocyturia to severe gross hematuria. Discharge of pus in the urine (pyuria) develops in the presence of inflammation in the kidneys and urinary tract.
The presence of kidney stones does not manifest itself symptomatically in 13-15% of patients. In this case, as a rule, pyelonephritis and morphological changes in the kidneys are absent.
Forecasts
For an acute form of pathology, with timely treatment, the outcome can be favorable.
Chronic inflammation can lead to metaplasia and hyperplasia, which are pre-cancerous conditions. Chronic inflammation can lead to metaplasia and hyperplasia, which are pre-cancerous conditions. Chronic inflammation can lead to metaplasia and hyperplasia, which are pre-cancerous conditions.
Many types of obstruction can be corrected, but delay in seeking medical help can lead to irreversible kidney damage.
Urinary tract obstruction is a pathological condition in which the outflow of urine is impaired. Obstruction can occur at any level of the urinary system, from the kidneys to the urethra. According to statistics, the pathology is more often diagnosed in people over 50 years of age.
Diagnosis of kidney stones
Recognition of kidney stones is made on the basis of anamnesis, a typical picture of renal colic, laboratory and instrumental imaging studies.
At the height of renal colic, sharp pain on the side of the affected kidney, a positive Pasternatsky sign, and painful palpation of the corresponding kidney and ureter are determined. Urine examination after an attack reveals the presence of fresh red blood cells, leukocytes, protein, salts, and bacteria. Biochemical examination of urine and blood to a certain extent allows us to judge the composition and causes of the formation of kidney stones.
Right-sided renal colic must be differentiated from appendicitis. acute cholecystitis. therefore, an abdominal ultrasound may be required. Using kidney ultrasound, anatomical changes in the organ, the presence, location and movement of stones are assessed.
The leading method for detecting kidney stones is x-ray diagnostics. Most of the stones are identified already during survey urography. However, protein and uric acid (urate) kidney stones do not block rays and do not produce shadows on urograms. They can be identified using excretory urography and pyelography. In addition, excretory urography provides information about morpho-functional changes in the kidneys and urinary tract, the localization of stones (pelvis, calyx, ureter), shape and size of kidney stones. If necessary, urological examination is supplemented with radioisotope nephroscintigraphy. MRI or CT scan of the kidneys.
Methods for studying obstructive uropathy
The use of imaging modalities, their choice and sequence depend on the suspected cause and location of the changes, as well as the results of previous studies.
Ultrasonography of the abdominal cavity and retroperitoneal space is the primary method of examination in most patients, with the exception of those suffering from urethral diseases, since it allows one to avoid potential allergic and toxic complications of intravenous administration of X-ray contrast agents and to evaluate changes in the kidneys. If the most minimal diagnostic criteria are taken into account, the false-positive rate is 25%. A combination of ultrasonography, plain radiography of the abdominal organs and, if necessary, computed tomography makes it possible to diagnose obstructive uropathy in more than 90%, however, ultrasonography and computed tomography without contrast are often unable to differentiate hydronephrosis from multiple renal or parapelvic cysts.
Duplex Doppler ultrasonography helps in the diagnosis of unilateral obstructive uropathy by determining an increased resistance index, reflecting increased renal vascular resistance in the affected kidney. Sometimes these changes can be detected at the very beginning of acute obstruction before the maximum expansion of the pyelocaliceal system occurs. An increase in vascular resistance develops as a result of activation of the renin-angiotensin system and increased synthesis of thromboxane A2 and endothelin. This test is difficult in obesity, and in cases of bilateral obstruction, findings are difficult to distinguish from changes in primary bilateral renal disease.
Excretory urography began to be used much less frequently with the introduction into practice of X-ray computed tomography and magnetic resonance imaging without and with contrast. However, difficulties in determining the level of obstruction, especially when the urinary tract is blocked by a stone, necrotic renal papilla or blood clot, are an indication for excretory urography, and if it is ineffective, for retrograde ureteropyelography.
Radioisotope study of the kidneys. If the kidney, under conditions of obstruction, does not secrete a radiopaque substance, it can help assess the safety of the functioning parenchyma, but is not able to clarify the level of blockage of the upper urinary tract. It is mainly used in the form of “diuretic renography” to assess the degree of urinary passage disturbance in the absence of clearly visible obstruction.
Antegrade and retrograde pyelography are more often performed in patients with azotemia. An antegrade examination is performed after percutaneous puncture nephrostomy, a retrograde examination is performed after cystoscopy with catheterization of the corresponding ureter. Underexamination for intermittent obstruction significantly reduces the diagnostic value of these methods.
Diuretic renography is most often performed in the presence of pain with slight dilatation of the upper urinary tract. Immediately before the radioisotope study of the kidneys, a loop diuretic is prescribed. If significant obstruction occurs, the passage of the radiopharmaceutical is slowed, despite an increase in the rate of urine production. Similar changes can be recorded in the form of delay of radiopaque contrast agent during excretory urography. The greatest differential diagnostic difficulties arise if the renogram curves do not change or change symmetrically for both kidneys. The patient's persistent complaints of pain require a study of perfusion pressure in the collecting system. After percutaneous puncture and catheterization of the pelvis, it is perfused with physiological solution at a rate of 10 ml/min. In the presence of obstruction, with a significant increase in the volume of transported fluid as perfusion occurs, an increase in pressure in the pelvis of more than 22 mm Hg is observed. Diuretic radionuclide testing , urography, and a positive perfusion test producing similar pain confirm obstruction. The absence of an increase in perfusion pressure indicates an extrarenal origin of pain. However, false positive and false negative results are possible.
Treatment of kidney stones
Treatment of nephrolithiasis can be conservative or surgical and in all cases is aimed at removing kidney stones. elimination of infection and prevention of re-formation of stones.
For small kidney stones (up to 3 mm), which can be passed independently, plenty of water load and a diet excluding meat and offal are prescribed. For urate stones, a dairy-vegetable diet that alkalizes urine and alkaline mineral waters (Borjomi, Essentuki) is recommended; for phosphate stones - take acidic mineral waters (Kislovodsk, Zheleznovodsk, Truskavets), etc. Additionally, under the supervision of a nephrologist, medications that dissolve kidney stones, diuretics, antibiotics, nitrofurans, antispasmodics can be used.
With the development of renal colic, therapeutic measures are aimed at relieving obstruction and pain. For this purpose, injections of platyphylline, metamizole sodium, morphine or combined analgesics in combination with atropine solution are used; A warm sitz bath is performed and a heating pad is applied to the lumbar region. In case of intractable renal colic, novocaine blockade of the spermatic cord (in men) or the round ligament of the uterus (in women), catheterization of the ureter or dissection of the ureteral orifice (in case of strangulation of a calculus) is required.
Surgical removal of kidney stones is indicated for frequent renal colic, secondary pyelonephritis, large stones, and ureteral strictures. hydronephrosis, kidney blockade, threatening hematuria, solitary kidney stones, coral stones.
In practice, for nephrolithiasis, a non-invasive method is often used - extracorporeal lithotripsy. allowing you to avoid any interference in the body and remove fragments of stones from the kidneys through the urinary tract. In some cases, an alternative to open surgery is a high-tech procedure - percutaneous (percutaneous) nephrolithotripsy with lithoextraction.
Open or laparoscopic interventions to remove kidney stones - pyelolithotomy (dissection of the pelvis) and nephrolithotomy (dissection of the parenchyma) are resorted to in case of ineffectiveness of minimally invasive surgery. In case of complicated kidney stone disease and loss of kidney function, nephrectomy is indicated.
A set of therapeutic measures for blockage of the ureter
In therapy, medication and radical methods are used. Treatment depends on the characteristics of the disease, severity and spread. Both methods are aimed mainly at restoring normal function of the genitourinary system and kidney function. After which other symptoms disappear. In cases of particularly severe diseases such as cancer, treatment is aimed at eliminating the primary disease.
Return to contents
Drug treatment
Medicines are needed to eliminate internal causes that cause ureteral obstruction in men and women, usually inflammation, infections, and parasitic infestations. In drug therapy, drugs are used depending on the primary cause of the obstruction. Anti-inflammatory, anti-infective or anti-parasitic drugs are prescribed. They also prescribe immunomodulatory medications and a strict diet. Alpha blockers are required for discomfort after stent placement.
Return to contents
Surgery
The type of operation depends on the characteristics of the pathology. The main ones are shown in the table:
| Technique | Types of operations | Short description |
| Restoring urine flow | Installation of a ureteral stent | The stent has the form of a hollow tube, serves to expand the ureter |
| Urinary catheterization | Insertion of a catheter to eliminate excess urine from the kidney through a puncture hole and under ultrasound control | |
| Percutaneous nephrostomy | Insertion of a hollow tube through the urethra to drain urine in cases of initial bladder injury | |
| Minimally invasive surgery | Endoscopic surgery | The endoscope is inserted through the urethra, with its help an incision is made and a stent is installed for the outflow of urine, used for diagnostic purposes |
| Surgical correction | Pyeloplasty | Removal of the damaged part of the ureter followed by installation of a wall to expand the lumen of the ureter and removal after 6 weeks |
| Transureteroureterostomy | Connecting a damaged ureter with a healthy one to normalize the outflow of urine | |
| Ureteral reimplantation | Cutting out the damaged area and then connecting healthy tissues together | |
| Ureterolysis | Elimination of external abnormal factors in the form of fibrous or scar tissue that affect the ureter | |
| Partial nephrectomy | Partial removal of the kidney affected by obstruction | |
| Ureterectomy | Partial or complete removal of the lesion with reconstruction by tightening the ureter or lowering the kidney to connect to the ureter |
Return to contents
Prediction and prevention of kidney stones
In most cases, the course of nephrolithiasis is prognostically favorable. After removal of kidney stones, subject to the instructions of the urologist, the disease may not recur. In unfavorable cases, calculous pyelonephritis and symptomatic hypertension may develop. chronic renal failure. hydropyonephrosis.
For any type of kidney stones, it is recommended to increase the drinking volume to 2 liters per day; use of special herbal preparations; exclusion of spicy, smoked and fatty foods, alcohol; avoiding hypothermia; improving urodynamics through moderate physical activity and exercise. Prevention of complications of nephrolithiasis comes down to early removal of kidney stones and mandatory treatment of concomitant infections.
Kidney stones video
Urolithiasis is a disease of the kidneys and urinary tract, characterized by the formation of stones (calculi) in the kidneys and urinary tract stones. Therefore, this disease is called nothing more than kidney stones.
Urolithiasis or nephrolithiasis is the medical term used to describe stones that form in the urinary tract.
The urinary tract, or system, consists of the kidneys, ureters, bladder and urethra. The kidneys are two bean-shaped organs located below the ribs in the middle of the back, one on each side of the spine. The kidneys remove excess water and waste from the blood by producing urine. They also maintain a stable balance of salts and other substances in the blood. The kidneys produce hormones that help build strong bones and the formation of red blood cells.
Doctors also use terms that describe the location of stones in the urinary tract. For example, when stones are found in the ureter, the term ureterolithiasis is used, the presence of stones anywhere in the urinary tract is called urolithiasis, stones directly in the renal pelvis are called nephrolithiasis.
Kidney stones are one of the most painful urological disorders that have plagued people for centuries. Scientists have found evidence of this by finding kidney stones in a 7,000-year-old Egyptian mummy. Unfortunately, kidney stones are one of the most common urinary tract diseases.
Kidney stones are a hard mass made up of tiny crystals. However, there may be one or more stones in the kidneys or ureter, they form when the urine becomes too concentrated and substances in the urine crystallize to form stones. Symptoms occur when stones begin to move down the ureter, causing severe pain.
Causes and risk factors of kidney stones
- Dehydration. Dehydration from reduced fluid intake or exercise without adequate fluid replacement increases the risk of kidney stones. An obstruction to the flow of urine can also lead to the formation of stones. In this regard, climate may be a risk factor for the development of kidney stones, as residents of hot and dry areas are more likely to experience dehydration and are susceptible to the formation of kidney stones.
- Chronic urinary infection. Kidney stones can also result from infections in the urinary tract, such as pyelonephritis and cystitis.
- Metabolic disease. Metabolic disorders, including inherited metabolic disorders, can change the composition of urine and increase a person's risk of stone formation.
— Disturbance of calcium metabolism in the body - hypercalciuria. Another inherited disorder characterized by high calcium levels in the urine causes stones in more than half of cases. In this condition, too much calcium is absorbed from food and excreted in the urine, where it can form calcium phosphate or calcium oxalate stones.
- Gout. Gout causes a chronic increase in the amount of uric acid in the blood and urine, which can lead to the formation of uric acid stones.
— Abnormalities of kidney development and kidney disease. People suffering from hyperparathyroidism, renal tubular acidosis, cystinuria and hyperoxaluria, narrowing of the ureter, abnormal kidney development, and polycystic kidney disease have an increased risk of developing kidney stones.
— Diabetes and hypertension. Chronic diseases such as diabetes and high blood pressure are also associated with an increased risk of developing kidney stones.
— Diseases of the digestive tract. People with inflammatory bowel disease are also more likely to develop kidney stones due to impaired calcium metabolism and increased concentrations of stone-forming substances in the blood. People who have had an intestinal bypass or ostomy are also at increased risk of developing kidney stones.
- Taking medications. Some drugs also increase the risk of kidney stones. These drugs include some diuretics, calcium-containing antacids, and the protease inhibitor Indinavir, a drug used to treat HIV infection.
- Nutrition. Dietary factors may increase the risk of stone formation in susceptible individuals, including high intake of animal protein, high salt content, excessive sugar intake, excess vitamin D, and possibly excessive intake of oxalate-containing foods such as spinach.
— Physical inactivity. A sedentary lifestyle and mainly sedentary work leads to disruption of phosphorus-calcium metabolism and congestion in the pelvis, which in turn causes the formation of stones in the urinary system.
Types of kidney stones
Kidney stones form when urine contains too much of certain substances. These substances can create small crystals that become stones. The stone may take several weeks or months to form. There are different types of kidney stones:
— Calcium stones (vedellite, wewellite, apatite, brushite, whitlockite). Calcium kidney stones are the most common. They are more common in men aged 20–30 years. Calcium usually combines with other substances such as oxalates, phosphates or carbonates to form stones. Oxalates are present in some foods such as spinach. They are also found in vitamin C supplements. Small intestinal diseases increase the risk of developing these stones. Interestingly, low levels of calcium in the diet can alter the calcium oxalate balance and lead to increased oxalate excretion and a tendency to form oxalate stones.
- Cystine or protein stones. Cystine is a substance that is a constituent of muscles, nerves and other parts of the body. Cystine stones can form in people prone to cystinuria. This disease is inherited and affects men and women equally.
— Magnesium stones (newberite, struvite). Struvite mainly occurs in women who have urinary tract infections. These stones can be very large and can block the kidneys, ureters or bladder.
- Uric acid stones (sodium urate, ammonium urate). Urates are more common in men than in women. They can occur with gout or chemotherapy.
— Mixed stones. Other substances, including medications such as acyclovir, indinavir, and triamterene, can also form stones.
Symptoms of kidney stones (urolithiasis)
Kidney stones usually have no symptoms until the stones begin to move down the ureters into the bladder. When this happens, the stones can block the flow of urine from the kidney.
The main symptom is severe pain that begins suddenly and can stop just as abruptly. This pain has been described by many as the worst pain of their lives, even worse than the pain of childbirth or broken bones.
The main symptoms of urolithiasis usually include:
- Pain in the abdomen or lower back, called renal colic. It can be so severe that it is often accompanied by nausea and vomiting and can radiate to the groin, thigh or testicle.
Congenital pathology
Pathology is diagnosed for the following defects:
- Double ureter . This is the most common form, in which 2 ureters arise from one kidney. Normal functioning of both ureters is extremely rare; underdevelopment of one of them almost always occurs. During normal functioning of both organs, fluid returns to the ureter, injuring the kidney.
- Obstruction in the ureteropelvic region . In this case, the ureter of the renal pelvis becomes the site of fluid accumulation. This pathology is characterized by stagnation of urine, which provokes enlargement and expansion of the kidney. This defect can be congenital or diagnosed in children. Treatment must be timely, otherwise the disease will lead to organ dysfunction.
- Blockage of the vesicoureteral part . Fluid accumulates in the area where the ureter connects to the bladder. This pathology is characterized by the development of inflammation during the release of urine into the kidneys.
- Ureterocele . The resulting hernia or cyst produces a squeezing effect on the walls of the organ, which causes a narrowing of the lumen of the ureter. The location of this pathology is often the area next to the bladder, and, as a result, urine is thrown back into the kidney.
Kidney stones: symptoms, treatment
The most pressing problem of modern urology is the problem of treating urolithiasis. Today, this pathology remains one of the causes of renal failure (about 7% of patients requiring hemodialysis are patients with urolithiasis). The annual incidence rate of nephrolithiasis increases every year and leads to the development of various complications, and the results of treatment are not always satisfactory in their effectiveness.
Urolithiasis, in clinical terminology called nephrolithiasis, is a polyetiological metabolic disease manifested by the formation of calculi (stones) in the kidneys. This pathology, characterized by a tendency to relapse and severe persistent course, is often hereditary in nature.
Today there are many theories that explain the causes of stone formation, but none of them can be considered completely correct and well-established. According to experts, there are endogenous and exogenous factors that provoke the development of nephrolithiasis.
Endogenous factors
Exogenous factors
Classification of kidney stones
Mineralogical classification
It should be noted that isolated forms of nephrolithiasis are quite rare. More often, stones have a mixed (polymineral) composition.
If the origin of kidney stones is related to dietary habits and the composition of drinking water, primary nephrolithiasis is diagnosed. This disease is caused by persistent acidification of urine, excessive intestinal absorption of metabolites and decreased renal reabsorption.
In pathologies accompanied by metabolic disorders (hyperkalemia, hypercalcemia, hyperuricemia), we are talking about secondary nephrolithiasis.
Localization, size and shape
Stones can be localized in one or both kidneys (in the renal pelvis, as well as in the lower, middle or upper calyx). They are single and multiple. The size of the stones, indicated in millimeters (20), can range from the head of a pin to the size of the renal cavity (staghorn stones can form an impression of the collecting system). The shape of kidney stones can be round, flat or angular.
Mechanism of formation of kidney stones
The mechanism of the initiation and development of nephrolithiasis depends on various factors (urine pH, type of diathesis, excretion of one or another type of salt, etc.). According to experts, the primary formation of stones occurs in the renal pelvis and collecting ducts. First, a core forms, and then crystals begin to form around it.
There are several theories of stone formation (crystallization, colloid and bacterial). Some authors note that the main role in the process of nucleation is played by atypical gram-negative bacteria capable of producing apatite (calcium carbonate). These microorganisms are detected in 97% of all kidney stones.
Most often, nephrolithiasis is diagnosed in males. At the same time, women are characterized by more severe forms of pathology (for example, coral stones, which occupy almost the entire cavity system of the excretory organ).
Due to the fact that kidney stones are a polyetiological disease, before developing treatment tactics, it is necessary to try to find out the cause of the development of the pathological process.