Definition and types of acute pyelonephritis
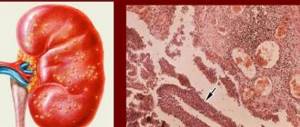
Acute pyelonephritis is an inflammatory process that affects the pyelocaliceal system of the kidneys. This disease is one of the most common in urology and is characterized by pronounced clinical symptoms. Unlike glomerulonephritis, pyelonephritis does not affect the glomerular system of the kidneys. The disease can affect one or both organs.
In clinical practice, it is customary to distinguish between primary, or non-obstructive, and secondary, or obstructive, types of pathology. Obstructive pyelonephritis develops when there is obstruction (narrowing of the lumen) of the ureters due to compression from the outside or blockage from the inside by a stone, tumor, etc.
Pyelonephritis is an inflammatory process in the renal pelvis
According to the nature of the inflammatory process, acute pyelonephritis is divided into purulent and non-purulent (serous).
Purulent pyelonephritis, in turn, can be divided into several types:
- carbuncle - a limited purulent-necrotic process in the tissues of the kidney;
- abscess - limited inflammation of the kidney tissue with the formation of a purulent cavity. It differs from a carbuncle in the larger size of the lesion;
- apostematous pyelonephritis - the formation of multiple foci of purulent lesions of the renal tissue.
Pyelonephritis: video
Causes of pyelonephritis
Acute pyelonephritis is a kidney disease that is inflammatory in nature and affects the parenchyma, pelvis and calyx of the organ. Acute pyelonephritis is a kidney disease that is inflammatory in nature and affects the parenchyma, pelvis and calyx of the organ. Most often, women and children suffer from this disease. The main signs of the formation of acute pyelonephritis are:
- streptococcus;
- coli;
- staphylococcus;
- Pseudomonas aeruginosa;
- Proteus.
Acute kidney inflammation is quite complex with pronounced symptoms. There are a number of favorable factors that allow harmful bacteria to enter the organ and infect it. There are three main ways that microbes travel to the kidneys:
- through the bloodstream, provided that there is a source of infection in the body, for example, tonsillitis, caries or other infectious diseases;
- through the lymph flow, subject to the presence of infectious diseases in the body;
- through the ureter, subject to the presence of an inflammatory process in the bladder, for example, urethritis or cystitis.
For information! The inflammatory process in the kidneys develops solely due to the entry of harmful bacteria into the organ; independent development of pathology is excluded.
Causes and predisposing factors
The most common cause of the disease is microorganisms that colonize the large intestine. In 90% of cases, the pathology is provoked by Escherichia coli.
Not all strains of E. coli have virulence factors. Of the numerous strains of Escherichia coli (over 150), only some are uropathogenic.
I.V. Mikhin
https://www.volgmed.ru/uploads/files/2014–8/36300-posobie_umo_dlya_studentov_pielonefrit.pdf
Other causative agents of pyelonephritis include:
- klebsiella;
- enterobacteria;
- protea;
- staphylococcus.
The disease can be caused by mixed infections. This is especially true for pathologies acquired during hospital treatment (hospital or nosocomial infections).
It should be noted that sexually transmitted infections (chlamydia, ureaplasma, gonococci, trichomonas) do not cause kidney disease, although they are accompanied by frequent urination.
The development of a secondary process is caused by a violation of the outflow of urine against the background of external compression, narrowing of the lumen or blockage of the ureters.
Predisposing factors for the development of pathology include:
- congenital obstruction (narrowing of the lumen) of the ureters;
- frequent and prolonged hypothermia;
- hypovitaminosis;
- frequent respiratory tract infections;
- endocrine disorders;
- pregnancy;
- decreased immune defense of the body;
- disorders of the nervous regulation of the bladder and ureters.
Urinary tract infections
The organs of the urinary system include:
- kidneys - a paired organ responsible for filtering blood and producing urine;
- ureters - hollow tubes through which urine flows into the bladder;
- the bladder is a hollow organ, a smooth muscle reservoir in which urine accumulates;
- The urethra (or urethra) is a tubular organ that removes urine from the body.
Despite the fact that the urinary tract is normally sterile, any organ can be susceptible to the development of an infectious process. A special feature is that in most cases, inflammation is transmitted between organs along the ascending (from the urethra up to the kidneys) or descending pathway (from infected kidneys to the bladder).
How does the disease manifest itself?
Symptoms of the disease include signs of general intoxication and local manifestations. Each type of pathology has its own clinical picture.
Compared to serous pyelonephritis, purulent forms are characterized by more pronounced manifestations and an acute course. Primary pyelonephritis is characterized by a picture of general intoxication, while in secondary pyelonephritis local symptoms come to the fore.
Primary acute pyelonephritis can develop very quickly. The patient complains of severe weakness and malaise. His body temperature rises, severe chills and profuse sweating appear. There are all the signs of general intoxication:
- headache;
- pain in muscles and joints;
- rapid heartbeat;
- nausea and vomiting.
Digestive disorders such as diarrhea, constipation, and bloating are possible.
Local symptoms of the disease manifest themselves as pain in the lumbar region. Sometimes discomfort spreads to the abdomen and inner thigh. The pain can be dull and diffuse or sharp and intense. There are no urinary problems with this type of pathology.
Lower back pain may be a symptom of acute pyelonephritis
Secondary pyelonephritis most often debuts with renal colic. Acute lower back pain is accompanied by high fever with chills, vomiting, and headache. After some time, a critical decrease in temperature occurs, and health improves somewhat.
Carbuncle and kidney abscess are characterized by severe constant pain in the lower back and high fever with chills. Local manifestations include tension in the muscles of the lower back and abdominal wall.
The severity of clinical symptoms may depend on the gender, age and condition of the patient. In weakened or elderly people, the manifestations may not be so striking. Children are characterized by increased body temperature, frequent vomiting and diarrhea.
I had to observe the erased course of the disease in a three-year-old child. Clinical manifestations consisted of complaints of joint pain, general weakness and irritability. The diagnosis was established by a pediatrician based on examination (there was tension in the lumbar region when palpating), changes in urine analysis and an ultrasound picture characteristic of pyelonephritis. Indirect confirmation of the diagnosis was the good effect of treatment with Nitroxoline and Canephron.
In women, the acute process may be accompanied by discharge from the genital tract or delayed menstruation. Although these symptoms are not obligatory and do not have much diagnostic value, they are understandable given the characteristics of the development of the disease.
Providing emergency medical care for glomerulonephritis
Glomerulonephritis is an immunoinflammatory disease with primary and initial damage to the glomerular apparatus of the kidneys. Main clinical forms: acute, chronic, rapidly progressive glomerulonephritis. It occurs not only as an independent disease, but also as a syndrome that is a component of various systemic diseases (systemic lupus erythematosus, hemorrhagic vasculitis, infective endocarditis, periarteritis nodosa, systemic scleroderma).
Acute glomerulonephritis
Symptoms . Acute glomerulonephritis most often develops 6-20 days after streptococcal infection. In typical cases, the triad is characteristic: edema, hypertension, hematuria. Initially, weakness, headache, shortness of breath, thirst, and pain in the lumbar region appear. Appetite decreases, the amount of urine decreases (sometimes it turns red). There is pallor of the skin, swelling under the eyes, puffiness of the face, and sometimes anasarca. Blood pressure is increased, there is a tendency to bradycardia, the borders of the heart are often expanded. Often there are signs of congestion in the lungs. Various changes in the repolarization phase on the ECG are detected in 20-75% of patients. There is a latent form that occurs with minimal clinical manifestations.
Chronic glomerulonephritis
The following forms are distinguished: latent (proteinuria, microhematuria, slight increase in blood pressure), hematuric (constant hematuria with episodes of macrohematuria, aggravated after respiratory diseases), nephrotic (low diuresis, persistent edema, as chronic renal failure develops, the edematous syndrome decreases, giving way to hypertensive, in During the course of the disease, nephrotic crises may develop with the appearance of a peritonitis-like syndrome, fever, erysipelas, hypovolemic collapses, phlebothrombosis, and the addition of infectious complications are also common), hypertensive (in the first place comes arterial hypertension, complicated by episodes of left ventricular failure, less often by strokes and myocardial infarction), mixed (a combination of nephrotic syndrome and hypertension, characterized by a steadily progressive course).
Rapidly progressive glomerulonephritis
It begins as acute glomerulonephritis, often with lower back pain, gross hematuria, retinopathy with retinal detachment, and then rapidly increasing renal failure. Diagnosis . At the prehospital stage it is difficult, especially in cases of monosymptomatic or latent forms. Differential diagnosis is primarily carried out with other renal diseases, as well as with diseases for which it may be a mask. Complications : pulmonary edema, congestive heart failure; hypertensive crisis; acute renal failure (anuria, azotemia, hyperkalemia, uremic pulmonary edema); eclampsia (precursors: severe headache, sometimes nausea, dizziness, polyuria; further sudden loss of consciousness, the patient may bite his tongue, wheezing breathing, foam at the mouth, clonic and tonic convulsions, pupils do not respond to light, sharply increased tendon reflexes, heart rate 50 -6O per minute); hemorrhages in the brain; acute visual impairment (retinal edema, spasm); myocardial infarction
Emergency medical care
Eclampsia: take measures against tongue biting (rubber object or handkerchief between teeth). 20-30 ml of 40% glucose are administered intravenously, 20-25 ml intramuscularly, or 10-15 ml of 25% magnesium sulfate solution intravenously. To quickly reduce blood pressure, sodium nitroprusside is administered intravenously up to 10 mcg/kg per minute or labetalol 20-40 mg per minute, repeat every 15 minutes until the effect occurs or a dose of 300 mg is reached. Furosemide is administered 2 mg/kg IV - up to 300-1000 mg. Convulsive syndrome is relieved with sibazone (diazepam) - 10-30 mg IV slowly over 5-10 minutes. If there is no effect on the administration of drugs and anuria, bloodletting up to 400-500 ml. A normal hypertensive crisis can be stopped, in addition to these drugs, with dioxide up to 300 mg, or hydralazine 10-20 mg IV, repeat after 30 minutes (IM 10-50 mg), or phenipshine (nifedipine) up to 1 mg IV ( sublingually 10-20 mg). In case of chronic renal failure, do not reduce ADP when residual nitrogen levels exceed 100 mg%. You can give 50-5 g of xylitol or sorbide, which causes fluid loss of up to 3-5 l/day. With anuria, heat, no-spa or papaverine 2 ml of a 2% solution IM, or platiphylline 2 mg s.c. can sometimes help. For hypovopemic collapses - 100-150 ml of polyglucin or reololigpyukin intravenously. Pulmonary edema with diabetes >160 mm Hg. Art. treated intravenously with sodium nitroprusside up to 10 mcg/kg/min or pentamine up to 50 mg slowly diluted over 10-15 minutes. In case of renal failure, the doses of antiarrhythmic drugs and glycosides are reduced by 2 times. Hospitalization : to the nephrology department when acute nephritis is diagnosed or when complications arise due to chronic nephritis.
9.1. Acute glomerulonephritis
Acute glomeluronephritis (AGN) is a bilateral diffuse immune inflammation of the kidneys with predominant damage to the glomeruli and involvement of the interstitial tissue of the kidneys in the pathological process.
Pathophysiology
The origin of AGN clearly shows a connection with infection. The most common variants of post-infectious nephritis include AGN, in which nephritogenic strains of group A β-hemolytic streptococcus act as the etiological factor. The entrance gates of infection are most often the pharynx, tonsils, less often inflammation of the middle ear and paranasal sinuses, and skin infections. In some cases, AGN can develop after pneumonia, scarlet fever, meningitis, osteomyelitis, against the background of infective endocarditis or specific infections - typhoid fever, leptospirosis, brucellosis, diphtheria. Other possible etiological causes are viruses and parasitic infestations.
Vaccination, individual intolerance and hypersensitivity to drugs and chemicals, insect venom, and pollen are also some of the etiological factors of AGN.
In the pathogenesis of glomerulonephritis, leading importance is attached to damage to the glomeruli by immune complexes (IC) that arise during the interaction of an antigen (AG) with an antibody (AT). In response to exogenous Ags (infectious, medicinal, foreign proteins) entering the body, Abs appear, which bind to them and form circulating ICs (CICs) in the vascular bed. CECs are filtered by glomeruli, precipitated and fixed on the basement membrane of their capillaries, causing cellular reactions of immune inflammation.
IR activates the complement system, the activated fractions of which directly damage the capillary walls and increase the permeability of the glomerular filter. Macrophages, lymphocytes and leukocytes migrate to the area of glomerular damage, which produce numerous biologically active substances and activate coagulation factors and platelets. These reactions cause direct damage to the glomeruli.
Diagnosis and differential diagnosis
Diagnosis of the disease begins with a thorough questioning of the patient and collection of anamnesis. Data obtained during clinical examination are of great importance.
Upon palpation, you can detect tension in the muscles of the lower back and abdomen, and an increase in the size of the affected kidney. When tapping the area of the projection of the kidneys with the edge of the palm, pain is noted.
Analysis of urine
In urine tests for acute pyelonephritis, the following changes can be detected:
- a significant number of bacterial cells;
- small amounts of protein (proteinuria);
- leukocyturia - the appearance of a large number of leukocytes in the urine;
- erythrocyturia - the appearance of red blood cells in the urine.
To determine the causative agent of the disease and its sensitivity to antibacterial treatment, bacterial culture of urine is performed.
Ultrasound
Ultrasound examination can give a different picture for different types of pathology.
With primary serous pyelonephritis, the ultrasound picture may not differ from normal. With secondary pyelonephritis of the same stage, examination can reveal signs of compression or blockage of the urinary tract. In this case, the kidney is increased in size and its pelvis is dilated.
As the severity of the disease increases, the condition of the renal tissue changes, its density increases (in the conclusion of a doctor - an ultrasound diagnostician - this is called an increase in the echogenicity of the renal parenchyma).
Apostematous pyelonephritis on ultrasound may not differ from serous one. The difference may only lie in the limited mobility of the organ and the loss of clarity of the outlines in the image.
Examination of a patient with suspected chronic pyelonephritis should begin with ultrasound
A kidney carbuncle on ultrasound is defined as a bulging along the outer contour and the appearance of zones of reduced density in the organ tissue.
With a kidney abscess, a purulent cavity can be detected in the form of a zone of reduced density, surrounded by a dense capsule. Sometimes the fluid level in the cavity is determined.
X-ray examination
X-ray examination for primary serous pyelonephritis is uninformative. However, with purulent forms of the disease, characteristic changes can be identified on x-rays - an increase in size and a change in the contours of the kidney. A transparent halo is found around the affected organ - this is what edematous perinephric tissue looks like. With secondary pyelonephritis, you can see kidney stones and curvature of the spine.
Excretory urography
Excretory urography is an x-ray examination in which the patient is injected intravenously with a contrast agent that does not transmit x-rays and allows one to evaluate the anatomy of the collecting system and the functional activity of the kidneys.
Excretory urography is the second method of instrumental diagnosis of pyelonephritis, which is resorted to if pathology is detected by ultrasound
As an additional measure of differential diagnosis, angiography of the renal vessels (x-ray examination with the introduction of a contrast agent) can be used.
CT scan
In recent years, computed tomography has increasingly been used to diagnose pyelonephritis. During this examination, layer-by-layer images of the organ are taken from different angles. CT scan can detect stones, tumors, and purulent processes in the kidneys. In acute pyelonephritis, swelling and thickening of the kidney tissue (parenchyma) are detected. With a carbuncle or abscess, a purulent cavity with a fluid level can be identified.
Computed tomography has undoubted advantages in visualizing the extent of the inflammatory process beyond the kidney
Differential diagnosis should be carried out with diseases of the abdominal organs (cholecystitis, appendicitis), as well as with inflammatory pathologies of the pelvic organs.
Pearls from the ambulance call cards
Daily work on an ambulance is rightfully considered one of the most difficult and stressful. Indeed, no matter how much hospital doctors shout and beat themselves in the chest about the difficult working conditions of their work, they work indoors, they have a kettle and the opportunity to always pour themselves coffee, and they even have a bed on which to sleep, even if not all night, but at least for a few hours. The ambulance doctor, like the paramedic, is deprived of all this.
( How NOT to call an ambulance, read here ) And of course, the ambulance worker, like the hospital doctor, needs to write a bunch of documents. The hospital doctor writes a medical history, the ambulance doctor fills out a call card. But there are a lot of them, these cards, and there is no way to fill them out somehow later, after - each one must be written either on the call, or immediately after, before the patient is forgotten. That’s why you occasionally find… pearls in cards. There is one phrase in the quick-help jargon: “check it out and be surprised.” Translation: go to the senior doctor’s office in the morning and read the cards written at night. Sometimes you can read something like this... For simplicity, let's go in order of priority in filling out the challenge card, and divide the gems into categories. Let's start by arriving at the call and finding the patient . “Anamnesis: a dead drunk body resembling a man is lying near the post office. There is a strong smell of alcohol from the mouth and other parts of the body...” Or for example: “The patient, having seen the employees of “03”, tried to hide from the team with a positive result” or “the presence of the patient’s body, both in an unconscious and in a conscious state of consciousness, was not detected at the indicated address.” Well, or this: “At the place of the call, a sweatshirt and trampled grass were found in the bushes; the body was not found, it probably crawled away.”
( Read the most ridiculous cases from the practice of doctors here ) But it rarely happens as it is written. More often than not, the patient is found, like this one: “A male body, reeking of fumes like a dragon with fire,” the passport part of the card is filled out: “We only managed to find out the name and age, all other statements cannot be deciphered.” And then the collection of anamnesis , which, translated from everyday Latin, means the history of life and illness. And here’s the thing: “Anamnesis: it was not possible to obtain additional information due to the patient’s lack of teeth and the valiant police at the scene of the call.” And one more thing: “He sent a team in the direction of the female genital organs with obscene language” or “when trying to wake up the patient, he shrugs it off and intends to bite members of the team; in order to avoid injuries at the workplace, further examination of the patient was carried out gently and carefully.” Well, or like this: “The patient, using all the charm and breadth of the Russian language, asked to be left alone,” or “Taking an anamnesis: where he hung around until 5 in the morning is unknown, he is silent like a fish and does not answer questions.” But in my opinion, the champion is: “He doesn’t make any complaints, he sits drunk on the toilet, he didn’t call “03”, he sends curse words in three letters. “03” was called by my wife to be removed from the toilet because she wanted to go to the toilet.” It often happens that people cause injury. In this case, the medical history also includes the circumstances of the injury. The circumstances can be varied: “According to the patient, she poured the cockroach poison “Mashenka”. The cockroach ate this poison, swelled up, escaped from the patient’s hand, jumped into the right ear and immediately crawled into the brain” (don’t be surprised, a cockroach in the ear, this is also an injury, a foreign body, more precisely). And it happens: “Anamnesis: a man is sitting in a trash can, saying that the boys beat him up.” Or this: “A man was hit by a regular bus (on the legs). The man left, the bus left. The traffic police didn’t come.” And it also happens that: “According to the patient: during joint alcoholism with a stranger in his own kitchen, as a result of the discussion that arose, the patient was hit on the forehead with a vodka bottle” or “...I received an injury by falling from a garbage can and hitting my head on land. He refused to tell me what he was doing in the trash can.” Another example: “I got off the bus with my head hitting the asphalt.” Well, the favorite of the section: “I received the wound in a fight. Then he went to the emergency room for medical help, where he received it. I did not receive treatment." Source: Young Specialist, ria-ami.ru
Treatment options
Acute pyelonephritis is treated by urologists and nephrologists. In some cases, a consultation with a gynecologist may be required.
Treatment of acute pyelonephritis must be carried out in a hospital setting. Treatment tactics for different clinical forms of the disease may differ significantly.
Mandatory conditions for any form of pathology are strict bed rest, a special diet and plenty of fluids.
Drug therapy
Immediately after hospitalization, patients are prescribed broad-spectrum antibiotics that are active against pathogens. The most commonly used groups are:
- Third generation cephalosporins - Cefixime, Ceftriaxone. Ceftriaxone is prescribed intramuscularly. Cefixime is taken orally;
- fluoroquinolones - Ciprofloxacin, Ofloxacin. Depending on the severity of the condition, medications may be prescribed in the form of tablets to be taken orally or as intramuscular injections;
- carbapenems - most often prescribed Meropenem or Imipenem;
- aminoglycosides - Gentamicin, Tobramycin. The appointment of this group should be approached with caution, as they have a pronounced toxic effect on the kidneys.
The duration of antibiotic treatment ranges from 10 to 14 days.
In addition to antibiotics, antimicrobial drugs from different chemical groups are prescribed:
- nirofurans - Furazolidone, Furagin, Nitroxoline;
- nalidixic acid preparations - Nevigramon;
- 8-hydroxyquinoline derivatives - drug 5-NOK;
- herbal preparations - Canephron. Available in drops and tablets. Treatment during pregnancy and childhood is allowed.
To reduce the activity of the inflammatory process, drugs from the group of non-steroidal anti-inflammatory drugs are prescribed. These medications reduce pain, swelling and inflammation, and lower body temperature. The most effective and least toxic for pyelonephritis are Diclofenac and Voltaren. The duration of treatment is 3–4 weeks.
To improve renal blood flow, Pentoxifylline (Trental), Curantil, and Troxevasin are prescribed. These substances prevent the formation of blood clots in the vessels of the kidneys, improve blood flow and microcirculation. The outflow of venous blood from the kidneys is also activated.
The drug Heparin occupies a special place in treatment. It reduces platelet aggregation, improves blood circulation in the capillaries of the kidneys, has an anti-inflammatory effect, and suppresses the body's immune aggression towards its own proteins. It is prescribed as an injection under the skin of the abdomen.
To enhance immunity, drugs from the group of immunomodulators are prescribed:
- Levamisole (Decaris);
- Timalin;
- T-activin.
To improve your general condition, it is recommended to take multivitamin complexes and adaptogens - pharmaceutical tincture of ginseng or eleutherococcus in drops.
Photo gallery: medicines
Ceftriaxone is a long-acting cephalosporin antibiotic.
Nitroxoline is a broad-spectrum antimicrobial drug for the treatment of urinary tract infections
5-NOK is able to fight pathogens
Canephron has a pronounced antimicrobial, antispasmodic and anti-inflammatory effect
Heparin improves blood circulation in capillaries
Folk remedies
In addition to drug treatment, herbal medicine is widely used. Healing plants that are used in the treatment of kidney diseases have anti-inflammatory, antimicrobial, diuretic and hemostatic effects.
Traditional recipes:
- The bearberry plant, or bear's ears, has an antiseptic effect. To prepare the infusion, 30 grams of crushed herbs are poured into 500 ml of boiling water and infused for an hour. Take 2 tablespoons every 2 hours. To improve the effect, the infusion is combined with alkaline mineral waters.
Bearberry leaves are a natural medicine known since ancient times. - Lingonberry leaf has a diuretic and antimicrobial effect. An infusion is prepared from it. To do this, pour 2 tablespoons of leaves into 300 ml of boiling water and leave for 1 hour. Take 2 tablespoons every 2-3 hours.
Decoctions and infusions of medicinal herbs should be taken for a long time - from 3 months to several years.
It is very useful to eat watermelons during the summer and autumn seasons. They have a diuretic effect and help remove toxins from the kidneys.
Tables: medications for pyelonephritis
| Collection No. 1 | Herbal component | Quantity | Cooking method | Admission procedure |
| Rosemary stems | 5 parts | 2-3 tablespoons of the medicinal mixture are poured with boiling water (0.5 liters) and placed in a thermos for 6 hours. You can leave it overnight. | Take 150 ml warm 3 times a day half an hour before meals. | |
| St. John's wort herb | 5 parts | |||
| Corn silk | 3 parts | |||
| Flax-seed | 2 parts | |||
| Mint leaves | 3 parts | |||
| Pine buds | 3 parts | |||
| Veronica grass | 5 parts | |||
| Horsetail | 4 parts | |||
| Collection No. 2 | Calamus root | 2 tsp. | 3 tablespoons of the herbal mixture are poured into 500 ml of boiling water and infused in a thermos for 6 hours. | 500 ml of infusion is divided into 3 doses. Drink warm half an hour before meals |
| St. John's wort herb | 5 tsp. | |||
| Fennel fruit | 2 tsp. | |||
| Kidney tea leaves | 3 tsp. | |||
| Flax seeds | 3 tsp. | |||
| Melissa herb | 2 tsp. | |||
| Bearberry grass | 5 tsp. | |||
| Elder flowers | 4 tsp. |
Surgical intervention
Indications for surgical treatment for acute pyelonephritis are the following conditions:
- all stages of secondary pyelonephritis, when it is not possible to restore the flow of urine by other means;
- primary purulent pyelonephritis - carbuncle or kidney abscess;
- ineffectiveness of conservative treatment for more than 3 days;
- the threat of developing bacteremic shock - a life-threatening condition caused by the massive release of a pathogen into the bloodstream. Clinically expressed in severe chills and a sharp decrease in blood pressure;
- severe intoxication, manifested by general weakness, loss of appetite, vomiting, immobility, and decreased hemoglobin.
Surgical treatment may be contraindicated if the patient has severe concomitant diseases - acute myocardial infarction, severe heart failure or diabetes mellitus.
Surgical interventions are performed under general anesthesia. All of them can be conditionally divided into 2 groups:
- Interventions aimed at restoring urine outflow in secondary pyelonephritis. These include:
- removal of stones;
- removal of part of the ureter at the site of its pathological narrowing;
- removal of tumors compressing the kidney or ureter.
- Kidney surgery for acute purulent process. This group includes:
- removal of the kidney capsule;
- opening and removal of ulcers;
- removal of the entire kidney if its condition is severe;
- removal of drainage from the kidney (nephrostomy).
In the postoperative period, the patient needs intensive treatment, which is aimed at eliminating microbial flora, reducing intoxication, maintaining the functioning of the heart and other organs. Care of the wound and the drainage tube that is left in the renal pelvis is very important. This device is removed on the 24th day after surgery. After discharge from the hospital, the patient continues to receive treatment on an outpatient basis. Since surgical treatment does not guarantee the absence of recurrent inflammatory processes in the future, the patient should remain under medical supervision throughout the rest of his life.
Reviews
I experienced pyelonephritis two years ago, was treated in the hospital, but not very well - for six months there were exacerbations, I took antibiotics, which gave a very temporary effect. Then for 2 months I took a tincture of propolis (homemade) and herbs (bearberry, lingonberry leaf) and for a year and a half nothing has appeared
nancy girl
https://club.passion.ru/zhenskoe-zdorove/pielonefrit-t106974.html
But I have a different opinion: pyeloniphritis manifests itself and is treated differently in everyone; I was diagnosed with this disease a year ago in July. The course of treatment was about 20 days. Moreover, antibiotics last for about 14 days. Within a month I was completely cured. And in order not to get sick later, you need to take care of yourself. You need to be careful with air conditioners (at home, in the office, in the car), in spring-autumn-winter, no shot jackets and blouses. Yesterday my close friend’s stepfather died (as her father was) of her kidneys!!! So the kidneys must be treated, and then carefully protected!! And less beer, I love it terribly, but it’s poison for the kidneys.
Vasyunya
https://club.passion.ru/zhenskoe-zdorove/pielonefrit-t106974.html
Five days of antibiotics only relieved your symptoms (I know from personal experience there is nothing good about this), but the treatment should last 2-3 months and the treatment should be systemic. If you are not treated well now, you will later suffer from chronic pyelonephritis, I experienced this myself.
Yumi
https://club.passion.ru/zhenskoe-zdorove/pielonefrit-t106974.html
Treatment of infection
Treatment of pyelonephritis should be comprehensive and include, in addition to medication, diet. In case of kidney disease of this kind, it is necessary to eat low-fat foods, avoid fried, spicy, and excessively salty foods. It is also prohibited to consume any foods that are bright red in color.
When treating kidneys, antibiotics are mainly prescribed, and the patient must undergo a full course of treatment in order to completely destroy the bacteria inside his body. Painkillers are also prescribed for severe pain.
However, unfortunately, such a disease can return and become chronic . Therefore, it is necessary to undergo regular diagnostics to identify this disease. “SM-Clinic” makes it possible to start treatment in a timely manner under the supervision of experienced specialists.
Sources:
- Bergeron MG Treatment of pyelonephritis in adults / MG Bergeron // Med. Clin. North Amer. Antimicrobial Therapy. - 1995. - Vol. 79. - No. 3. - P. 619-649.
- Nekrasova A.A. Be careful - pyelonephritis! / A.A. Nekrasova // Atmosphere. Cardiology. - 2004. - No. 2. - P. 40-41.
- Rumyantsev A.Sh. Etiology and pathogenesis of pyelonephritis / A.Sh. Rumyantsev, N.S. Goncharova // Nephrology. - 2000. - T. 4. - No. 3. - P. 40-52.
- Styazhkina S.N. Structure of incidence of pyelonephritis / S.N. Styazhkina [and others] // Problems of modern science and education. — 2016.
Pyelonephritis: do's and don'ts
If a patient is diagnosed with pyelonephritis, it is very important to adhere to certain rules and remember what can be done and what is strictly contraindicated:
- To reduce the load on your kidneys, you should reduce the amount of protein in your diet. However, the amount of fats and carbohydrates may remain the same.
- If the patient has severe edema, the amount of fluid should be limited to 1 liter per day (including first courses and drinks). Salt should be completely eliminated during the acute period of the disease.
- Be sure to avoid alcohol.
- Under no circumstances should you heat your kidneys during the acute period of the disease. This can lead to increased inflammation and spread of infection to other areas of the body.
- During the acute process, you should limit any physical activity and maintain bed rest. This recommendation also applies to sex.
Patients with pyelonephritis need to follow certain rules to protect their kidneys
What is killing your kidneys: video
Lifestyle with pyelonephritis
With pyelonephritis, it is necessary to follow some rules in your lifestyle in order to help the body cope with the disease.
First of all, you should give up bad habits, namely smoking and alcohol. Refusal of them improves protective functions and improves blood supply to the body.
- Diet for pyelonephritis: the importance of proper nutrition in eliminating renal pathology
Acute pyelonephritis requires bed rest; any physical activity is contraindicated. During the acute phase of the disease, it is forbidden to have sex, visit the pool and open water bodies to avoid hypothermia, and also not visit saunas and baths. But warm baths with a water temperature in the range of 36-37 degrees, on the contrary, are shown.
The chronic course of pyelonephritis allows sexual contact, visiting pools and ponds, but subject to the thermal regime, dosed physical activity.
Prognosis and possible complications
If the patient is correctly diagnosed and given competent and timely treatment, recovery occurs in 2–3 weeks.
In approximately 30% of cases, the disease becomes chronic. The consequence of this may be sclerosis of the kidney (degeneration of renal tissue into connective tissue) and the development of nephrogenic arterial hypertension (persistent increase in blood pressure caused by renal pathology).
Complications of acute pyelonephritis include:
- paranephritis - inflammation of the perinephric tissue;
- retroperitonitis - inflammatory process of the retroperitoneal space;
- renal failure;
- bacteremic shock;
- sepsis;
- meningitis is an inflammation of the membranes of the brain.
These complications often cause the death of the patient.
Manifestation of symptoms
Clinical manifestations of UTI can appear already at the initial stage of the disease. But the process of infectious inflammation can also be asymptomatic for a long time.
A urinary tract infection can present with various symptoms:
- pain in the pelvic area, lower back, side;
- itching in the urethra;
- burning sensation, pain, difficulty urinating;
- increased urge to urinate;
- uncharacteristic liquid discharge from the bladder (clear, serous, greenish-purulent);
- hyperthermia, chills, fever;
- change in odor and color of urine.
In children, especially younger children, the symptoms of UTIs may be even more vague than in adults.
Parents may notice an increase in urination, traces of unusually colored urine on the diaper, and an increase in body temperature.
Disease prevention
Prevention measures include:
- drinking enough fluid - about 2 liters per day. People who engage in physical labor or sports should drink even more fluids;
- compliance with personal hygiene rules. You can prevent infection from entering the urinary tract by toileting your genitals every day and regularly changing your underwear. In addition, you should shower after sexual intercourse;
- increasing immunity. This can be achieved by regular physical exercise, spending time in the fresh air and nutritious nutrition;
- avoiding physical overload and hypothermia;
- treatment of chronic infections of the genital organs, oral cavity, and upper respiratory tract.
To avoid the disease becoming chronic, you must carefully follow your doctor’s prescriptions and regularly undergo kidney examinations.
With proper and timely treatment, the outcome of the disease is favorable in most cases. However, sometimes complications may develop and the disease may become chronic. To prevent this, patients who have suffered acute pyelonephritis need systematic monitoring by a urologist or nephrologist. It is very important to get tested regularly. According to indications, the doctor prescribes maintenance treatment. Uncontrolled use of medications is unacceptable, as this can lead to a worsening of the condition.
Rehabilitation
If you managed to stop the acute inflammatory process, this does not mean that you managed to completely cope with the disease. To prevent pyelonephritis from developing into a chronic form, it is important to undergo proper rehabilitation. A set of measures, including massage, physiotherapy, and exercise therapy, will allow you to completely return to a normal lifestyle.
Massage for pyelonephritis
After acute inflammation of the kidneys, a special therapeutic massage will help restore the function of the organ much faster. The session must be conducted by a qualified specialist. It is strictly forbidden to aggressively influence the lumbar region, as this can provoke a new inflammatory process. The main elements of therapeutic massage are light stroking, rubbing, and vibration.
Therapeutic massage will help restore kidney health
If you have had to endure a severe form of pyelonephritis, nephrologists recommend repeating therapeutic massage periodically 2-3 times a year for several more years for preventive purposes. The kidneys remain weakened after the disease, and proper massage helps prevent the development of re-inflammation.
Physical exercise
Immediately after an acute period of inflammation, you will have to avoid the usual physical activity. This is especially true for those people who play sports or lead an active lifestyle. Any actions should be performed only with the permission of a doctor.
Physical therapy helps restore health well. A set of exercises should also be selected by a specialist in accordance with the patient’s age, as well as the characteristics of the disease.
Video: effective exercises for the kidneys
Physiotherapy
Not a single inflammatory disease can occur without the use of physiotherapy during the rehabilitation period. With the help of such procedures, it is possible to improve blood circulation, increase the body's defenses, and remove residual effects of the pathological process. For pyelonephritis, the following methods are considered the most effective:
- UHF therapy. The treatment is carried out using an electric field with ultra-high frequency. The area of inflammation is exposed for 10–15 minutes, which improves blood circulation and relieves pain.
- Magnetotherapy. Using a constant or pulsed magnetic field, it is possible to relieve kidney swelling, improve blood flow, and increase local immunity.
- Electrophoresis. Medicinal substances that help eliminate the inflammatory process are administered through the skin using an electric current.
- Laser therapy. Treatment is carried out using low-intensity laser radiation. Thus, it is possible to achieve a vasodilating and immunostimulating effect.
Magnetic therapy is one of the methods of rehabilitation after pyelonephritis
Visit to the bathhouse and spa treatment
A useful way to prevent kidney inflammation is a bath or sauna. With its help, those who were unable to avoid pyelonephritis will be able to recover. However, any thermal procedures should be carried out only after the acute inflammatory process has stopped and with the permission of the attending physician.
You should start visiting the bathhouse gradually. It is recommended to stay in the steam room for no more than 20 minutes for the first time. Then this time can increase by 5-10 minutes each time. The maximum session should last no more than an hour. If you visit the bathhouse every day for a month, you will be able to completely restore your kidney health.
People who have suffered severe pyelonephritis are advised to undergo sanatorium-resort treatment with the physiotherapeutic procedures described above. In addition, there will be medicinal baths, mineral water intake, etc.
Prevention
Prevention of acute pyelonephritis involves identifying clinical situations that may lead to pyelonephritis and developing strategies to reduce this likelihood. These strategies may include changes in contraceptive use, prophylactic antibiotics, or early detection and treatment of cystitis.
If these strategies do not resolve the infection or its recurrence (repeated less than 14 days after completion of the appropriate regimen), the patient should undergo systematic evaluation for predisposing anatomical, functional, or structural abnormalities.
Diagnostic methods
A preliminary diagnosis is made after an analysis of the patient’s complaints by a therapist or urologist. To confirm the diagnosis and draw up a set of treatment measures, the following are prescribed:
- general clinical analysis of blood and urine;
- biochemical analysis of blood and urine (metabolic indicators such as urea, creatinine, and some enzymes characterize kidney activity);
- bacteriological culture of urine or PCR analysis (to determine the nature of the causative agent of the disease);
- instrumental research methods (cystoscopy, biopsy, urography, X-ray contrast studies, ultrasound of the kidneys and bladder).
Timely and comprehensive diagnosis makes it possible to identify the disease at an early stage and prevent the spread of the inflammatory process.