Diagnosis of diseases of the urinary system consists of laboratory tests, ultrasound of the urinary system and the use of other laboratory and instrumental diagnostic methods that will help identify the problem. This will make it easier to choose a drug treatment regimen. What does diagnostics of the urinary system include, how to properly prepare for it, and what features are important to observe in order to get the most accurate results?
Indications
If a person is concerned about problems with the functioning of the genitourinary system, he should immediately seek medical help. Problems can be very diverse - from the occurrence of an inflammatory process to cancer. Indications for prescribing a diagnostic study:
- development of discomfort during urination;
- temperature that cannot be brought down at home;
- development of pain symptoms in the lumbar region;
- the presence of blood, mucous and purulent inclusions in the urine;
- deterioration of the patient's general condition;
- rapid decrease in body weight.
During the diagnostic study, the doctor identifies the root cause and at what stage the disease is. A correct diagnosis guarantees a quick cure, which prevents the development of a serious complication. The patient needs to work closely with the doctor, then the prognosis for a successful recovery increases.
First inspection
During the initial examination by a doctor, it is important for the patient to remember when the condition first worsened and what primary symptoms appeared. It is important for the doctor to know whether there have been other cases of illness, how the treatment was carried out, what antibiotics or other medications were used. Based on the collected data, the doctor has a primary picture of the diagnosis, but to clarify it, other diagnostic measures must be taken.
Inspection and palpation
Visual examination should not be limited to simply examining the patient. A detailed palpation of the abdominal cavity is performed and symmetry is determined. With the development of inflammation and other kidney diseases, the lumbar region is asymmetrical and the muscles are hot. If a cancerous tumor develops on the bladder or ureters, the abdominal cavity enlarges, as the excretion of urine from the body is impaired, which provokes inflammation. If women or men develop a urinary tract infection, the external genitalia will be irritated and may develop rashes and pus-filled lesions.
Examination of the urinary system organs
Of the X-ray studies of the urinary system, cystourethrography, cystography, and especially ureteropyelography are of well-known interest.
Cystourethrography
A valuable diagnostic method for studying women suffering from urinary incontinence is cystourethrography.
After filling the bladder with a 5% suspension of barium, sergosine or other contrast agent and inserting a metal chain into the urethra, frontal and lateral x-rays are taken both at rest and with increased intra-abdominal pressure.
Cystourethrograms determine:
- the height of the bottom of the bladder in relation to the pubic bones;
- vesicalization of the urethra and a detectable funnel (neck) of the bladder, the size of which is determined by the angle of its apex;
- localization of the internal opening of the urethra on the contour of the bladder.
In this case, it is easy to note the following pictures; a) a normal picture of the closing apparatus of the bladder (the weakened urinary continence observed in these cases often depends on a violation of innervation, and not only on topographic-anatomical relationships); b) rotational depression of the bladder or prolapse of the bottom of the bladder (cystocele) with or without vesicalization of the urethra; c) vertical displacement of the bladder, indicating disorders in the supporting and fixing apparatus of the upper third of the urethra. It is judged by the angle of the infundibulum apex (straight or acute) on the lateral cystogram with increased abdominal pressure. These studies not only clarify the type and causes of urinary incontinence, but also make it possible to objectively monitor the results of the applied conservative or surgical treatment.
Cystography
Although a cystoscopic examination of the bladder gives us the most accurate idea of the pathological changes occurring in it, but still in a number of cases, for example, when it is felt with the formation of a cystocele, with bleeding tumors that prevent a more detailed examination of them with the naked eye, and finally, for objective monitoring of changes configuration and capacity of the bladder after x-ray or radiotherapy, fluoroscopy (graphy) of the bladder is of undoubted interest.
Ray research is carried out in a variety of ways; in some cases (for example, in the presence of foreign bodies, solid tumors), a survey photograph is taken with an empty bladder, but in most cases the bladder is filled with a contrast solution, thanks to which we can get an idea of the shape, size, deformation of the bladder, etc. in the picture.
To fill the bladder, use a 2% (some even 8%) solution of collargol (introducing 200 ml), 10% sodium bromide solution or other contrast agents.
The technique for examining the bladder with X-rays is as follows: after filling the bladder, the patient is laid with her back on the X-ray film (size 18 x 24 cm) so that its upper edge is at the lower edge of the chest. The diaphragm is installed above the upper edge of the symphysis.
If a pressing tube is used, then the edge of the lower opening of the latter should be pressed against the abdominal wall at the horizontal branch of the pubic bone. The tube is installed somewhat obliquely (from top to bottom) so that the shadow of the symphysis pubis does not fall on the bladder.
If the photo is taken successfully, the image of the sacrum is visible on the film.
Filling the bladder before the sensation of urge appears is generally only suitable for determining the shape (contours) of the bladder; To identify tumors, diverticula, and intravesical processes, cystography in this form is unsuitable, and the introduction of small amounts of contrast agents should be preferred. The decisive sign of urinary incontinence is the lowest location of the point of origin of the urethra. Among women with vertical prolapse of the bladder, according to our observations, 82% suffered from urinary incontinence, and with rotatory prolapse of the bladder, incontinence was found in only 15%. The anterior vesicourethral angle and the lateral shape of the funnel do not have any particular diagnostic value. On a lateral radiograph of the bladder, the most important are: 1) the angle between the long axis of the urethra at rest and during straining, 2) the urethrosymphyseal angle.
Ureteropyelography
The introduction of cystoscopic examination into practice made it possible for the first time to observe changes in the upper urinary tract; Initially, judgments about changes in the ureters and renal pelvis were made on the basis of the results of catheterization of the ureters based on the amount (and properties) of urine flowing from them.
Retrograde ureteropyelography
With the advent of contrast agents, they began to be injected into the renal pelvis retrogradely, through ureteral catheters, and thus the method of retrograde ureteropyelography was developed, which made it possible to elucidate a number of interesting changes in gynecological diseases (cervical cancer, tumors of the internal genital organs, genitourinary fistulas), changes in normal pregnancy and various forms of its pathology, especially with pyelitis (A. M. Mazhbits, A. L. Petrov, etc.), etc. In particular, with the help of this method, such frequent dilations of the ureters and pelvis with cancer parametritis have been established.
Research by E. S. Tumanova has reliably revealed that with uterine prolapse, there is extremely often an expansion of not only the ureters, but also the renal pelvis up to the upper calyces.
On the other hand, studies using retrograde pyelography have shown that even with extensive prolapses involving the entire bladder triangle, there may be no dilation of the ureters.
Likewise, there are cases of hydronephrosis of quite significant magnitude with non-dilated ureters, which indicates the presence of good tone of the ureters with reduced elasticity of the walls of the renal pelvis and calyces.
The cause of isolated dilations obviously lies in weakness or defects in the development of the smooth muscles of the corresponding parts of the urinary organs.
With the usual filling of the pelvis with iodolipol, the images (especially in the absence of changes in the ureters) clearly show the contours of the pelvis and often the bladder, but not the ureters.
For retrograde ureteropyelography, a 40% sergosine solution can also be used as a contrast agent, which is injected heated to 37° through the ureteral catheters in an amount of 6-8 ml. This makes it possible to obtain clear images of the urinary tract on X-rays.
Sergozin does not cause any irritation from the pelvis. Retrograde pyelography does not replace intravenous urography, but complements it.
Retrograde ureteropyelography provides indispensable services in recognizing renal dystopia. The figure shows a pelvic kidney with a sharply curved ureter.
Despite a number of advantages, ureteropyelography could not become particularly widespread, on the one hand, because it is technically quite difficult or often (for example, with fistulas) even impossible, and on the other hand, it is not without a number of negative aspects.
In some cases, mainly due to overstretching of the urinary tract with a contrast mass introduced under pressure, pyelovenous reflux is observed, that is, the entry of a contrast agent into the venous system of the kidney; The images obtained during artificial dilatation of the upper urinary tract may give rise to incorrect conclusions about the presence of dilatation of the pelvis or ureter. Hence the desire to find a more physiological and safe way naturally arose.
Intravenous ureteropyelography (resp. urography)
The introduction of uroselectan practically resolved this important issue. Soon other high-quality and harmless drugs for intravenous pyelography appeared (Abrodil, our domestic drug Sergozine, urografin, etc.).
The main advantage of intravenous urography is that it makes it possible, under conditions that are closest to natural, to judge not only the anatomical and dynamic state of the urinary tract.
This method is technically simple, safe, eliminates the possibility of transfer of infection to the upper urinary tract, and produces clear contours in the image. The patient being studied should thoroughly cleanse the intestines the day before with a laxative, and in the morning, in addition, give herself an enema. The study is performed on an empty stomach.
Ex tempore, a 40% solution of sergosine (in saline solution) or another water-soluble substance is prepared and 50 ml of it is administered intravenously; however, as a rule, no side effects are observed.
In some cases, there is pain along the vein at the time of infusion of the solution, but this pain, radiating to the shoulder joint or neck, goes away after a few minutes.
Usually, after 5 minutes, the contours of the renal pelvis and ureters are clearly visible on the x-ray; after 15 minutes the contrast is much more pronounced, and after 30-35 minutes it disappears.
Intravenous pyelography is indispensable for strictures, blockage, compression, damage to the integrity of the ureters, for malformations of the upper urinary tract (recognition of aplasia of the kidney, horseshoe kidney; duplication of the ureters and much more) and for determining the excretory capacity of the kidneys. In view of this, it has acquired the significance of an important auxiliary method for judging the condition of the urinary organs not only in urological practice, but also in various diseases of the genital area.
Source: https://ginekolog.my1.ru/publ/ginekolog/metody_obsledovanija_bolnykh/issledovanie_organov_mochevoj_sistemy/6-1-0-285
Laboratory diagnostics
General blood and urine analysis
The patient is referred for a general analysis of urine and blood - OAM and OAC. If inflammation of the kidneys, urethra or bladder is complicated by a bacterial infection, then urine and blood tests will differ from those in healthy people. The results will show a significant excess of the norms for such blood inclusions as leukocytes, red blood cells, casts, and protein. If the kidneys are involved in the inflammatory process, blood, mucous and purulent inclusions will be visible in the urine.
Blood chemistry
A biochemical blood test allows you to identify such dangerous diseases as renal failure, the development of cancer, and severe pathologies of the genitourinary system. With renal failure, keratin, urea and uric acid in the blood plasma increase. If bladder cancer develops in adults, the tumor markers of the genitourinary system will exceed the norm, therefore, to exclude such dangerous pathologies, a person is prescribed a biochemical analysis.
Radioisotope research
Radioisotope research - all methods are based on the same principle: isotopes of various chemical elements take part in physiological processes occurring in the body, just like similar stable (radioactive) substances. The introduction of radionuclides into the body makes it possible to determine with high reliability their quantity in organs and biological environments (taking into account the activity administered to the patient).
- Scanning - used to examine the liver, pancreas, kidneys, and thyroid gland.
To perform the scan, Au (198) or J (131) is injected into the patient intravenously. The scan is performed after 40-50 minutes using a special device - a scanner, the main part of which is a nuclear radiation detector that automatically moves over the area of the organ under study in two perpendicular directions. Using a special writing device, the results of activity measurements are recorded on paper or photographic film in the form of strokes, line by line, and the frequency and intensity of the strokes depend on the activity accumulated in the organ.
Thus, as a result of scanning, a scanogram is obtained - a planar image of the organ under study, which allows one to judge by the nature of the shading the degree, characteristics of the accumulation and distribution of the isotope in the tissues of the organ. Currently, color scanning is used, in which areas of the scanogram with different degrees of isotope filling are reproduced in different colors. When assessing a scanogram, the size and shape of the image, the intensity of shading in various areas, and the presence of “filling defects”—the absence of shading in certain areas—are taken into account.
- Functional study of organs and systems is based on one principle: determining the rate and degree of intake, accumulation or distribution and excretion of isotopes and labeled compounds in organs and systems of the body.
A radioactive element is usually injected into the patient intravenously, and then, using sensors of radiometric devices, the radiation emanating from organs or tissues is detected and recorded in the form of a graphic image or in digital values.
This method is currently most widely used to diagnose thyroid pathology, for example, a biphasic radioiodine test, the results of which reflect the accumulation of J 131 in the thyroid gland or the concentration of iodine in the plasma.
- Radioimmunohormonal studies - in recent years, this type of radioisotope diagnostics has become increasingly important, because Compared to conventional immune and biochemical diagnostics, it has very high sensitivity and specificity and allows you to determine the content of many hormones and enzymes in the blood serum.
The study is carried out “in vitro”, the material being studied is the patient’s blood serum, to which is added the corresponding labeled hormone with a certain activity, as well as specific antibodies
.
Then, in comparison with special standards, the enzyme concentration of the aphid hormone being studied is determined with a high degree of accuracy, for example, endogenous insulin
, pepsin, angiotensin, gastrin, secretin.
Tests for sexually transmitted infections
Smear examinations
During a gynecological examination, the doctor takes a smear from the woman’s urethra and vagina, which is then sent to the laboratory for analysis. If there are no pathogens in the body, then the results will be clean. If you receive positive results, you need to go to a gynecologist or urologist so that he can assess the situation and decide on treatment.
Culture and cytology
Cultures are taken to identify genitourinary infections and to identify the presence of sensitivity to antibacterial drugs, which is important for treatment. During the course of therapy, the doctor examines the data and prescribes a narrow-spectrum antibiotic, which copes with pathogenic microflora in a short time, which speeds up recovery.
To get the most accurate results, preparatory procedures are agreed upon with the doctor.
If the development of infectious diseases of the genitourinary system in the female half of the population is suspected, a cytological analysis of the smear is important. This method will allow you to identify pathological inclusions in the smear. If the tumor is cancerous, abnormal cells will be present in the sample. The procedure does not bring pain or discomfort, the smear is taken with a special sterile stick, so there are no complications after the manipulations.
Sperm research
Diagnosis of the genitourinary system in men is based on sperm examination. The sample is collected in a special sterile container, diagnostics is carried out in no more than 10 minutes. If the man was unable to obtain a sample, he will need to urinate into a container, then the doctor will examine the activity of sperm that have entered the urine. If the indicators do not correspond to the norm, tests should be taken a week later, and then on the 21st day.
Endoscopic studies
Endoscopy (endo-inside, scopo-look) is a method of visual examination using optical-mechanical lighting devices. The development of fiber optics and the creation of fiberscopes (flexible endoscopes) based on it have made this method safe and effective not only for diagnosis, but also for the treatment of many pathological conditions.
Modern fiber endoscopes are complex in their design; in them, light is transmitted through a fiber - a light guide, with a diameter of several tens of microns; the fibers are folded into bundles, from which they form a fiber-optic endoscope system, which is covered with a protective shell and placed inside a flexible tube.
- FEGDS - fibroesophagogastroduodenoscopy - examination of the esophagus, stomach and duodenum - allows you to assess the lumen and condition of the mucous membrane of the esophagus, stomach and duodenum - color, the presence of erosions, ulcers, neoplasms, the condition of the vessels, the presence of hemorrhages, the nature of mucus secretion, the nature of the folds, conduct a targeted biopsy, determine the acidity of gastric juice, perform a polypectomy, stop bleeding, apply medications locally.
Contraindications – narrowing of the esophagus or cardia as a result of a tumor, esophageal diverticula, pathological processes in the mediastinum that displace the esophagus (aortic aneurysm, enlarged left atrium), severe scoliosis
.
Complications – perforation of the esophagus or stomach, allergic reactions or anaphylactic shock
for
lidocaine
, traumatic laryngotracheitis, injuries to organ walls, wrapping the endoscope in the lumen of an organ, aspiration pneumonia.
- RRS -
sigmoidoscopy - examination of the rectum and sigmoid colon -
allows you to directly examine the mucous membrane of the rectum and sigmoid colon (the rectoscope is inserted to a depth of 25-30 cm), identify the presence of an inflammatory process, internal hemorrhoids, erosion, hemorrhage, neoplasms, conduct a targeted biopsy, obtain smears , perform scrapings from the mucous membrane.
Contraindications – ulcerative colitis in the acute stage, strangulated hemorrhoids, anal fissures in the acute stage.
Complications – intestinal perforation, intestinal bleeding.
- Colonoscopy
- an examination of the colon -
allows you to directly examine the mucous membrane of the colon, identify the presence of an inflammatory process, internal hemorrhoids, fissures, erosion, hemorrhage, neoplasms, conduct a targeted biopsy, obtain smears, and perform scrapings from the mucosa.
Contraindications – intestinal obstruction, decompensated circulatory failure, nonspecific ulcerative colitis
in the acute stage, profuse intestinal bleeding, stage III hypertension.
Complications - perforation of the intestine during exacerbation of ulcerative colitis, severe pain reaction to tension of the mesentery, trauma and bleeding.
Capsule intestinoscopy involves the patient swallowing a special capsule equipped with a miniature video camera, a processor, and a system for transmitting information. As it passes through the intestines, the capsule continuously, at a speed of 2 frames per second, transmits a video image to a semiconductor recording device through a system of sensors attached to the skin of the abdomen. Later, the recording device is connected to a computer workstation where the images are processed and can be viewed on a monitor and printed. The total number of images is more than 50,000. This method can detect ulcerative lesions of the small intestine, helminthiasis, bleeding from the small intestine or functional disorders of intestinal motility. Modern capsules can be controlled by changing the magnetic field applied to the abdominal wall.
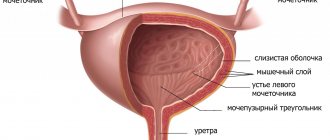
- Cystoscopy - examination of the bladder cavity - allows you to directly examine the walls of the bladder, identify the presence of an inflammatory process, neoplasm, and conduct a targeted biopsy.
Contraindications: tumors of the urethra.
Complications – organ injuries, bleeding, functional disorders, infection of cavities and organs.
- Bronchoscopy - for diagnosing erosions and ulcers of the bronchial mucosa, removing foreign bodies, removing bronchial polyps, treating bronchiectasis and centrally located lung abscesses, administering medications, performing targeted biopsies.
Contraindications – acute heart failure
.
Complications – collapsed state, damage to the walls of the bronchus, an allergic reaction to the anesthetic.
Methods of instrumental diagnostics of the genitourinary system
Inspection with a mirror
Examination with a mirror is included in instrumental diagnostic methods and allows the gynecologist to assess the condition of the vaginal mucosa and external genitalia. If necessary, during the examination the doctor takes a smear for a more detailed diagnosis. During colposcopy, the condition of the uterine tissue is determined, whether there are wounds, erosions or other neoplasms there. In suspicious areas, material is taken for histology. During hysterosalpingography, X-rays with contrast are used, with which the doctor examines the tissue of the uterus and the patency of the fallopian tubes.
Ultrasound, CT and MRI and preparation
Ultrasound of the urethra allows you to assess the condition of the tissues of the bladder, urethra, and kidneys. The doctor sees on the monitor all changes and pathologies in real time, which is important when making the correct diagnosis. In order for the results to be accurate, the day before you need to get rid of intestinal gases and fecal inclusions. If the doctor sees suspicious tumors on the bladder or kidneys, he will refer the patient to a CT or MRI with contrast.
MRI and CT scans of the kidneys and urinary tract allow you to see even the smallest tumor that cannot be seen on ultrasound. The contrast makes it possible to examine the tissue structure in more detail and see pathological changes there. These diagnostic methods differ in that with CT, the patient is exposed to radiation, and with MRI, the properties of the magnetic field are used.
Instrumental methods for studying the kidneys and urinary tract.
The main radiological methods include survey and excretory urography. Survey urography allows you to determine the position and size of the kidneys, the presence of stones in the kidneys, urinary tract and bladder. Excretory urography is indicated for patients with sufficient nitrogen excretion function of the kidneys in order to determine the anatomical and functional state of the kidneys, renal pelvis and bladder. To carry it out, iodine-containing X-ray contrast agents (urografin, urotrast, etc.) are used, which are administered intravenously. The first x-ray is taken at 1 minute, the next x-rays are taken at 5, 10, 15, 20, 30, 45 and 60 minutes after administration of the contrast agent. This method allows you to determine the shape, size, position of the kidneys, their calyces, pelvis, ureters and bladder, as well as judge the excretory function of the kidneys.
scan is performed using neohydrin labeled with radioactive mercury Hg203. Using this method, you can obtain information about the contours of the kidneys, their size, shape, and also determine non-functioning areas of the parenchyma.
One of the most informative methods is ultrasound echography.
Ultrasound of the kidneys clearly determines their size, position, relationship between the parenchyma and the pyelocaliceal system; the vessels of the kidney and ureters are less scanned. Ultrasound of the kidneys allows us to exclude tumors, cystic formations, stones, kidney abscesses, pyo- and hydronephrosis.
In the diagnosis of many kidney diseases, an important role is played by puncture biopsy of the kidneys and histomorphological examination of the punctate. Indications for puncture biopsy are the need to clarify the diagnosis for diffuse and focal kidney diseases, as well as in order to select and prescribe more rational therapy. The biopsy is carried out with special needles and can be performed by one of three methods: 1) closed (percutaneous) biopsy
– in this case, the needle is inserted into the kidney tissue through a small puncture of the skin, which is made with a lancet;
2) with biopsy using the semi-open method
after making an incision in the skin and subcutaneous tissue 2–2.5 cm long below and along the XII rib from the edge of the long muscle of the back, push the muscles apart with a finger until the pole of the kidney can be felt. Then, under the control of a finger, the kidney punctate is taken;
3) with an open method
The kidney is surgically exposed and a piece of renal tissue is taken with a puncture needle for histomorphological examination.
Cystoscopy is an endoscopic method. A special device, a cystoscope, is inserted into the bladder through the urethra and then the wall of the bladder and the orifices of the ureters are examined through an optical eyepiece when the bladder is full.
Radioisotope renography (RRG) is the most common research technique that allows one to assess the degree of blood supply to the kidneys, the functional activity of the proximal tubules for the transport of isotopes, and the state of the renal collecting system. To conduct the study, hippuran is used, labeled with iodine isotopes (131 I and 125 I), which selectively accumulates and is excreted mainly by the kidneys. The process of entry of the isotope into the urinary tract and its removal from the body, reflecting the functional state of the kidneys as a whole, is manifested by a change in the intensity of y-radiation in the lumbar region. This radiation is captured by detectors located in the projection area of the kidneys. In them, y-radiation is converted into electrical impulses, which are recorded on the recorder in the form of curves - renograms. To determine the rate of purification of the blood from the isotope (blood clearance), the third detector is fixed above the heart area of the subject. Isotope renography is performed for persons with pathological changes in the urine, with an increase in the level of nitrogenous waste in the blood, for patients with a significant increase in blood pressure, and for persistent pain in the lumbar region. The subject is seated vertically in a chair. The sensors are installed perpendicular to the surface of the patient’s back above the projection of the kidneys. The third sensor (blood clearance) is attached above the precordial region. After that, hippuran, labeled with iodine isotopes, adjusted for the weight of the test subject, is administered intravenously. The study in most cases lasts 18-20 minutes. The patient is informed about the need to empty the bladder as soon as possible after the procedure.
The radioisotope renogram includes three curves (Fig. 1), reflecting the dynamics of y-radiation over the kidneys and heart (blood clearance). Each curve above the kidneys consists of three segments: vascular (A), secretory (B) and excretory (C).
The first segment corresponds to the entry of the isotope into the vascular bed of the kidney and reflects its vascularization. The recording duration of this segment should be no more than 40-50 seconds. The second segment of the renogram is slower; the rise of the curve is recorded within 3-5 minutes and reflects the accumulation of the isotope by the cells of the proximal tubules. After reaching the maximum accumulation, the transport of hippuran into the lumen of the renal tubules begins, which corresponds to a decrease in the activity of y-radiation over the kidney and the beginning of the third segment of the renogram. After 15-20 minutes from the start of the study, this curve becomes a plateau, indicating the absence of y-radiation in the kidney area and the need to stop recording.
The clearance value characterizes the total cleansing function of the kidneys. The clearance curve looks like two segments: 1 - a steep line, the peak of which is reached 2-5 s after the isotope enters the bloodstream, and 2 - a gentle decline, the speed of which depends on kidney function.
In clinical practice, it is customary to evaluate three indicators: T max - time of maximum rise of the renogram (normally up to 5 minutes);
T '/2 excretion - half-life (normally 8-10 minutes);
T '/2 clearance - the period of half-purification of the blood (normally 5-7 minutes, or 50%, Winter indicator).
Rice. 1. Radioisotope renogram is normal.
There are three main types of pathological renograms found in various diseases of the kidneys and other organs: obstructive, parenchymal and dysfunctional. Depending on the type and phase of the pathological process, a number of transitional types of radioisotope renograms can be observed.
Obstructive curve type
noted when the outflow of urine from the kidney completely stops, it is characterized by a normal or slightly reduced vascular segment, turning into an ever-increasing secretory segment. The excretory segment is missing. The height of the vascular segment depends on the blood circulation in the kidney, and the steepness of the secretory segment depends on the degree of obstruction of the urinary tract and on the functional state of the kidneys. This type of renogram is observed in cases of acute blockage of the ureter with a stone, its spasm or compression by a nearby tumor or inflammatory infiltrate (in such cases, the obstructive curve is fixed over two kidneys).
In case of partial disruption of the passage of urine from the kidney due to urolithiasis, inflammatory, degenerative and sclerotic processes in the parenchyma, in which the epithelial cells of the proximal tubules suffer, a recording curve of the parenchymal type of renogram is obtained.
It is characterized by varying degrees of decrease in the vascular segment associated with the death of functioning nephrons. The secretory segment is elongated, and the excretory segment is flatter. The reduction in the vascular and secretory segments is due to impaired renal circulation, intersticial edema of the parenchyma and its replacement with fibrous tissue. Lengthening of the excretory segment in such cases is caused not so much by obstruction of the tubules, collecting ducts and larger collectors by inflammatory and dystrophic detritus, deflated renal epithelial cells, but by a decrease in the amount of urine and impaired isotope transport by the cells of the proximal tubules.
Chronic kidney diseases in advanced stages (chronic glomerulonephritis, chronic pyelonephritis, nephroangiosclerosis with arterial hypertension, diabetes mellitus) lead to symmetrical changes in the parenchymal type renogram.
In urological diseases that are unilateral or bilateral (but with predominant damage to one of the kidneys), the isotope renogram shows asymmetric curves reflecting the degree of kidney damage.
Afunctional type of curve
Renograms indicate a lack of function of the epithelium of the proximal tubules due to their total replacement with sclerotic tissue. The renogram of such a kidney is represented by a low vascular segment and a straight line without distinguishing the secretory and excretory segments. Such a renogram can be obtained on the side of congenital or iatrogenic (nephrectomy) absence of a kidney, with complete occlusion of the renal artery by an atherosclerotic plaque, congenital hypoplasia of the kidney with the absence of parenchymal elements, and with other renal anomalies.
Bilateral afunctional curves are characteristic of the final stage of kidney disease of any etiology with the outcome in nephrosclerosis, manifested by chronic renal failure.
Rice. 2. Types of radioisotope renogram curve:
a – obstructive; b – parenchymal.
Questions for self-control of knowledge.
Test control tasks.
1. The appearance of a patient with nephrotic syndrome is characterized by: 1) skin color “coffee with milk”; 2) bronze skin tone; 3) cyanosis of lips, earlobes, fingers; 4) severe swelling of the face; 5) severe swelling of the lower extremities.
2. The appearance of urine the color of “meat slop” is characteristic of: 1) microhematuria; 2) gross hematuria; 3) cylindruria; 4) leukocyturia; 5) stranguria.
3. The patient’s presence of acute unilateral pain in the lumbar region with irradiation to the groin area after a shaking ride is characteristic of: 1) paranephritis; 2) acute pyelonephritis; 3) acute glomerulonephritis; 4) urolithiasis; 5) chronic glomerulonephritis.
4. Aching, dull, bilateral pain in the lumbar region is characteristic of: 1) renal infarction; 2) kidney prolapse; 3) urolithiasis; 4) kinking of the ureter; 5) acute glomerulonephritis.
5. In patients with paranephritis, a forced position is observed: 1) on the sore side with the leg bent to the stomach; 2) sits with legs down; 3) stands, leaning his hands on the back of a chair (bed); 4) on the side with the head thrown back and legs bent at the knee joints brought to the stomach; 5) tossing around in bed.
6. Prerenal oliguria is observed in all conditions except: 1) esophageal stenosis; 2) uncontrollable vomiting; 3) glomerulonephritis; 4) decrease in blood pressure during collapse; 5) burn of the oral cavity.