If there is a suspicion of the occurrence of oncological processes in the genitourinary system, a bladder tumor marker is performed. Such an analysis makes it possible to confirm or refute the development of a malignant formation with a high degree of probability. However, increased amounts of cancer antigen in the blood or urine may be the result of invasive intervention or the development of an inflammatory process in the urinary tract.
A bladder tumor marker test is required if you suspect the presence of a cancerous tumor in the organ.
What are tumor markers
Tumor markers are biological substances of protein origin that are detected in tests in the event of the development of cancer.
This diagnostic method makes it possible to detect the presence of a malignant neoplasm at the very beginning of its growth, which significantly increases the effectiveness of subsequent treatment.
The results of tumor marker tests help doctors determine the cause of a patient’s poor health, but they are not an absolutely accurate indicator of the presence of a malignant tumor.
Neoplasms in the organs of the urinary system are diagnosed only after a comprehensive examination: numerous laboratory tests, biopsy, ultrasound.
Why does adrenal tumor appear?
Before talking about the possible causes of cancer, it is necessary to tell what the adrenal glands are and what role they play in the human body.
These are paired endocrine glandular organs, the main task of which is the production of steroid hormones: aldosterone, corticosterone, cortisol, androgen, adrenaline and deoxycorticosterone.
All of them maintain the condition of blood vessels, help adapt to stressful situations, are responsible for metabolic processes, control the distribution of proteins, fats, carbohydrates and water-salt balance.
The adrenal glands are susceptible to various pathologies, one of which is cancer. Why does malignancy occur? As in most cases of cancer, it has not yet been possible to find out the exact cause of the disease.
There are two sets of genes in the human body. The first of them affects the development of cancer cells, the second, on the contrary, suppresses this process. Any disturbances that lead to imbalance contribute to the development of cancer.
Also, over time, some cells undergo changes and mutate into pathogenic ones. This is mainly due to the living conditions and lifestyle of a person.
To a lesser extent, genetic predisposition. Another reason for the appearance of a tumor is heredity, with factors contributing to the development of cancer.
Secondary reasons include:
- bad habits;
- unhealthy diet, which is dominated by animal fats;
- sedentary lifestyle;
- constant increase in blood pressure;
- injury;
- congenital changes in the system of regulation of the functions of internal organs with the help of hormones;
- working or living in an environmentally unstable area;
- frequent stress;
- the presence of an already congenital syndrome, which gives impetus to the development of a new formation;
- age either before 5 years or after 40 years.
Frequent stress can cause adrenal cancer.
The disease can also appear due to regular and uncontrolled use of medications. Benign cancer of the adrenal cortex is much more common, but if it is not detected and treated in time, then in half of the cases the process develops into malignant.
Types of tumor markers of the kidneys and bladder
Bladder cancer has become increasingly common in recent years. Of all cases of cancer, this type is diagnosed in 5% of patients and in every 2nd man with nicotine addiction.
Tumor markers are detected using a blood test or urine test. Exceeding the normal content of tumor markers in biomaterial samples indicates tumor growth.
It is recommended to undergo such a study if there is any suspicion of a malignant neoplasm.
Tumor markers for bladder cancer:
- UBC is by far the most informative marker. The only promising indicator that always detects a tumor at the earliest stage. According to statistics, an increased concentration of UBC in the urine indicates cancer in 70% of patients.
- NMP22 is a specific protein secreted by tumors. Helps evaluate the effectiveness of antitumor therapy.
- TPS is a tumor marker, the presence of which helps to identify cancer not only of the bladder, but also of the gastrointestinal tract and reproductive system. The concentration of this protein in the biomaterial increases sharply in the presence of metastasis. Exceeding TSP standards after chemotherapy should alert the attending physician, as this indicates the futility of the treatment received.
In a comprehensive diagnosis of bladder cancer, the following markers are also looked at: VTA, fibrinogen, nuclear matrix protein, cytokeratin products.
The presence of these proteins in low concentrations in the blood or urine can indicate not only cancer, but also any other pathological process.
These substances are produced by the body in a healthy state, but their synthesis is activated in the presence of serious pathologies, including cancer, so a high concentration may indicate the appearance of atypical cells in the body.
Kidney tumor markers for cancer detection:
- HCG is a hormone whose name is familiar to everyone; doctors use it to detect pregnancy in women. After fertilization, it begins to be actively produced, blocking the functioning of the reproductive system and thereby eliminating the possibility of getting pregnant again. Under normal conditions, hCG is practically not produced in both women and men. But exceeding this indicator in the absence of pregnancy may indicate the development of a malignant kidney tumor.
- TU-M2 – PK (pyruvate kinase) – based on the concentration of this substance, doctors draw conclusions about the degree of aggressiveness of the tumor.
- NSE - elevated levels of this enzyme may indicate kidney and lung cancer.
There is another type of kidney cancer marker. It is designated as HCE. If the values are exceeded several times, the doctor must prescribe additional tests to identify cancer cells.
Oncologists say that at the moment there are no specific markers that detect only kidney cancer.
All of the above indicators may indicate the presence of cancer, or may indicate the presence of other pathological conditions.
Therefore, to confirm test results, it is important to conduct a comprehensive examination, including tissue biopsy when a tumor is detected.
Tumor-M2-pyruvate kinase (Tu M2-PK)
The tumor marker Tu M2-PK shows how aggressive the malignant tumor is. It is necessary to ensure the cellular metabolism of the neoplasm. One of the metabolic pathways in cells, glycolysis, is that without access to oxygen, a glucose molecule breaks down into two molecules of pyruvate under the influence of the enzyme pyruvate kinase.
In tumor cells, the role of pyruvate kinase is played by Tu M2-PK, one of its forms. Intermediate products of reactions involving Tu M2-PK have high energy intensity and provide active growth in the number of cancer cells.
Since Tu M2-PK is a metabolic and not a cumulative tumor marker, unlike others, it is one of the first to enter the bloodstream. In addition to blood serum, it is also detected in feces. M2-PK is a reliable indicator of the appearance of malignant tumors and can detect them in more than 80% of cases.
On this topic
What affects the prognosis for liver cancer
High levels of Tu M2-PK may also indicate cancer of the intestine, esophagus, breast, lungs, pancreas, and bile duct. This tumor marker is most often used to detect intestinal tumors. In addition to detecting cancer and precancerous conditions, determining Tu M2-PK levels allows monitoring the effectiveness of treatment and determining the presence of metastases.
- When will an hCG test show pregnancy? Concentration of hCG in urine by day after ovulation
Normally, the concentration of Tu M2-PK in blood plasma is up to 15 units/ml. A reading of 15-20 units/ml represents a gray area. Studies show that after removal of the affected kidney, Tu M2-PK returns to normal within three months or less.
Indications for prescribing tests for tumor markers
Tumor markers for kidney cancer are not just given as part of preventive examinations.
The following reasons must exist to prescribe such tests:
- a history of cancer in the patient’s relatives;
- carrying out chemotherapy for an already identified tumor, tests are taken after each course;
- sudden weight loss, chronic fatigue;
- increased body temperature in the absence of cold symptoms;
- presence of bad habits;
- diseases that are considered a precancerous condition;
- work in hazardous production;
- enlargement of lymph nodes characteristic of cancer.
It is impossible to make an accurate diagnosis based solely on the results of tumor marker tests. This can only be done after a series of related studies.
What tumor markers should a woman take?
For the prevention and detection of diseases, only specific indicators are used that can make it possible to identify oncology. You need to know that all tumor markers are extremely sensitive to any inflammatory processes. Therefore, if at least one source of infection is present in the body, tests can show the presence of cancer cells. For the result to be correct, it is initially necessary to undergo an inpatient examination and completely exclude chronic ailments.
Main tumor markers:
- “CA-15–3 and MSA” are intended to detect malignant tumors in the breast. Also, using these indicators, the absence or presence of metastases is determined.
- Decoding the tumor marker “CA-125” shows the presence or absence of ovarian cancer. Also, this protein structure occurs in increased quantities during pregnancy. Therefore, if “CA-125” is positive, then additional examinations are carried out.
- “CA-72–4” - this type is used in cases where there is a suspicion of ovarian cancer, when you need to be completely sure that the treatment is being carried out correctly, and also to confirm the gradual destruction of malignant cells.
- HCG in women helps diagnose uterine cancer. Thanks to the test, pathological abnormalities can be identified at an early stage. In addition, such an analysis is used to re-diagnose the disease in uterine tissue after surgery.
Contraindications
There are no special contraindications for testing for tumor markers; we can only highlight the following conditions in which it is necessary to postpone a visit to the laboratory:
- days preceding menstruation (PMS), since during this period tests may give false results due to changes in hormonal levels;
- infectious diseases;
- ARVI;
- the presence of pathologies in the genitourinary system.
In each specific case, the decision is made by the doctor. There are situations in which you cannot delay the examination and postpone tests until a later time.
Indications and contraindications for the study
A thorough examination of the genitourinary system and a test for tumor markers of the bladder should be performed if the following symptoms appear:
- the appearance of blood in the urine (hematuria) - occurs in every 9th cancer patient;
- urination disorders - frequent urge, the patient experiences pain during the process, a small volume of urine per act;
- regular urinary tract infection;
- lower back pain;
- swelling of the legs.
The reliability of the results is influenced by many factors. Therefore, the study should be postponed if:
- the patient has an acute inflammatory or infectious disease of the urinary tract;
- Less than 2 weeks have passed since invasive intervention in the urinary system.
Preparation for the procedure
Basic rules for preparing for the submission of biomaterial to detect cancer markers:
- 72 hours before the test, you must avoid drinking alcoholic beverages;
- abstain from smoking, sexual activity and physical labor;
- women should not submit material for analysis on the days of menstruation;
- exclude smoked meats and marinades from the menu, reduce salt consumption;
- stop taking anticoagulants and other medications; in some cases, with the permission of the doctor, you can continue to take medications before donating blood.
For reliability, it is important to perform a laboratory test on the day of blood collection, but some laboratories freeze the blood and test it later.
With this approach, false results may appear, so the analysis is repeated several times to confirm the diagnosis.
Tumor markers help the doctor determine the direction of further examination; they are used to monitor the effectiveness of the chosen treatment. Even after the patient is completely cured, he will need to be tested for tumor markers 1-2 times a year for control.
Taking medications that regulate the functioning of the circulatory, cardiac and genitourinary systems can distort the results of studies. If necessary, the doctor will insist on stopping medications during the examination.
It is not recommended to take such tests on your own, without a doctor’s referral, since tumor markers are not accurate indicators of the presence of the disease; other examinations will then be required to confirm suspicions.
Urine for tumor markers is collected in a jar immediately after waking up and should be examined as quickly as possible.
Stages of disease development
In medicine, there are four stages of adrenal cancer, each of which has its own characteristics:
- at the first stage, the size of the formation does not exceed 5 cm, while the lymph nodes are not enlarged, there are no metastases;
- at the second stage, the size of the formation increases to more than 5 cm, but there is no metastasis;
- moving into the third stage, the tumor increases so much that it leaves the boundaries of the organ and affects nearby tissues, the lymph nodes enlarge;
- at the fourth stage, active metastasis of cancer occurs to other organs: kidneys, liver, lungs.
In the first two stages, it is very difficult to diagnose the disease, which negatively affects the correct diagnosis.
In addition to stages, adrenal tumors are divided into types:
- pheochromocytoma is a hormonal growth that occurs in the adrenal medulla. A feature of the formation is the active production of hormones;
- neuroblastoma is a pathological neoplasm that affects every immature cell of the sympathetic nervous systems.
Also, formations can form in the cortical or medulla layer of the adrenal glands, be primary or secondary.
The adrenal cortex and medulla are of different origins. The cortex differentiates from the mesoderm (from the coelomic epithelium) between the root of the dorsal mesentery of the primitive intestine and the urogenital fold.
The tissue developing from mesodermal cells and located between the two primary buds is called interrenal tissue. It gives rise to the adrenal cortex, from which accessory adrenal glands (interrenal bodies, glandulae suprarenales accessoriae) are formed.
The adrenal medulla develops from embryonic nerve cells - sympathoblasts, which are evicted from the anlage of the nodes of the sympathetic trunk and turn into chromaffinoblasts, and the latter into chromaffin cells of the medulla.
Chromaffinoblasts also serve as material for the formation of paraganglia, which in the form of small clusters of chromaffin cells are located near the abdominal aorta - aortic paraganglia (paraganglion aorticum), as well as in the thickness of the nodes of the sympathetic trunk - sympathetic paraganglia (paraganglia sympathica).
The introduction of future medulla cells into the interrenal adrenal gland begins in the 16 mm long embryo. Simultaneously with the unification of the interrenal and adrenal parts, differentiation of the cortical zones and maturation of the medulla occur.
[20], [21], [22], [23], [24], [25], [26], [27], [28], [29]
Carrying out the procedure
Venous blood is donated only in the morning, on an empty stomach. Testing for tumor markers is carried out differently from conventional studies. Blood from a vein is drawn into a syringe, not into a test tube.
Urine for cancer testing is provided in a special sterile container.
Analysis results are usually ready within 2-3 days.
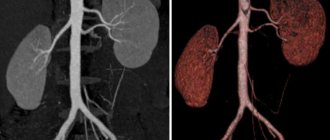
If the tests reveal the presence of cancer markers, the patient is prescribed further diagnostics:
- Ultrasound;
- MRI with contrast;
- MSCT.
Tissue from the kidney or bladder is taken for examination only if a tumor is detected.
Kinds
Markers differ for different reasons. For example, the main one has high sensitivity and specificity. Secondary species are studied simultaneously with the main ones.
Additional tumor markers are usually specific to a particular organ and are used to determine relapses.
Based on its origin, such a substance is divided into:
- oncofetal,
- enzymes,
- hormones,
- receptors.
Most cancer indicators are type 1. These structures are found in high concentrations in the tissues of the embryo, where they appear in dividing cells.
The second most important are enzymes. They are divided into those in which the biological function has been elucidated and those where it has not been established.
| Localization | Tumor marker |
| Mammary gland | CA15-3, CEA |
| Testicles | B.H.C.G., A.F.P. |
| Ovaries | CA125, CA 19-9 |
| Uterus | CA 19-9, CA 125 |
| Intestines | CA 19-9, CA 125 |
| Pancreas | CA 19-9, CA 72-4 |
| Liver | AFP |
| Leather | S 100 |
| Bladder | TPA, Cyfra 21-1 |
| Prostate | P.S.A. |
Some indicators may be increased, but it is difficult to determine the exact localization from them. For example, CEA, produced in the tissues of the embryo. In adults, it is produced in small quantities and is sensitive to most tumors.
Results and their interpretation
Depending on the analysis method, reference values of tumor markers may change. Usually the range of normal levels of substances in the blood is indicated next to it, on the same line with the result.
A complete interpretation of the tests to make an accurate diagnosis should be carried out on the basis of comprehensive studies.
Tumor marker values for kidney cancer:
- Normal hCG values for adults:
- Non-pregnant women of reproductive age – from 0 to 1 IU/ml;
- Non-pregnant women in menopause – from 0 to 7 IU/ml;
- Men – from 0 to 2 IU/ml.
- Normal values for the NSE tumor marker in the blood are from 0 to 16.3 ng/ml;
- Normal values for TU-M2 (pyruvate kinase): 0 to 15 U/ml. A very large amount of this tumor marker indicates a high degree of aggressiveness of atypical tumor cells.
Exceeding normal values (for each laboratory they are expressed in their own units of measurement) may indicate the presence of a malignant tumor in the kidneys or other organs. There are no special markers that specifically detect kidney cancer.
Tumor markers for bladder cancer:
- Normal UBC values in urine range from 0 to 15 ng/ml.
- The normal level of NMP22 in urine is from 0 to 10 U/ml.
- For the tumor marker TPS in the blood, reference values are considered to be from 0 to 85 U/l.
If a tumor is detected in the bladder or kidneys, the patient is prescribed a biopsy of the affected tissue to determine the nature of the tumor.
It is important not to forget that even in the presence of cancer, marker tests may be normal.
Tumor markers UBC, NMP22, TPS - interpretation, norms
Tumor markers UBC, NMP22, TPS are determined in urine using an enzyme-linked immunosorbent assay (ELISA).
Reference values of tumor markers (norms) may differ slightly in different laboratories, which is due to the sensitivity of the equipment used.
The normal level of the UBC tumor marker in urine is up to 33 mcg/liter (with highly sensitive equipment, reference values can be determined up to 12 mcg/liter). A multiple excess of this indicator may indicate the presence of bladder cancer.
The normal level of the tumor marker TPS in the blood serum is up to 85 U/l. An excess of this tumor marker is determined in epithelial cell cancer, in particular in bladder cancer. Also, an increase in this tumor marker can be detected in other malignant neoplasms: breast, ovarian, prostate, and stomach cancer.
The normal value of the tumor marker NMP22 in urine is up to 10 U/ml. Exceeding this indicator may also indicate bladder cancer.
Additional Information
It is very important to know that urine testing for the UBC tumor marker is not screening - it only indicates the need for cystoscopy to clarify the diagnosis. Instead of performing a cystoscopy on a patient every time, the doctor prescribes this test for the patient, and based on its results he judges whether the patient needs a cystoscopy or not. This is especially true for patients who have already been diagnosed with bladder cancer and have been prescribed treatment. Carrying out cystoscopy too often is fraught with complications, and the UBC test allows you to eliminate unnecessary procedures.
The introduction of minimally invasive diagnostic procedures into oncological practice greatly facilitates the doctor’s work in terms of diagnosing malignant diseases. For the patient, such methods are also very convenient - they allow you to obtain maximum information with minimal inconvenience for him. However, one should not exaggerate the importance of this diagnostic method - the final diagnosis is made only on the basis of cystoureteroscopy and tumor biopsy.
Literature:
Surgical treatment of adrenocortical cancer
Adrenal hyperfunction is a pathology of the adrenal glands, characterized by excessive secretion of adrenal hormones. It is divided into several types:
- hypercortisolism (Itsenko-Cushing syndrome)
- corticogenital syndrome (excess sex hormones)
- hyperaldosteronism (increased aldosterone production)
- overproduction of catecholamines (pheochromacytoma)
- mixed hyperfunction (there is an increase in the production of several adrenal hormones)
Let's consider each type separately.
Itsenko-Cushing syndrome is the so-called primary hypercortisolism and is associated with damage to the adrenal cortex. Women are 4-8 times more susceptible to the disease; the age range is from 20 to 45 years. The causes of this condition may be:
- Tumor (benign or malignant) - most often arises from cells of the zona fasciculata and is called glucosteroma (synthesizes glucocorticoids).
- Various types of adrenal hyperplasia (nodular, primary bilateral hyperplasia, diffuse, nodular)
- Hormonal disbalance
The mechanism of development of this condition comes down to the secretion of high levels of cortisol. Cortisol, in turn, inhibits the release of ACTH by the pituitary gland. Let us remember that ACTH affects the breakdown of fats, weight, the formation of a person according to gender and, of course, the secretion of sex hormones.
Now it is easy to understand the mechanism of formation of the clinic of primary hypercortisolism syndrome. The symptoms are as follows:
- Cushingoid obesity: deposition of adipose tissue on the face, upper half of the torso, above the collarbones, “buffalo hump” (deposition of fat in the lower back of the neck)
- muscle atrophy of the lower extremities
- severe headaches
- arterial hypertension
- osteoporosis: patients complain of pain in the joints and bones, the person is like glass, fractures can occur, as they say, out of the blue
- the skin becomes thinner, becomes dry, and purplish-red stretch marks appear on the body
- psycho-emotional disorders (irritability, aggression, tearfulness, prolonged depression, even suicide attempts)
- Steroid-induced diabetes or impaired glucose tolerance often develops
- sexual dysfunction (menstrual irregularities, infertility)
- pustular skin diseases, acne
Surgical treatment was, is, and probably will continue to be the most effective method for a long time. The entire affected adrenal gland is removed. The main thing is not to damage the tumor capsule, because tumor cells can disperse, and their aggressiveness is very high.
They try to remove the enlarged lymph nodes closest to the tumor, which improves long-term survival results. With a large cancerous tumor growing into the kidney, the question of removing the kidney may arise.
We have not yet finally decided on the removal of the adrenal gland using endoscopic equipment - laparoscopic adrenalectomy. There have been insufficient studies due to the rarity of the tumor, and the results are contradictory.
In the meantime, it is recommended not to perform laparoscopic adrenalectomy for adrenal tumors larger than 5 cm and growing into surrounding tissues with metastases to the lymph nodes. In this matter, sufficient experience of the oncologist surgeon is very important.
In the postoperative period, they are involved in the prevention or treatment of insufficiency of the function of the remaining adrenal gland and, of course, the prevention of thrombosis.
You may have to take hormonal medications for life to compensate for the function of one lost and second atrophied adrenal gland. Replacement therapy is an inevitability that cannot be refused.
In case of relapse after surgical treatment, they try to perform resection as radical as possible. The degree of radicalism is reflected in the patient’s life expectancy.
If Ki 67 expression is detected in a tumor, then foreign oncologists have been conducting preventive chemotherapy with cloditan for more than 40 years. The drug is toxic, requires regular determination of blood concentration, its therapeutic effect depends on the administered dose.
Doctors at the European Clinic use the most modern drugs and cancer treatment regimens. We know how to help even in difficult cases. Consultations are held daily, appointments are available 24 hours a day.
Surgery for adrenal cancer is the only radical method that can, in some cases, completely cure the patient. Given the rapid metastasis of adrenal cancer, tumor removal should be performed as quickly as possible after its identification and assessment of hormonal activity.
When planning the operation, the following points should be taken into account.
Surgical treatment of patients with adrenal cancer should be performed in a specialized endocrine surgery center that performs a significant number of adrenal surgeries annually.
Diagnostics, preoperative preparation, surgical intervention - all these stages have a lot of “pitfalls”, knowledge of which is achieved only with increasing experience of doctors after several years of work in this field.
- high levels of blood cortisol and/or male sex hormones, which increases blood clotting;
— blood loss during surgery with the need for transfusion;
— separation of tumor blood clots in the veins of the abdominal cavity during surgery;
— illiterate preparation of the patient for surgery, insufficient prevention of the development of thrombosis.
The operation should be carried out with maximum preservation of the integrity of the tumor capsule. If the capsule is damaged, adrenal cancer recurs in 100% of cases.
The absence of tumor trauma is ensured by the experience of the surgeon performing the operation, as well as the use of modern equipment - ultrasonic harmonic scalpel, bipolar coagulator with feedback, etc.
The most important rule to ensure radical surgery is to remove the tumor within healthy tissue (the so-called R0 resection).
An important stage of surgery for adrenal cancer is prophylactic lymph node dissection - removal of retroperitoneal lymph nodes. Some scientific studies have shown that lymph nodes are affected in 20-30% of patients - this fact alone dictates the need for prophylactic removal of lymph nodes in all patients.
In some cases, with small tumor sizes, it is possible to perform endoscopic surgery to remove adrenal cancer, but the endoscopic method of surgical treatment for this tumor is not the main one.
Traditional open access surgery allows for the most complete examination of the abdominal cavity and retroperitoneal space, performing a thorough lymph node dissection, reducing the risk of damage to the tumor capsule and the associated spread of metastases throughout the peritoneum.
It should be borne in mind that the disadvantage of open surgery is its traumatic nature. In any case, any surgical intervention (open or endoscopic) should be planned only in a specialized center for endocrine surgery - this rule is not questioned.
In case of tumor recurrence, when the tumor center or its metastasis is surgically removed, one should be inclined to repeat surgery aimed at complete removal of the cancer, since scientific evidence suggests the advantages of this approach - patient survival increases.
— Petrograd branch (St. Petersburg, Kronverksky pr., 31, Gorkovskaya metro station, tel., from 7.30 to 20.00, seven days a week);
— Primorsky branch (St. Petersburg, Savushkina st., 124, building 1, Begovaya metro station, tel. (812) 344-0-344, from 7.00 to 20.00, seven days a week).
| Sleptsov Ilya Valerievich, endocrinologist surgeon, Doctor of Medical Sciences, professor of the Department of Surgery with a course in surgical endocrinology, member of the European Association of Endocrine Surgeons |
| Fedorov Elisey Aleksandrovich, Endocrinologist surgeon of the highest qualification category, Candidate of Medical Sciences, specialist at the North-Western Endocrinology Center. One of the most experienced surgeons in Russia performing operations on the adrenal glands. The operations are performed using a minimally traumatic retroperitoneoscopic approach through lumbar punctures, without incisions. |
Due to the need to quickly admit patients to the clinic for treatment, patients suspected of having adrenal cancer may be consulted out of turn.
If there are no places for a consultation, the clinic administrator has the opportunity to request the consultant for additional unscheduled appointment times for patients.
1, for children over one year old - saline solution containing 5% glucose. At the same time, a water-soluble hydrocortisone preparation is administered intravenously at a rate of 10-15 mg/kg body weight per day.
It should be remembered that excessive administration of drugs containing sodium, in combination with high doses of mineralocorticoids, can contribute to the development of cerebral and pulmonary edema, arterial hypertension with intracranial hemorrhages.
Insufficient administration of glucose against the background of high doses of glucocorticosteroids contributes to the development of metabolic acidosis.
Normal values of UBC antigen in urine
Normally, the concentration of UBC antigen in urine does not exceed 12 μg/l. Reference values may vary depending on the conditions under which the study was conducted, the reagents and equipment used. Therefore, the normal range should be determined using the results form issued by the laboratory. For the same reason, it is recommended to take the test again in order to determine the dynamics of the disease in the same laboratory. This will allow the doctor to correctly correlate the indicators, evaluate the effectiveness of therapy, and identify relapse.