Artificial kidney from the Swedish company Gambro
Artificial kidney
— a device for temporary replacement of the excretory function of the kidneys. An artificial kidney is used to free blood from metabolic products, correct electrolyte-water and acid-base balances in acute and chronic renal failure, as well as to remove dialysable toxic substances in case of poisoning and excess water in case of edema.
The main task of the artificial kidney apparatus is to cleanse the blood of various toxic substances, including metabolic products. At the same time, the volume of blood within the body remains constant.
Currently, work is also underway to create an artificial kidney using bioengineering methods.
Indications for hemodialysis
Dialysis is a procedure for artificially purifying the blood of harmful elements in case of impaired kidney function.
Today, its relevance has increased significantly. It should be understood that such a measure does not promote healing and does not help eliminate inflammatory processes, but only serves as a filter organ, relieving a person of toxic decay products. In ICD-10, dialysis is coded Z49. In modern medicine, several methods of blood purification are used. Peritoneal dialysis. A method based on the filtration ability of the peritoneum, the thin shell of which plays the role of a semi-permeable membrane. It is prescribed if the patient does not have the opportunity to undergo the procedure in a specialized center due to the absence of the latter, or if there are serious contraindications to standard manipulation. This blood purification can be done at home. The dialysis solution is poured directly into the abdominal cavity through a catheter.
Hemodialysis. The blood is purified using a special device - a hemodialyzer, which is connected to the vessels through a set of tubes, semi-permeable membranes involved in the filtration process.
| Types of dialysis | Periodicity | Advantage |
| Peritoneal | Every 6 hours | No risk of bleeding No strain on the heart |
| Hemodialysis | 3-4 times a week | Short procedure duration |
Advances in clinical medicine make it possible to carry out the procedure (regardless of its type) at home, providing maximum comfort to the patient.
The main purpose of the hemodialysis procedure is to filter the blood. With the help of special devices, the biological environment is cleansed from harmful substances:
- creatinine and urea;
- medicines, toxins and poisons;
- excess water, alcohol and electrolytes.
Today, the procedure can be performed mainly in a hospital, less often at home.
The essence of the procedure
Access to the natural hemodynamic environment is provided through an arteriovenous fistula; filtration is carried out in a multilayer osmotic membrane, which allows vital blood components to pass through and retains harmful waste compounds. The flow rate is controlled by a precision pumping station equipped with electronic gauge control.
First, venous blood is collected and fed into a filtration system with a semi-permeable membrane. It has pores of different diameters, separating the blood and the cleaning solution. Excess fluid and harmful substances pass into the dialysate. At the same time, special sensors monitor arterial and venous pressure.
The device provides for the supply of Heparin to the blood, which dissolves blood clots while simultaneously preventing the formation of new ones. It also has an anti-inflammatory effect and helps improve renal blood flow.
It is important to know! The frequency, intensity and duration of the procedure are prescribed on a strictly individual basis. 3-4 sessions per week are considered optimal.
Programmed hemodialysis of the kidneys, in which indications and contraindications depend on many factors, is not prescribed for any disorders of renal function, but only when there is no other way to cleanse the blood of toxins and poisons. The reason for carrying out this particular type of procedure is the data of urine and blood tests:
- urea in the blood reaches 35 mmol/l;
- plasma creatinine level is 1 mmol/l or higher;
- bicarbonate content – 20 mmol/l;
- the amount of potassium is more than 6 mmol/l;
- oliguria – daily urine volume does not exceed 450 ml;
- the kidney performs its functions no more than 11-16%;
- GFR does not exceed 200 ml/sec.
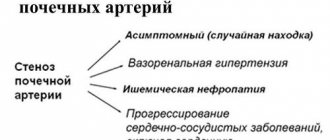
If hemodialysis is necessary, there are instructions in which cases it is performed. The doctor decides to connect the patient to the device if a number of the following pathologies are present:
- Acute renal failure - acute renal failure.
- Overdose of drugs: sleeping pills, sedatives, antibiotics, sulfonamides, antitumor drugs.
- Intoxication with poisons – toadstool, arsenic.
- Alcohol poisoning – ethylene glycol, methyl alcohol.
- Overhydration, leading to swelling of the heart, lungs, brain, joints.
- Electrolyte imbalance in case of dehydration, peritonitis, fever, intestinal obstruction, burns, cystic fibrosis.
- Poisoning with narcotic substances - heroin, morphine.
- Chronic renal failure and CKD.
But not every patient can undergo blood purification using hemodialysis. There are a number of clearly defined contraindications and restrictions.
- Diseases of infectious origin, which are more serious in terms of threat level than chronic renal failure.
- Pre-stroke condition, hemorrhage in the membranes of the brain, as well as the early period after it.
- Psycho-emotional imbalance, severe mental disorders - schizophrenia, psychopathy, epilepsy, MDP.
- Mental retardation, dementia, reduced intelligence.
- Hyperbilirubinemia.
- Arterial hypertension, which can lead to a stroke right during the procedure.
- Blood diseases - leukemia, aplastic anemia. The likelihood of cell destruction and bleeding increases.
- Malignant tumor processes. The risk of cancer cells spreading through the bloodstream increases.
It is important to know! Another reason prohibiting the use of hemodialysis is physiological transformations in the body due to the patient’s age of 85 years and older. If you have diabetes, this threshold is reduced to 70 years.
Blood purification is performed using a special device called an “artificial kidney.” The design of the device may be different, but the principle of operation remains the same - removal of harmful substances by diffusion and convection. The kit includes the following items:
- a system that supplies blood and regulates its progress during purification;
- a dialyzer in which a double-sided filter is located;
- container for cleaning solution;
- a screen on which the entire process is displayed and controlled.
The operating principle of the device is quite simple. Blood from the vein enters the device through special tubes. The device is simultaneously supplied with a solution that passes through the filter on one side and blood on the other. The biological fluid is returned back to the vascular system, and the spent composition with toxic waste is removed.
To prepare a patient for chronic hemodialysis, it is necessary to form an arteriovenous fistula - an opening that provides free access to the vessels through which the required amount of blood can be infused and removed. It is created through surgery on the wrist or elbow. The procedure takes place in several stages.
- Local anesthesia is performed (less commonly, general anesthesia).
- The area is treated with antiseptic agents.
- Using an incision, the artery is exposed, a ligation is made, and then excision is performed.
- A lateral vein is brought out and clamps are applied to it.
- Both types of vessels are dissected, after which they are sutured together.
- The wound is sutured and a sterile dressing is applied to the area.
Installation of a fistula takes less than an hour, and if the manipulation is performed correctly, the operated area heals quickly.
Hemodialysis is carried out in specialized centers or departments where there is an artificial kidney apparatus. Currently, the BAXTER-1550, FREZENIUS 4008S, NIPRO AURDIAL, and Fresenius installations are used. Patients are delivered by ambulance, transferred from other hospitals, or come independently for a planned procedure according to an individual program.
The procedure is considered relatively expensive. Those wishing to undergo chronic hemodialysis should be aware that the cost varies in different clinics and countries. The total amount is made up of several factors:
- patient's severity;
- presence of concomitant diseases;
- level of respectability of the medical institution.
In private clinics, the expense item includes:
- care services provided by staff;
- payment for the ward;
- additional expenses.
The amount indicated in the price list is paid in a lump sum upon admission to the medical center at the time of conclusion of the contract. It must match the one named by the doctor providing the consultation.
| Country where hemodialysis is performed | Total cost of the procedure and stay in the clinic |
| Russia | Moscow – 97,650 rubles; St. Petersburg – from 14,500 rubles; Rostov-on-Don – from 13,000 rubles. |
| Israel | “Assuta”, “Hadassah” - from 300 dollars. |
| Germany | – from 200 euros. |
| USA | New York - 250-300 dollars. |
But situations often arise when the procedure can be performed free of charge. Only in this case we are not talking about treatment abroad or private clinics. Patients in critical condition undergo urgent hemodiafiltration.
In various countries, annually 60-100 patients per 1 million population require renal replacement therapy (RRT) due to the development of end-stage chronic failure of the filtering organ. Until recently, this sounded like a death sentence. Today medicine offers three main methods of maintaining the lives of people with this diagnosis.
It is important to know! Despite constantly improving medical technology, chronic hemodialysis has many negative side effects and circumstances that worsen the patient’s well-being. Therefore, it can be considered as an intermediate therapy.
Patients with a transplanted organ (if rejection does not occur) can live as before, and their quality of life is much higher. Despite the fact that from an economic point of view this method is considered unprofitable due to its high cost, it is an option of choice for end-stage chronic renal failure.
Blood filtration using a device is prescribed in the following cases:
- acute or chronic renal failure;
- pyelonephritis;
- acute glomerulonephritis;
- diabetes;
- swelling of the lung or brain;
However, not only kidney disease and impaired excretory function can cause hemodialysis. Manipulation is necessary in case of poisoning with toxins.
Implantable artificial kidney: an overview of the current state of technology
Kidney transplantation is the preferred treatment for chronic kidney disease, but the shortage of kidney transplants, the increasing number of patients with chronic kidney disease, and the rapid progression of the disease make most patients dependent on dialysis.
Because dialysis dramatically impacts patients' lifestyles, great hope is placed on the development of artificial kidneys, although their use is currently hampered by serious safety concerns.
On the other hand, patients with hemodynamic instability generally do not tolerate intermittent dialysis treatment due to their inability to adapt to a changing scenario of unexpected events.
The artificial kidney is expected to provide patients with chronic kidney disease with a new option beyond the short-term solution of kidney dialysis and expensive kidney transplants. Today, developments in this area are being carried out both with the goal of creating wearable devices and an implantable version of the artificial kidney.
In this review, we discuss recent advances in the development of implantable artificial kidneys.
The implantable artificial kidney, which is being developed by several teams of scientists today, is similar to the existing extracorporeal kidney care device, which is a biologically artificial kidney that combines a membrane hemofilter and a bioreactor to function as a healthy kidney.
However, such a device must be small, have high efficiency filtration membranes, and must be able to regulate blood flow and stabilize the necessary components. An implantable artificial kidney should be able to replicate the function of a real kidney, eliminate the need for dialysis, and not require constant medical supervision.
In addition, its use should not require the use of immunosuppressants and medications.
This is ideal, but what do we have in reality today?
Kidney Project (University of California, San Francisco)
The most famous development in this area is carried out within the framework of the Kidney Project, which employs specialists from the University of California, San Francisco and Vanderbilt University (USA).
They have developed an implant the size of a coffee cup that can perform the functions of a kidney and is a great solution for patients with chronic kidney disease.
This small, surgically implanted device consists of a highly permeable filtration block and human kidney cells.
The filter component has micropores that can be individually shaped to perform specific tasks. These filters can be placed one after the other, each of which will perform a different filtering function. In total, the device contains fifteen such filters, placed one on top of the other.
In between and around these filters are living kidney cells that perform functions that artificial components do not do well, including reabsorbing nutrients and getting rid of accumulated waste.
Since such a hybrid biological device would be placed out of reach of the body's immune response, it would thus be protected from rejection by the human body.
Those. The device contains living cells and could theoretically not only filter blood, but also perform other important functions of a real kidney, such as releasing hormones to control blood pressure.
In addition to filters that separate various substances in the blood, the implant includes a “bioreactor” that processes the ultrafiltrate, extracts sugar and salts from it, which it returns to the blood.
In this process, water is also reabsorbed back into the body, and the ultrafiltrate is converted into “urine”, which is sent to the bladder for removal from the body.
These devices are housed in a durable housing, covered with a film of material that is safe for use inside our body. The implant is connected by tubes to nearby veins and the bladder.
The device is powered by the patient's blood pressure and does not require the use of external tubing or cables that are now associated with wearable artificial kidneys.
Purified blood is returned to the circulatory system through veins connected to the implant, and waste is transferred to the bladder through a corresponding tube. All elements through which blood passes are coated, which should prevent the formation of blood clots. In addition, the formation of blood clots is prevented by a specially designed blood flow pattern within the system.
According to the developers, the device will not perform all the functions of a human kidney.
“But the goal is for it to perform critical functions and be a system that, once implanted, allows the patient to eat and drink freely, have mobility, better overall health, and, unlike a transplant, not require the use of immunosuppressants,” say university scientists.
Note that patients must still take the hormonal supplements they use during dialysis procedures.
Testing of a working prototype is expected to take place in 2020.
USKRC
American Kidney Research Corporation (USKRC) recently announced the development of what they claim is the “world's first” implantable artificial kidney.
This device uses a method to produce synthetic urine using deionization blood purification technology, which is the first of its kind.
It involves filtration and ion transport processes that are similar to those occurring in the human kidney.
The development, which is funded by the USKRC, is led by scientists from the University of California, Los Angeles and the University of Arkansas.
According to the system developers,
There are various ions and substances in the blood, including sodium, potassium, urea and water, that need to be transported, either into the blood or into the urinary stream, and in appropriate amounts over a period of time. To do this, it is necessary to create an ion transport system and a water transport system, which is what we did. This is why we were able to create synthetic urine.
The device includes a pair of electrodeionization units - one for potassium, since these levels are necessary to maintain the electrical activity of the heart, and the other for all other ions.
It also has three other modules: ultrafiltration to retain blood cells and proteins in the body, nanofiltration to prevent glucose release, and a reverse osmosis module to modulate the amount of water released.
The system is designed to remove urine at a rate comparable to that of a healthy kidney, dispensing approximately the same amount of water consumed in a given day. It includes feedback sensors and custom software to monitor changes in blood chemistry.
Standard dialysis machines expose blood to dialysate through a membrane; the difference between the composition of the dialysate and the blood determines which ions leave the body and enter the dialysate. Unlike dialysis, this approach does not require purified water or dialysate, which complicate the work of doctors and the lives of patients.
Recently, a prototype of such a device was tested on animals, including pigs, whose kidney function is very similar to the functioning of this organ in humans.
Test results showed that the technology could measure (and likely in the future monitor) the level of potassium removed from the blood and then transferred into artificial urine under computer control.
The current prototype of this device is a wearable device the size of a small suitcase, which in the near future is expected to be improved, significantly smaller, and biocompatible to enable its implantation into the human body.
USKRC estimates that if sufficient funding is secured, human trials could be initiated in two to two and a half years.
The reason this technology is a game-changer, the developers say, is its ability to purify the blood of patients with end-stage renal disease without the need for dialysis procedures. This changes the methodology that has been practiced for decades, resulting in a paradigm shift.
In the near future, the developers plan to refine each of the components of their device. He intends to change the ultrafilter so that the patient does not need heparin or an anticoagulant. In addition, they plan to redesign the ultrafilter so that the filter itself contains components that will prevent blood clotting and improve electrodeionization units.
Qidni Labs
The company, Qidni Labs, is creating a fully implantable artificial kidney that uses a nanofiltration system to mimic the function of the organ. The prototype developed by the company’s specialists has already proven itself well when implanted in pigs.
The device's filter is made of ultra-thin crystalline silicon membranes, which are coated with a biocompatible material so as not to provoke an immune reaction. Today, such silicon membranes can be mass-produced with pore sizes ranging from 5 to 20 nanometers—large enough to allow waste particles to pass through, but too small for blood cells.
According to the developers, this device will continuously filter the patient's blood for many years, without requiring maintenance or cleaning, which will free the patient from dialysis machines forever.
Based on this technology, the company also plans to release a wearable miniature dialysis machine, which is likely to hit the market before the implantable device. Qidni Labs is currently testing its devices and, if all goes according to plan, the developers expect these devices to hit the market in four to five years.
The project is currently at the preclinical stage.
Lab-grown live buds
Several researchers around the world are trying to grow a complete human kidney using kidney cells from embryos, stem cells taken from adults, or cloned tissue.
In particular, a team of scientists from the University of Manchester became the first in the world to grow the parts of the kidney (nephrons) that filter blood in the laboratory using human stem cells. The nephrons grown in this way were then implanted into mice and showed their ability to filter blood and produce urine, similar to how a normal kidney works.
The new structures contained most of the components present in human nephrons - including proximal tubules, distal tubules, Bowman's capsule and loop of Henle.
With healthy kidneys having about 1 million nephrons each, the process would have to be scaled up to grow entire organs ready for transplantation. The benefit of using a patient's own stem cells is that it can help prevent the body from rejecting a lab-grown kidney (which can happen with today's kidney transplants).
This research is in its early days and much more work is needed, but the ability to grow nephrons in the laboratory is already a remarkable achievement.
Source: https://evercare.ru/news/implantiruemaya-iskusstvennaya-pochka-obzor-segodnyashnego-sostoyaniya-tekhnologii
Main types of artificial kidney devices
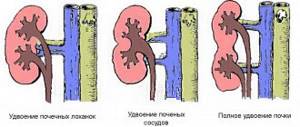
According to the anatomical structure, the human body has a paired organ - the kidneys.
They perform a very important function throughout the body: they are responsible for the processes of urine excretion.
If any disturbances occur in the functioning of one of the kidneys, a person’s general condition worsens, metabolic products begin to accumulate in the body, and general intoxication occurs.
If the process is at an advanced stage, it can even lead to death.
The kidneys are directly involved in such body processes as:
- circulation;
- removing excess fluid from the body in the form of urine;
- regulation of the amount of salt ions in the human body;
- participation in endocrine and metabolic reactions.
It is important to note that many people with some form of kidney disease have high blood pressure. However, today, thanks to the discoveries of scientists, an “artificial kidney” device or hemodialysis helps in the fight against kidney failure.
Hemodialysis concept
The use of an “artificial kidney” device allows the patient’s blood to be completely purified outside his body. This is the essence of the hemodialysis process. In this case, blood circulation occurs through a special filter that is attached to the dialysis machine.
In fact, it completely replaces the work of incompetent kidneys. The goals of this method are:
- getting rid of accumulated breakdown products of protein compounds (for example, urea);
- cleaning of excess creatinine, bringing its level back to normal;
- removal of toxic substances;
- removal of accumulated substances from medicines;
- cleaning from alcohols and electrolytes;
- removal of excess fluid.
Thanks to hemodialysis, the body's functioning is improved, toxins are eliminated, the balance of electrolytes is equalized, and blood pressure is normalized.
Today, it is performed mainly in hospital settings.
For hemodialysis, a machine called an “artificial kidney” is used. It includes the following elements:
- a special device that helps blood flow during cleaning;
- dialyzer, in which blood purification occurs;
- containers for solutions that purify blood;
- device screen on which the entire process is visualized and controlled.
The principle of its operation is as follows:
- through special tubes, blood from the patient’s vein enters the device;
- the device is equipped with a special double-sided filter, which during the cleaning process allows the patient’s blood to flow on one side and a special cleaning solution on the other;
- During the cleansing process, this solution rids the blood of all toxins and excess fluid.
It is important to note that cleaning solutions are selected for each patient separately. The feed speed is also individually set. On average, this process takes about 5-6 hours.
To remove toxins from the blood, engineers have created a medical device called an “artificial kidney.” The weight of stationary equipment is more than 80 kg.
This device cleanses the blood of waste products. The procedure itself is called hemodialysis.
The “artificial kidney” (AKD) device is based on the biological processes of cleansing the body of toxic substances and removing them, carried out by the kidneys. During hemodialysis, the patient's blood volume does not change.
By design, hemodialysis equipment comes in three types:
- stationary. This is a bulky device installed in clinics;
- portable. A smaller, portable analogue of a stationary device that can be used at home;
- implantable artificial kidney. It is not yet possible to use such a device in practice, since this is the latest development of scientists, which is currently undergoing the necessary tests.
There are several main types of hemodialysis machines, differing in the type of filters:
- Disk. Such structures consist of 25-35 plates that act as a frame. Between them there are 2 sheets of semi-permeable membrane. The plates protect the membranes from rupture. Blood flows between the sheets. The disadvantage of this type of device is the small volume of liquid being processed.
- Capillary. In such models, the membrane consists of many hollow fibers. The blood passes inside the capillaries, which are washed externally by the dialysate solution.
Based on filtration speed, membranes are divided into the following groups:
- normal (medium speed);
- highly efficient (high speed);
- high-precision (high accuracy at medium speed).
Each hospital strives to purchase the most modern model of the device. However, due to the high cost, not all institutions can afford them.
A stationary device is a kidney support device installed in a medical institution. The design of such a device consists of:
- hemodialyzer with a filtration membrane;
- water purification systems;
- pumping station;
- monitor.
For the patient’s convenience, a chair-bed is installed next to the device.
Modern models of hemodialysis equipment can operate autonomously. They monitor the patient’s condition, prepare the dialysate solution themselves, and adjust its composition depending on the patient’s parameters.
In this case, the entire cycle is automated, including filling the systems and flushing them.
Hemodialysis procedures are performed on an outpatient basis or in a hospital setting.
Blood purification requires strict supervision by medical personnel. This allows you to prevent possible complications that may arise after the procedure.
Thanks to new developments by medical equipment manufacturers, patients with kidney disease have the opportunity to carry out the procedure at home. The portable artificial kidney is small in weight (from 4 to 7 kg), but effective.
The advantages of such a device are:
- no need to go to the hospital;
- the ability to carry out a vital procedure in comfortable conditions;
- safety due to individual use of the device.
However, along with the advantages, there are also disadvantages: the high cost of a portable “artificial kidney” and the need for preliminary training of users to operate the device.
Developments in the field of medicine do not stop. Recently, scientists from the USA presented a new device - an “artificial kidney” for implantation. This device is designed to solve the problem of a shortage of donor kidneys for transplantation.
The essence of the development is to carry out an operation to implant a compact device into the human body that can perform the function of the kidneys.
It contains biological filters consisting of kidney cells. The device will work thanks to natural blood pressure.
The device is currently being tested in laboratory conditions. Developments are being carried out to improve the device and increase the efficiency of blood purification.
Notes
- An implantable artificial kidney has been developed in the USA
- Improving Dialysis Patients' Quality of Life with Miniature Artificial Kidney
- Artificial kidney created from human
- The Independent: Scientists close in on pioneering transplant of synthetic kidney
- Nature Medicine: Bioengineered kidney makes urine after transplantation
To improve this article it is desirable:
|
Indications for use
The main indications for hemodialysis are:
- chronic and acute renal failure;
- poisoning with toxic substances;
- excess of drugs in the body;
- alcohol poisoning;
- burns, cystic fibrosis, intestinal obstruction or other diseases that cause electrolyte imbalance in the body;
- drug overdose.
Among the contraindications to hemodialysis are the following:
- the presence of an infection in the body, which, under the influence of this procedure, spreads faster through the blood;
- patients after stroke;
- mental disorders (neuroses, psychoses, schizophrenia);
- tuberculosis or other diseases of the respiratory system;
- the presence of malignant tumors;
- disorders of the cardiovascular system;
- age category of patients after 75 years;
- various diseases of the circulatory system.
If there is a need for emergency hemodialysis, then contraindications are not taken into account.
There are a number of contraindications for hemodialysis:
- bleeding of various types;
- severe form of arterial hypertension;
- infectious diseases;
- heart attack and ischemic stroke;
- open tuberculosis;
- oncological diseases;
- diseases of the central nervous system;
- diabetes mellitus in patients over 70 years of age;
- pathologies affecting blood clotting.
Also, the blood filtration procedure is not performed for people over 80 years of age and for patients who have two or more chronic diseases.
However, there is an exception: when it comes to saving the patient’s life, contraindications are not taken into account. He is connected to a machine to cleanse the body of toxins, and if side effects occur, additional treatment is prescribed.
Cost of hemodialysis
The hemodialysis procedure is very expensive. This is due to the high price of equipment and solutions for blood purification. On average, one session costs from 3 to 7 thousand rubles per session.
On average, 3 sessions per week are required. As a result, the price of hemodialysis varies from 9 to 21 thousand rubles.
When carried out at home, the price is slightly lower. The main amount is made up of an “artificial kidney” device and a specialist who monitors the patient’s condition.
In emergency cases, the patient can undergo the procedure free of charge.
Notes[ | ]
- An implantable artificial kidney has been developed in the USA
- Improving Dialysis Patients' Quality of Life with Miniature Artificial Kidney Archived December 20, 2010 on the Wayback Machine
- Artificial kidney created from human
- The Independent: Scientists close in on pioneering transplant of synthetic kidney
- Nature Medicine: Bioengineered kidney makes urine after transplantation
To improve this article it is desirable:
Please, after fixing the problem, remove it from the list of parameters. After eliminating all the shortcomings, this template can be deleted by any participant. |
Quality of life and prognosis
If you have doubts about the benefits of hemodialysis, it is worth considering how long people live agreeing to an unpleasant procedure. According to statistics, extracorporeal blood purification increases life expectancy by 15-20 years. Important conditions: sessions cannot be postponed until the next day or skipped; It is forbidden to stop taking prescribed medications on your own and break your diet.
If you do not transplant the affected organ, but regularly use the “artificial kidney” device, you can live another 20 years, but then you will have to “sit” on the procedure for life. In this case, the patient dies not from kidney failure, but from inflammatory or infectious diseases and their consequences. This is due to a severe weakening of the immune system, against the background of which any pathogen can cause irreparable harm to health and life.
Meals during sessions
Before blood purification begins, the patient is vaccinated against hepatitis B, as well as a preventive conversation.
Be sure to measure the patient's temperature, blood pressure and pulse.
It is also very important for the correctness of the calculation to know the exact weight of the patient; it is measured before each session. Next, the person takes a position that is comfortable for him: half-sitting or lying on the couch. Two catheters are connected to his arm: one of them passes through an artery, the other through a vein.
The process is quite painful.
After this, the desired flow rate of the cleaning solution and the duration of the procedure are set on the device monitor.
Thus, blood moves through one of the tubes, and the dialysate solution moves through the second. During hemodialysis, a person may feel sick due to large fluid loss.
After the cleaning process is completed, a tight bandage is applied to the hand and the patient is allowed to lie down for a while.
The frequency depends on the patient’s disease:
- in case of renal failure, carry out 2-3 times a week for 4-5 hours each;
- in case of poisoning with toxins or alcohol, hemodialysis is carried out once for 12-14 hours;
- if there is an excess of medications in the body, 1 hemodialysis is enough;
- If there is an imbalance of electrolytes or accumulation of narcotic substances, it is enough to carry out the procedure 2-3 times a week for 3-5 hours.
The number of sessions and their duration are selected by the doctor individually for each patient.
Proper nutrition plays a very important role. It is necessary to avoid taking salt, foods with potassium and phosphorus. It is important to remember that during treatment it is not recommended to drink a lot of liquid. There is no need to rely heavily on fish or dairy products.
Avoid eating spicy and fried foods. If, nevertheless, the patient could not resist and ate something from the prohibited foods, then it is necessary to warn the doctor about this. He will take this fact into account in future sessions.
What does hemodialysis do?
An artificial kidney takes over the functions of the damaged organ. Medical professionals call the kidney the human laboratory. Her work influences the state of the body. The tasks of the kidney are:
- The kidney performs the cleansing function of the plasma of blood cells; the organ rids the blood of metabolic products and other compounds after taking medications.
- The kidney monitors the concentration of electrolytes in the blood vessels.
- This organ regulates blood pressure by removing fluid from the body and normalizing electrolytes in the body.
- The kidneys provide the necessary level of fluid in the body, on which the functioning of the organs depends.
- The kidney synthesizes active substances that are involved in maintaining blood pressure and are the basis for the creation of red blood cells.
An artificial kidney takes over the functions of a damaged organ
The positive thing is that a damaged kidney, even with 1/5 of all nephrons, is able to maintain the functions necessary for the body. If one of the kidneys stops functioning, the second one can take over the tasks of the damaged one.
The patient's condition is worse if 2 kidneys are affected at once. In such a situation, medical specialists prescribe hemodialysis, which takes over the tasks of the kidneys. Chronic renal failure can lead to this situation.
Operating principle of the device
By design, the “artificial kidney” is a complex device with several flexible tubes and reservoirs.
The device consists of several elements:
- dialyzer;
- perfusion device (a kind of pump);
- a device that mixes and supplies the dialysis solution;
- monitor to control the speed of blood circulation.
The perfusion device supplies blood to the dialyzer and, after purification, returns it to the body.
The basis of the device is a dialyzer. This is a tank consisting of two parts. A membrane for filtration is installed between the sections. On one side, blood is supplied to it, and on the other, a solution for dialysis.
Dialysis solutions are saturated with electrolytes in almost the same concentration as in blood plasma. After blood purification, waste is removed from the chamber using flexible tubes.
The physicochemical principles of the functioning of an artificial kidney are based on blood filtration. At the same time, substances with low molecular weight (potassium, sodium, creatinine, ammonia, chlorine, etc.) are removed from the blood.
The filtration process is fully controlled by medical personnel using a monitor that displays the main indicators.
Normally, the blood flow rate is 300-450 ml/min. If it is lower, the duration of the process increases. At higher speeds, the blood is purified less efficiently.
A special fistula connecting the vein and artery allows the speed to be normalized. It is formed during a special operation and allows you to connect the device as needed without harm to the vessels.
A fistula is necessary in cases of frequent dialysis.