Glomerulosclerosis
Glomerulosclerosis is a sclerotic process in the renal glomeruli. This pathology is not considered independent, but occurs against the background of other pathological processes occurring in the body. Often, glomerulosclerosis is an integral part of nephrotic syndrome and is accompanied by hypertension and kidney failure.
A similar pathological syndrome manifests itself in the formation of scars or deposits, which subsequently leads to inevitable damage to the glomerular apparatus. Glomeruli or glomeruli are tubular filters that purify the blood and remove excess into the urine.
Focal segmental glomerulosclerosis: symptoms, diagnosis, treatment, prognosis
Focal segmental glomerulosclerosis (FSGS) is the leading cause of kidney disease worldwide.
The suspected etiology of primary FSGS is a plasma factor with responsiveness to immunosuppressive therapy and risk of relapse after kidney transplantation.
Adaptive FSGS is associated with excessive nephron load due to increased body size, decreased nephron capacity, or single glomerular hyperfiltration associated with some diseases.
Introduction
Focal segmental glomerulosclerosis is the leading glomerular cause of renal failure. He refers to a histologic pattern that characterizes 6 possible underlying etiologies, sharing the common theme of contusion and podocyte depletion.
Diagnosis of focal segmental glomerulosclerosis relies on the integration of clinical history (family history, birth history, peak weight and body weight, medication use), clinical laboratory findings (serum albumin, urine protein, and viral serologies) and renal histopathology. Proteinuria may be in the nephrotic or subnephrotic range. Elimination of other systemic diseases or primary renal pathologies that may lead to a similar presentation is critical.
Epidemiology and global burden
The prevalence of focal segmental glomerulosclerosis, compared with other diagnoses of similar diseases, is increasing throughout the world. However, the absolute incidence and prevalence are difficult to establish given the large global variations in indications, availability, and pathologic support for renal biopsy.
A review of the published literature worldwide was conducted and shows annual incidence rates ranging from 0.2 to 1.8 per 100,000 population per year. The average incidence rate was 2.7 patients per million. There is significant racial-ethnic predisposition. In addition, symptoms of kidney failure in women are milder than in men.
Typology
The classification of focal segmental glomerulosclerosis is multifaceted. It includes pathophysiological, histological and genetic aspects. FSGS was originally divided into primary (idiopathic) and secondary forms. The latter includes familial (genetic), virus-associated, and drug-induced forms.
Clinical guidelines for focal segmental glomerulosclerosis may relate to the histological variant, primarily the glucocorticoid reactivity of the tip lesion and the aggressive, inexorable nature of the collapsing variants.
6 clinical forms
By combining genetic susceptibility, pathophysiological factors, clinical history, and response to therapy, it is useful to group FSGS into six clinical forms. They include:
- primary;
- adaptive;
- highly genetic;
- virally mediated;
- drug-related;
- APOL1-related.
Minimal symptoms of glomerulonephritis in adults are the absence of tubulointersital scarring. The tip lesion represents focal adhesion of the glomerular tuft to Bowman's capsule near the proximal takeoff of the tubule.
The most typical option is collapsing. A specific example can be appreciated in the installation of endothelial tubulo-reticular inclusions observed during ultrastructural analysis.
They can be observed in high interferon states, including viral infection.
Minimal disease change and tip involvement are the most responsive and least progressive, and collapsing glomerulopathies are treatment-resistant and rapidly progressive.
Signs indicating illness
Signs and symptoms of glomerulonephritis in adults depend on whether there is an acute or chronic form. These include:
- Pink or brown-colored urine due to an increased number of red blood cells (hematuria).
- Foamy urine due to excess protein (proteinuria).
- High blood pressure (hypertension).
- Fluid retention (edema). Appears on the face, arms, legs and stomach.
Symptoms of kidney failure in women are highlighted separately:
- Reduced urine output.
- Fluid retention causing swelling of the legs.
- Dyspnea.
- Fatigue.
- Confused consciousness.
- Nausea.
- Weakness.
- Irregular heartbeat.
- Pain in the kidney area.
- Fainting or coma in severe cases.
The surest way to identify FSGS
The first thing to do is a urine test for your kidneys. It includes two tests:
- Albumin to creatinine ratio. Too much albumin in the urine is an early sign of kidney damage. Three positive results within three months or more is a sign of disease.
- Glomerular filtration rate. The blood is tested for a waste product called creatinine. It comes from muscle tissue. When the kidneys are damaged, problems arise in removing creatinine from the blood. The test result is used in a mathematical formula with age, race, and gender to determine the glomerular filtration rate.
Main reasons
Conditions that can lead to inflammation of the kidney glomeruli include:
- Infectious diseases. Glomerulonephritis can develop 7-14 days after a skin infection (impetigo) or streptococcal throat infection. To fight them, the body is forced to produce many additional antibodies, which can ultimately settle in the glomeruli, causing inflammation.
- Bacterial endocarditis. The bacteria can spread through the bloodstream and lodge in the heart, causing infection of one or more heart valves. Bacterial endocarditis is associated with glomerular disease, but the relationship between the two is unclear.
- Viral infection. Human immunodeficiency virus (HIV), hepatitis B and C can cause the disease.
- Lupus. May affect many organs and parts of the body, including blood cells, skin, kidneys, heart, joints and lungs.
- Goodpasture's syndrome. This is a rare lung disease that mimics pneumonia. It can cause glomerulonephritis and bleeding in the lungs.
- Nephropathy. This primary glomerular disease occurs due to deposits of immunoglobulin in the glomeruli. May progress for years without noticeable symptoms.
Additional reasons
Additional causes of the disease include:
- Polyarteritis. This form of vasculitis affects small and medium-sized blood vessels. Known as Wegener's granulomatosis.
- High blood pressure. Kidney function decreases. They process sodium less well.
- Focal segmental glomerulosclerosis. Characterized by diffuse scarring of some glomeruli. This condition may be the result of another disease or occur for an unknown reason.
- Diabetic kidney disease (diabetic nephropathy).
- Alport syndrome. Hereditary form. May also impair hearing or vision.
- Multiple myeloma, lung cancer and chronic lymphocytic leukemia.
Mechanism of disease
Focal segmental glomerulosclerosis is a diverse syndrome that occurs after podocyte injury for various reasons. The sources of damage are various:
- circulating factors;
- genetic abnormalities;
- viral infection;
- drug treatment.
For the most part, the interactions between these drivers are unclear and complex. For example, adaptive FSGS involves both podocyte stress (mismatch between glomerular load and glomerular capacity) and genetic susceptibility.
Damage to podocytes from any form of FSGS (or from other glomerular diseases) initiates the process leading to acute nephritic syndrome. There is a progressive loss of damaged podocytes into the urinary space. To balance the deficiency, these cells compensate by hypertrophy, covering the surfaces of the glomerular capillaries.
In adaptive FSGS, glomerular hypertrophy occurs early in the disease process. In other forms, glomerular hypertrophy occurs with progressive loss of the nephron. This leads to increased pressures and flows in the remaining glomeruli of the patent.
The following sections discuss the pathological mechanisms, therapy and treatment of focal segmental glomerulosclerosis.
Primary FSGS
Includes genetic, viral and drug-related FSGS.
The mechanism of podocyte injury involves a circulating factor, possibly a cytokine, that renders specific patients susceptible. This is the most common form in teenagers and young adults.
It is usually associated with nephrotic proteinuria (sometimes massive), decreased plasma albumin levels, and hyperlipidemia.
Currently, therapy for primary FSGS is based on immunosuppressive agents. These are glucocorticoids and calcineurin inhibitors that directly modulate podocyte phenotype.
Recurrent FSGS remains a clinical problem. Only one of 77 initial renal biopsies from patients who subsequently relapsed showed a perihilar variant.
Plasma exchange therapy may cause temporary remission.
Adaptive FSGS
Occurs after a period of glomerular hyperfiltration at the nephron level and hypertension after pathophysiology. Conditions that are associated with its development include:
- congenital cyanotic heart disease;
- sickle cell anemia;
- obesity;
- androgen abuse;
- sleep apnea;
- high protein diet.
The duration of single-nephron glomerular hyperfiltration is usually measured decades before glomerulosclerosis progresses.
Adaptive FSGS leads to progressive cycles of glomerular hypertrophy, stress and exhaustion, and excessive deposition of extracellular matrix in the glomerulus.
Renal biopsy features that support the diagnosis include large glomeruli, predominance of perihilar scars demonstrating sclerotic changes. Clinical features include normal serum albumin, which is unusual in primary FSGS.
Genetic FSGS
Takes two forms. Some patients with a certain genetic predisposition will develop the disease, while others will not. The number of genes associated with FSGS is increasing every year, in large part due to the proliferation of whole exome sequencing. To date, at least 38 have been identified.
Several genes are associated with the syndrome, which includes extrarenal manifestations. This may provide a clinical clue that the patient may have a mutation in a particular gene. Others are associated with characteristic changes in basement membrane morphology or mitochondrial morphology.
If the family has not previously had genetic testing, the most effective approach is to use panels targeting early FSGS (infancy and childhood). Genetic testing resources around the world are available from the National Center for Biotechnology Information and the National Institutes of Health.
Source: https://FB.ru/article/474154/fokalnyiy-segmentarnyiy-glomeruloskleroz-simptomyi-diagnostika-lechenie-prognoz
Causes
A number of reasons can lead to the occurrence of glomerulosclerosis:
- Chronic liver pathologies such as cirrhosis;
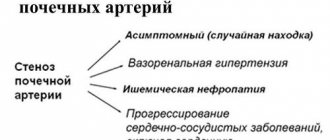
- Renal atherosclerosis, associated with hardening of the renal arteries;
- Severe forms of glomerulonephritis, accompanied by progressive renal lesions;
- Nephrotic syndrome of idiopathic form;
- Diabetes;
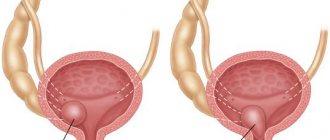
- Reflux nephropathy, which is characterized by the reverse flow of urine from the bladder structures into the kidney;
- Drug therapy with certain drugs;
- Hypertonic disease.
In some cases, mild glomerulosclerosis occurs with age. Starting from the 30th birthday, kidney function decreases by 10% with each decade, i.e. at 40 years old the kidneys will work at 90%, and at 50 years old - at 80%, etc. In addition, there is some tendency to glomerulosclerosis in black men. It is rare in children.
Signs indicating illness
Signs and symptoms of glomerulonephritis in adults depend on whether there is an acute or chronic form. These include:
- Pink or brown-colored urine due to an increased number of red blood cells (hematuria).
- Foamy urine due to excess protein (proteinuria).
- High blood pressure (hypertension).
- Fluid retention (edema). Appears on the face, arms, legs and stomach.
Symptoms of kidney failure in women are highlighted separately:
- Reduced urine output.
- Fluid retention causing swelling of the legs.
- Dyspnea.
- Fatigue.
- Confused consciousness.
- Nausea.
- Weakness.
- Irregular heartbeat.
- Pain in the kidney area.
- Fainting or coma in severe cases.
Forms and types
Depending on the etiological and structural features, glomerulosclerosis is divided into several specific types:
- Focal segmental - this variant of glomerulosclerosis occurs in 6-10% of patients with a chronic form of glomerulonephritis. The basis of this form of pathology is damage to epithelial cellular structures, in which sclerosis of individual glomerular segments occurs. Characteristic signs of this form of glomerulosclerosis are nephrotic syndrome, persistent proteinuria, hematuria and hypertension.
- Diabetic – this form of glomerulosclerosis is considered the most severe complication of diabetes. More common in women. It manifests itself as an increase in pressure inside the glomeruli, then microalbuminuria joins, and then pronounced proteinuria and nephrotic syndrome. Terminal failure develops approximately 6-10 years after the onset of proteinuria.
- Focal-global - sclerotic lesions cover the entire glomerular apparatus.
- Segmental - lesions are localized in a specific segment of the organ.
- Focal-focal - sclerotic processes in the glomerular apparatus of the kidney are focal in nature.
Forms and types of glomerulosclerosis
Definition of the concept
Diabetic glomerulosclerosis is also called diabetic nephropathy and Kimmelstiel-Wilson syndrome - this name appeared thanks to two pathologists who discovered this kidney damage. In people with diabetes after 20 years of age, this disease occurs in 20-60% of cases (data vary greatly in different sources), and women are more susceptible to it.
Basically, diabetic glomerulosclerosis develops in insulin-dependent diabetics, and insulin-independent individuals suffer from it much less frequently.
The kidneys are covered with a special tissue - fascia, which serves as protection from mechanical damage. Under the fascia, the kidneys are represented by the medulla and cortex. The places where the cortex dissects the brain structure are called renal pyramids. They are lobule-like and include glomeruli called glomeruli. It was the glomeruli that gave the disease its name.
Symptoms
Characteristic signs of sclerotic lesions of the glomerular apparatus, depending on its cause, may include:
- Diabetic signs;
- Clinical manifestations of liver pathologies or hepatorenal syndrome;
- Nephropathic signs – pain in the lumbar area, back, etc.;
- Hyperfluidity;
- Signs of blood in the urine;
- The daily volume of urine excreted increases sharply or, conversely, decreases.
The course of the pathology can be seriously complicated by proteinuria and nephrotic syndrome, which leads to an increased frequency of relapses and more frequent deaths from the pathology. In the video about the causes and symptoms of focal segmental glomerulosclerosis:
Diabetic option
Diabetic glomerulosclerosis or intercapillary occurs as a result of severe variants of diabetes mellitus. In medicine, this disease was given the name Kemmelstil-Wilson syndrome, which was the name of the person who first described this disease. There are a number of other names for diabetic glomerulosclerosis, for example, diabetic kidney, diabetic nephropathy.
The term diabetic nephropathy is justified, since there is not only damage to the capillaries of the glomerular apparatus; other vessels are always involved in this process.
There are many hypotheses for this syndrome, but its causes are not fully known. The most common version is a metabolic disorder, increased permeability of the glomerular basement membrane. As a result, a hyaline substrate is deposited on it, which impairs the function of the glomeruli.
Symptoms of nephrosclerosis
It is more common in women, especially those with metabolic disorders. Kidney damage develops against the background of a failure in the normal metabolic process of carbohydrates, fats, and proteins. Hereditary factors and autoimmune reactions also play a role.
There is a general classification of vascular damage of diabetic origin. There is an initial stage in which there are few symptoms. Next comes the transitional stage, with which the symptoms are already clearly visible. And the final stage or stage of glomerulosclerosis.
Based on the speed of development of disorders, a distinction is made between slowly progressing and rapidly progressing variants. It is worth noting that diabetic glomerulosclerosis is also divided on the basis of its combination with vascular pathology of other locations, for example, with pyelonephritis.
The leading manifestation of the disease will be protein in the urine, arterial hypertension, and damage to the visual organs. The symptoms of the disease depend on the stage of the disease at the moment. The initial manifestation will be protein in the urine (up to 0.33 grams per liter); it occurs against the background of normal filtration rates in the glomeruli. If the disease continues for a sufficiently long time, both albumin and larger compounds are detected in the urine; the protein content sometimes reaches 25 grams per liter.
Pyelonephritis is often accompanied by sclerosis of the glomeruli of the kidneys
In addition to protein in the urine, leukocytes, casts, and bacteria are also determined. The pathology of urine sediment during a long course of the disease is not particularly noticeable. Waxy casts can only be detected in cases of kidney failure. Later, inflammation develops in the kidney.
Its function gradually decreases, nitrogenous bases begin to circulate in the blood, and a disturbance in the exchange of electrolytes and lipids occurs.
Damage to the organs of vision occurs in the vast majority of cases; aneurysms of microscopic size appear in the retina, and there may be hemorrhage. If a doctor finds an aneurysm during an eye examination, the first thing he thinks about is diabetes. After all, this is a highly specific sign. As the disease progresses, a scar stage may occur in the retina, followed by detachment.
When glomerulosclerosis of diabetic origin occurs, the leading symptom will be hypertension. It is combined with eye damage and protein in the urine. Thus, it can be differentiated from hypertension of an atherosclerotic nature. Hypertension occurs due to activation of the renin-angiotensin-aldosterone system.
As the disease progresses, nephrotic syndrome is added to the general symptoms. But uremia appears with complete kidney failure; it manifests itself with all the signs of chronic kidney failure.
In addition to all of the above, the vascular system of the heart, legs, and brain is affected. Thrombotic phenomena are not uncommon, there may be heart attacks, polyneuropathic processes. At the final stages of the disease, pyelonephritis occurs.
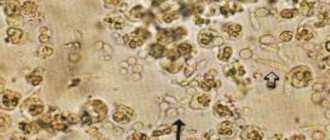
Histological picture of the pathology
A patient with diabetic glomerulosclerosis is monitored by both a nephrologist and an endocrinologist.
Diagnostics
Diagnostic tests are limited to traditional ultrasound examination of the kidneys. Laboratory tests are also prescribed for the presence of proteinuria and hematuria, the Rehberg test, which shows the rate of filtration activity of the glomeruli. Renal and hepatic functions, etc., are carefully examined.
The patient is also prescribed an extensive kidney examination, X-ray and MRI, radiation and radioisotope diagnostics, biopsy and uroflowmetry, urodynamic studies, etc.
Treatment
Therapy is often based on steroid drugs. A prerequisite for treatment is monitoring and maintaining the patient’s normal blood pressure.
- In the absence of nephrotic syndrome, the use of ACE inhibitors is indicated, providing an antiproteinuric effect and helping to slow the progression of chronic renal failure.
- Patients are also prescribed corticosteroid therapy (Prednisolone).
- Cytostatics such as Cyclophosphamide and Chlorbutin, when combined with drugs of the glucocorticoid group, further help reduce the likelihood of relapse, i.e., ensure the stability of the achieved remission.
- Immunosuppressive therapy with Cyclosporine is also prescribed.
In general, patients are recommended to eat a low-protein diet, which has a positive effect on intraglomerular hypertension. If the pathology is accompanied by hypoalbuminemia, then reducing the consumption of protein foods will not be effective.
In the presence of nephrotic syndrome, a low-cholesterol diet is recommended; it is recommended to consume foods with polyunsaturated acids such as sunflower oil or fish.
When undergoing renal transplantation, most patients experience a relapse of glomerulosclerosis, so organ transplantation often does not make therapeutic sense.
Diet therapy
For diabetic glomerulosclerosis, it is necessary to follow certain principles of diet therapy:
- Food should be hypocaloric. This means a significant reduction in the proportion of fats and carbohydrates. Basically, you need to limit fats to 30-50 grams per day. Read more about the low carb diet.
- Ensure adequate protein intake. The norm is calculated based on the patient’s body weight. On average, 1 kg of weight per day should contain 0.8 grams of protein.
- If the glomerular filtration rate is reduced, a low-protein diet will be needed. In this case, the patient should include at least 30-40 grams of protein in his diet per day. It is important that there is sufficient caloric content of foods, otherwise the patient may develop protein-energy deficiency. The process must be supervised by a doctor.
- Limit your intake of foods containing cholesterol. It must be replaced with vegetable oil.
- Meals should be divided - 5-6 meals per day. This allows you to ensure uniformity of blood sugar levels throughout the day, since sharp fluctuations in this indicator have a pathological effect on the blood vessels.
- If diabetic glomerulosclerosis is accompanied by arterial hypertension, then the patient needs a low-salt diet. He should consume no more than 4-5 grams of table salt per day.
- Fluid restriction. If you have diabetes, you can drink it without restrictions, but concomitant kidney problems prevent this permission. You should completely avoid alcohol and carbonated drinks.
- Exclusion of products with a diuretic effect. This rule must be remembered when taking medicinal decoctions, which are allowed and recommended for diabetes.
Consequences and forecasts
The prognosis for focal segmental glomerulosclerosis is quite serious, especially when complicated by nephrotic syndrome, which occurs in almost 70% of patients. This variant of the course of the disease is considered by nephrologists as the most unfavorable and not responsive to the immunosuppressive approach to treatment. 5-year survival rate reaches 71-73%.
In such patients, terminal renal failure develops within 5-8 years, and if proteinuria is present along with nephrotic syndrome, then failure occurs within a couple of years. If nephrotic syndrome and hypertensive nephritis are absent, then the prognosis is more favorable - the 10-year survival rate exceeds 80%.
Primary FSGS
Includes genetic, viral and drug-related FSGS. The mechanism of podocyte injury involves a circulating factor, possibly a cytokine, that renders specific patients susceptible. This is the most common form in teenagers and young adults. It is usually associated with nephrotic proteinuria (sometimes massive), decreased plasma albumin levels, and hyperlipidemia.
Currently, therapy for primary FSGS is based on immunosuppressive agents. These are glucocorticoids and calcineurin inhibitors that directly modulate podocyte phenotype. Recurrent FSGS remains a clinical problem. Only one of 77 initial renal biopsies from patients who subsequently relapsed showed a perihilar variant. Plasma exchange therapy may cause temporary remission.