The only treatment option for kidney failure that can provide long-term results and improve the patient’s quality of life is a kidney transplant. Thanks to the transplantation of this organ, doctors were able to help more than one patient at the terminal stage. Despite the fact that such operations have been performed for a long time, the issue of kidney transplantation in Russia does not lose its relevance due to the huge number of patients in need of it. In our country, every eighth resident suffers from chronic diseases of the excretory system.
General information
We are talking about a complex surgical process, which involves the removal of organs or soft tissues from a donor and their implantation in the recipient. About half of the surgical operations performed in the world for the purpose of organ transplantation are kidney transplant procedures. About 30 thousand such interventions are carried out annually in the world.
Transplantology has made the whole world talk about itself, since it is this treatment technique that demonstrates high survival rates among hopeless patients. In 80% of cases, patients overcome the five-year threshold after a kidney transplant.
Compared to dialysis, which not so long ago was the only way to maintain the vital functions of seriously ill patients, renal transplantation significantly improves the patient’s quality of life, as it eliminates the need for constant stay in a medical institution. However, the wait for surgery may be too long due to a shortage of donor organs. Then dialysis becomes, in fact, the only way to maintain the functionality of the patient’s body. In addition, in order to keep the implanted kidney in satisfactory condition for as long as possible, the recipient will have to take medications until the last days, be periodically examined by specialists and be responsible to himself for his lifestyle, diet, work activity, etc.
Methods for obtaining a transplant
If a person needs a kidney transplant, the first step is to find a donor. The person wishing to donate his organ to someone in need can be a living person (in Russia this can only be a relative) or a deceased person, if before his death he or his relatives entered into an agreement to remove a kidney. The first option is more preferable, as it increases the recipient’s chances of organ survival. In the second case, a donor organ is collected from a person with documented brain death, which is documented.
Statistically, a kidney transplant from a living donor is more successful. This is due to the ability of the doctor to plan the operation in advance and get more time to undergo the examination and prepare the recipient, while the implantation of an organ of a deceased person is carried out as soon as possible due to the inability of doctors to delay the inevitable processes of tissue decomposition.
Forecast for adults
According to statistics, in the first year after surgery, if the kidney was received from a living donor, rejection will occur in 2% of cases. If the donor is deceased, the probability of rejection in the first year increases, amounting to 6%. And in subsequent years, the new element is threatened with death. This is primarily facilitated by the immune system. The kidney will never be perceived as something native, natural; it will forever remain a foreign object. That is why you will have to take additional medications. Any cold is a threat. After a kidney transplant, you need to pay a lot of attention to your health.
Every year of functioning, according to statistics, the kidney dies by 3-5% if the donor is a living person. It dies at 5-8%, if the donor was a deceased person. This reaction is not entirely clear. Scientists don't know why it dies. This is not rejection as such, but a gradual decline in performance. Rejection is a sudden process that develops rapidly and is a threat to life.
The problem of gradual loss of function, as well as rejection, is solved quite simply: sooner or later a new operation may be needed or you will have to agree to regular dialysis. However, by this time a revolution may occur in science and a revolutionary method of therapy will be invented, which has no equal.
Who is surgery recommended for?
The main indication for transplantation is serious impairment of kidney function. If a patient is diagnosed with chronic renal failure, this means that his body loses the ability to perform blood purification functions. This disorder can be partially compensated for by dialysis. End-stage renal failure is the last phase of chronic kidney pathologies, complications of congenital anomalies or damage. In this case, a kidney transplant operation or continuous use of renal replacement therapy, which is aimed at artificially removing toxic metabolic products from the body, is required. Otherwise, general intoxication of the body may occur and, as a consequence, the death of the patient.
Diseases that lead to chronic renal failure include:
- interstitial nephritis (inflammatory process in interstitial renal tissue);
- pyelonephritis (infectious organ damage);
- glomerulonephritis (disturbances in the functioning of the glomerular apparatus);
- renal polycystic disease (multiple benign tumors);
- nephropathy (damage to the glomerulus and parenchyma of the kidneys due to diabetes mellitus);
- kidney inflammation as a complication of systemic lupus erythematosus;
- nephrosclerosis (replacement of healthy parenchyma cells with fibrous tissue).
Forever?
My sister suddenly developed kidney problems, she was prescribed hemodialysis, will she have to undergo this procedure for the rest of her life?
Maria, Moscow
Article on the topic
Tricks of hemodialysis. When to go for renal replacement therapy - Hemodialysis is prescribed when the kidneys are dead. Dialysis can be compared to a wheelchair: if a person has no legs, he sits on a wheelchair and moves only with its help. Dialysis is a life-saving renal replacement therapy.
But our patients are more susceptible to any other diseases. The incidence of cardiovascular diseases in them is tens of times higher than in healthy people. The incidence of pneumonia is significantly higher.
A much better solution in case of death of one’s own kidney is transplantation of a donor one.
Are there any contraindications?
In modern transplantology, there is no consensus on in what cases an operation to engraft a donor organ is not recommended. The list of contraindications for kidney transplantation may vary slightly in different medical centers. Most often, patients are denied a transplant in the following cases:
- Incompatibility of the recipient's immunological reaction to the donor's lymphocytes. Not a single qualified specialist will undertake such an operation, since in this case the risk of hyperacute rejection of a foreign organ will be extremely high.
- Oncological pathologies. Transplantation is contraindicated even some time after tumor treatment. In the majority of cases, patients are allowed to undergo a transplant after at least two years have passed since radical cancer treatment. At the same time, in some medical centers specializing in transplantation, they do not wait any longer if kidney cancer, bladder cancer, cervical cancer, or skin basal cell carcinoma were successfully removed at an early stage. After treatment for cervical cancer, breast cancer, and melanoma, the observation period is increased to 5 years.
- Infections. Absolute contraindications to a donor kidney transplant include HIV infection, active hepatitis B, C, and tuberculosis. After cure for tuberculosis, the patient is monitored for at least a year.
- Chronic diseases that can worsen the patient's condition in the postoperative period. These include peptic ulcer of the gastrointestinal tract and heart failure.
Not so long ago, nephropathy, which occurs as a complication of diabetes mellitus, was considered a contraindication to kidney transplantation. Such patients actually have a worse prognosis for survival after transplantation, however, with correct and timely treatment, the patient’s chances of recovery increase several times.
It is not recommended to resort to a donor kidney transplant if the patient refuses to comply with medical instructions. Indiscipline of recipients in 5-10% of cases leads to rejection of the implanted organ. Refusal to follow the prescriptions prescribed by specialists regarding immunosuppressive therapy, diet and lifestyle is fraught with serious complications. Another contraindication associated with the patient’s inability to comply with the rules after a kidney transplant is mental disorders, changes in behavior due to drug addiction and alcoholism.
Of course, transplantation is not carried out if the donor and recipient have incompatible blood types. In addition to absolute contraindications, there are also relative ones. Children and elderly people receive a kidney transplant only in isolated cases, since such operations involve increased complexity and a low probability of organ survival. If a potential donor does not meet the stated requirements or has serious pathologies, his participation in the transplant is called into question, which can be dispelled by recommendations from highly specialized specialists.
Transplantation techniques
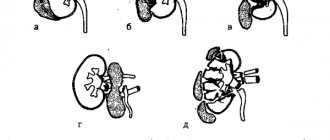
Operations to engraft an organ to a recipient are classified as follows:
- Isogenic transplantation. Here, the role of the donor is a blood relative - a person whose biological material has genetic and immunological similarities. This is the most common type of kidney transplant procedure.
- Allogeneic transplantation. A stranger becomes a donor if there is compatibility with the patient’s body. In our country, organs are transplanted only from a deceased donor.
- Replantation involves returning an organ to a person. The need for such an operation arises due to serious injury, separation or cutting off of an organ.
In addition, transplant operations are distinguished based on the location of the implanted organ. For example, the most complex is heterotopic transplantation, when a “foreign” organ is engrafted in its anatomically designated place, while the recipient’s non-functioning kidney is removed. In orthotopic transplantation, the engrafted organ is placed in a different location, most often in the iliac region, but the diseased kidney remains and is not removed.
How to prepare for a transplant
To understand whether to undergo a kidney transplant and whether this treatment option is advisable, the patient must undergo a comprehensive clinical examination. Comprehensive diagnostics will identify or exclude possible contraindications. Before a patient gets on the waiting list for a kidney transplant, he must:
- Take laboratory tests of blood, urine and sputum.
- Undergo X-ray, ultrasound and other types of instrumental studies (gastroscopy, electrocardiography, MRI, CT).
- Get advice from highly specialized specialists (psychologist, narcologist, otolaryngologist, dentist, cardiologist, gastroenterologist, hematologist). For female recipients, a recommendation from a gynecologist is also mandatory.
Before the actual operation, the patient will have to undergo a re-examination, since the wait for a suitable donor organ can take from several weeks to several months.
If there are no contraindications, the compatibility of the donor and recipient is determined, the patient is placed in an inpatient department. In some cases, a kidney transplant is preceded by dialysis - the procedure of artificial blood purification is resorted to a couple of days before the transplant. The patient is prescribed sedatives if his psychological state requires it.
The last consumption of food and liquid before surgery occurs 8-10 hours. In addition, the recipient must sign the appropriate papers to formalize his consent to carry out this type of intervention. The package of documents also includes confirmation of information about possible risks, threats to health and life.
Pre-kidney transplant screening in Singapore
Before the operation, the patient undergoes a full examination to assess the health of the whole body and various blood parameters (group, leukocyte antigens, coagulation, etc.). A cross-match test is carried out. This test helps determine the presence of antibodies against the donor kidney tissue. If immune cells that can destroy donor tissue are initially absent from the recipient's body, then the risk of rejection of the new organ is significantly reduced. Additional diagnostics before kidney transplantation in Singapore include x-rays, ultrasound, biopsy of diseased organs and testing for viral diseases (HIV, hepatitis and cytomegalovirus). If a patient has a potential donor, they will also undergo an evaluation of their overall health and kidney status.
How is the operation performed?
A kidney transplant from a living donor takes place in several stages. As a rule, the nephrectomy procedure in the recipient occurs almost simultaneously with the surgical removal of the donor organ, so such a transplant requires the participation of several teams of specialists. Compared to an operation to implant an organ from a deceased donor into a patient (here the kidney is prepared in advance), this surgical intervention can last much longer.
The transplantation is performed under general anesthesia. While one team of specialists performs a nephrectomy on the donor, the second prepares a site for the transplant in the recipient. After this, the organ is fixed and connected to the patient’s artery, vein and ureter. The next mandatory step is bladder catheterization.
The main indicator of a successful operation is the urine output of the transplanted kidney after just a few days. In the normal state of the organ, it reaches its full functionality within a week, therefore, according to reviews, a kidney transplant does not require a long stay in the hospital. If there are no complications, the patient is discharged after a couple of weeks.
The quality of life after a kidney transplant does not suffer for the donor either. One remaining organ grows over time and fully performs the necessary functions.
Possible complications in the future
The most terrible and irreversible complication in the process of postoperative rehabilitation is donor organ rejection. This happens because the immune system reacts to the kidney as a foreign protein. At the same time, lymphocytes produce antibodies that attack the foreign antigen. In addition, the donor organ contains microorganisms foreign to the recipient’s body, which, when entering the bloodstream, also activate the immune response.
Although the word rejection seems fatal and sudden, the rejection of an organ does not always mean the cessation of its functioning. This often happens in the postoperative period, and properly selected drugs can reduce the risk of kidney rejection. Of course, this is only possible if the donor is correctly selected and the operation is successfully performed.
In any case, timely medical intervention can have a positive impact on the process, stop it and save the donor organ.
Are kidney transplants given to children?
In adulthood, dialysis is much easier to tolerate than in early age. Such treatment can bring difficulties not only physically, but also mentally. Prolonged stay on dialysis interferes with the normal development and growth of the child. If the baby has an indication for transplantation, the operation must be performed as soon as possible. At the same time, in childhood, a kidney transplant, according to reviews, has a greater chance of a successful outcome. The organ takes root quickly, and the patient’s condition quickly stabilizes.
Difficulties often arise at the stage of finding a suitable donor. If an emergency kidney transplant is necessary, a child will receive an organ from an adult. However, this option is only possible if there is enough space in the retroperitoneal space of the small recipient for organ implantation. In addition, the risk of insufficient blood supply to the “new” kidney cannot be excluded due to the small diameter of the vessels. For children with heart or cardiovascular diseases, or mental pathologies, surgery is contraindicated.
Kidney transplantation: progress of the operation
The course of such an operation as a kidney transplant involves general anesthesia, as well as incisions in the abdominal wall above the groin - on the right and left. Next, a pre-prepared donor organ is placed in the lower segment of the abdominal cavity and the vessels of this organ are connected to the corresponding vessels of the recipient. Then, after blood flow has been restored in the new kidney, it should begin to filter the blood, releasing metabolic products, as it should.
The operation itself lasts approximately 4 hours. And the success rate depends largely on whether the donor was a relative or not. If yes, then the success rate is equal to 90%.
Life after surgery
When asked about a kidney transplant: “How long do people usually live with an implanted organ?” No specialist can give a definitive answer. The success of organ engraftment largely depends not only on the characteristics of the human body, but also on his strict adherence to the recommendations of the attending physician.
After transplantation, long-term rehabilitation is required, which involves bed rest, taking anti-inflammatory and immunosuppressive drugs, a radical revision of the daily menu and constant medical supervision. In general, the prognosis can be considered favorable; with high-quality intervention and a satisfactory course of the rehabilitation period, the person will certainly return to normal life. In some cases, a re-transplant is required after 15-20 years.
How long do people live after kidney transplant surgery?
When making a decision about a kidney transplant, people should know how long they can live with a transplanted kidney. The functioning of the transplanted kidney and its full functioning depends on many circumstances. First of all, it is important what condition the donor was in:
- if the kidney was taken from a deceased donor, then the organ functions on average for 5-10 years;
- if the organ was removed from a living donor, then the duration of its functioning can be more than 20 years.
The patient’s health condition depends on what therapy is prescribed, how well the main and auxiliary drugs were selected, how carefully the person monitored his health, whether he followed a dietary diet, and whether he followed all the recommendations of the nephrologist. It is important to constantly monitor the functioning of the transplanted kidney, and if a complication occurs, go to the hospital and undergo a full course of treatment. Then the person’s quality of life will improve, and the patient will not feel discomfort.
How to eat healthy with a kidney transplant
Diet allows you to minimize the risk of complications. Initially, after surgery, the patient can receive nutrients only through infusion of medicinal solutions. A patient can be prescribed a diet after a kidney transplant within 5-7 days.
The body of a person who has undergone such a serious surgical intervention especially needs a balanced supply of vitamins, calcium, phosphates, and nutrients. Weight gain is unacceptable, as extra pounds can lead to a number of negative consequences.
Doctors recommend adhering to the basic principles of nutrition after kidney transplantation not only for the recipient, but also for the donor:
- Limit salt intake, and it is advisable to avoid spices and spices altogether, since these substances contribute to fluid retention in the body and cause thirst.
- Do not include canned foods on the menu.
- Eliminate fatty meats, fish, sausages, and fast food from your diet.
- Plant foods should predominate in the diet, and you should be careful with animal proteins.
- Any alcoholic drinks, coffee and strong tea are strictly prohibited.
- Instead of whole milk, it is advisable to drink low-fat kefir or yogurt without additives.
- Limit daily fluid intake to 1.5-2 liters, preventing increased stress on the kidneys.
Postoperative period
After surgery associated with organ transplantation, the patient must take lifelong medications that inhibit the lymphocytic activity of his own immunity. This is a very important point, since only by taking immunosuppressants can kidney transplant rejection be avoided. Rehabilitation after surgery takes from several months to 2-3 years, depending on the individual characteristics of the recipient’s body and the speed with which the kidney transplant takes root.
During the first week, the patient who has undergone a transplant is in the intensive care unit, where his health condition and basic vital signs are carefully monitored. Only after the attending physician is convinced of the engraftment and functioning of the transplant, the patient will be transferred to a regular department, where he will continue treatment.
Life after a kidney transplant is not easy, since, in addition to constantly taking specialized medications, the patient is placed on mandatory registration and must visit the transplant center once every 3 months to monitor his own condition and monitor how the transplanted graft behaves. The patient must constantly follow a diet after a kidney transplant. The nutrition of patients is aimed at reducing the load on the urinary system. The patient is prescribed a special diet after a kidney transplant, which includes foods that do not create a burden on the urinary system, including the donor kidney.
Kidney transplantation does not affect existing disability, since the patient remains on lifelong drug therapy, and his standard of living is undoubtedly lower than that of a healthy person. However, this operation can significantly prolong the life of a patient with diseases of the urinary system in the terminal phase.
Why the organ does not take root, signs of rejection
During the postoperative period, the patient is in the hospital under 24-hour medical supervision. To assess the functioning of the transplant, blood and urine tests for electrolytes, urea, creatinine are regularly performed, ultrasound and other instrumental diagnostics are performed to assess the quality of blood flow in the transplanted kidney.
There are several possible complications after a kidney transplant. The patient’s life may be under real threat, so it is important to recognize negative changes in the body as early as possible. Their cause may be:
- Unsatisfactory connection of blood vessels, which can cause bleeding. As a result, the patient develops hematomas in the retroperitoneal space.
- Inflammation and suppuration of the suture on the body after surgery. Therapy, which is carried out to minimize the risk of rejection, weakens the immune system, which can lead to wound infection.
- Thrombosis in the iliac arteries or deep veins of the legs.
- Rejection. It may appear suddenly (hyperacute) or during the first months after surgery. Sometimes rejection becomes chronic. In this case, it is a sluggish and unnoticeable reaction. Its occurrence is fraught with serious consequences. If immunosuppressants fail to correct the situation, the donor kidney will die.
Rejection of a new organ can be suspected based on a number of signs. Typically, patients complain of pain, swelling, increased body temperature and blood pressure, decreased frequency of urination, shortness of breath and general malaise. If such signs appear, the patient needs immediate medical attention. In case of acute rejection, the doctor will decide to increase the dose of the immunosuppressive drug or change it to a stronger one.
Dietary recommendations
After the critical period in which complications may develop after a kidney transplant has passed, the patient will need to strictly monitor his health. Compliance with a therapeutic diet is considered an important point that will provide the patient with a healthy and fulfilling life. The principles of a therapeutic diet in the postoperative period are based on the rules of a healthy lifestyle and nutrition. The patient needs to limit the consumption of simple carbohydrates, which do not bring any benefit to the body, while at the same time increasing the level of cholesterol and glucose in the blood. Such products include:
- bakery products made from premium flours;
- sweet desserts, milk chocolate;
- fatty meat, smoked meats;
- some types of porridges (semolina, wheat, millet).
If blood tests show an increase in cholesterol, you need to limit your intake of foods that contain a lot of fat. These are dairy products, fatty meats and fish, butter and vegetable oil, lard. It is advisable to avoid out-of-season vegetables and fruits, as they contain a lot of nitrates, which can cause kidney complications. In the postoperative period, you need to adhere to the drinking regime. You need to drink at least 1.5-2 liters of liquid per day, mostly clean drinking water. Drink store-bought juices and fruit drinks with caution. Alcoholic drinks, beer, sweet soda are strictly prohibited, and cigarettes must be given up.
Where is a kidney transplant performed?
Transplant operations are a type of high-tech medical care. In Russia, kidney transplants are performed by more than 40 medical organizations that have the appropriate license. It is worth noting that quotas from the federal budget are allocated for each region to perform free operations for patients in need, but, unfortunately, there are not enough government funds for all of them. On average, the cost of a kidney transplant is about 1 million rubles. Moreover, we are not talking about the price of a donor organ, since such trade is prohibited in Russia, but about the cost of surgical intervention, regardless of which organ will be transplanted - from a relative or from a deceased donor.
There are more medical centers in our country that provide kidney transplantation than clinics specializing in transplantation of other organs. The leading institutions in Moscow are:
- Federal Scientific Center for Transplantology and Artificial Organs.
- Russian Scientific Center for Surgery named after Academician B.V. Petrovsky of the Russian Academy of Medical Sciences.
- Oncological Research Center of the Russian Academy of Medical Sciences.
- Scientific Center for Cardiovascular Surgery named after A. N. Bakulev, Russian Academy of Medical Sciences.
- Medical and Surgical Center named after N. I. Pirogov.
- Russian Children's Clinical Hospital of Roszdrav.
- Military Medical Academy named after S. M. Kirov.
There are also transplantology departments in 23 regions and cities, including St. Petersburg, Novosibirsk, Voronezh, Nizhny Novgorod, Krasnoyarsk, Khabarovsk, Yekaterinburg. Information about the nearest kidney transplant medical center can be obtained from the territorial structures of the Ministry of Health. Patients also submit applications for quotas there.
Throughout his life after transplantation, the patient must constantly monitor his health and take medications to suppress the immune response - they will help prevent rejection. In addition, the patient should undergo periodic diagnostic procedures and lead a healthy lifestyle.
For the health of the person who took part in the transplant as a donor, the risks are less serious, however, in later life with one kidney there is still a chance of negative consequences.
Kidney transplant - a chance to start a new life
These young people were literally “chained” to an artificial kidney machine for many years; they had to go to the hospital two or three times a week for hemodialysis, a vital procedure for diseased kidneys. And now the “shackles” have been removed, each of them has been transplanted with a healthy kidney at the Republican Clinical Hospital (RCH) in Kazan. There is a new life and new plans ahead.
Since childhood, Arthur had pyelonephritis, which by the age of thirty became a serious problem; Dinara, a skier, was diagnosed with diseased kidneys when doctors diagnosed another disease. But Evgenia had a congenital kidney abnormality - glomerulonephritis, in which the kidneys gradually die and nothing can be done about it.
The medical histories of these three young people were different, but they had one thing in common - the belief that each of them would definitely get their kidney, and the doctors would do everything possible to ensure that the transplant was successful. And so it happened: Arthur received a related kidney, his mother gave it to him, Dinara and Evgenia waited for donor organs. Doctors, in turn, skillfully implanted them into their patients.
Since the beginning of this year, RCH specialists have performed 31 kidney transplants and have already exceeded the annual target. Funds for extra-planned operations in the amount of 11 million rubles were allocated to the hospital by the leadership of the republic as part of the state program for the development of healthcare in Tatarstan until 2014. This amount is enough to carry out 12 more such additional operations.
The cost of one kidney transplant operation, according to the Ministry of Health of Tatarstan, is about 923 thousand rubles. For residents of the republic it is carried out free of charge, within the framework of the state program. Currently, there are about 300 people on the official waiting list for surgery, while about 1.5 thousand are on hemodialysis and need an organ transplant.
“If they don’t get a kidney transplant, they will be chained to a hemodialysis machine all their lives, because some of them need this procedure every day. This is a salvation for such patients; without the artificial kidney apparatus, they would simply die. Today, there are hemodialysis departments in all municipalities of the republic,” Rafael Shavaliev, chief physician of the Republican Clinical Hospital (RCH), told reporters. It is difficult to depend on medical equipment all your life without being able to leave your hometown even for a few days. A kidney transplant for such patients is a chance for a normal, fulfilling life.
The trend towards an increase in the number of patients with chronic renal failure is steadily growing. “Every year the number of patients in need of dialysis, and, accordingly, a kidney transplant in the republic increases by approximately 100-120 people,” said Almaz Gainullov, head of the kidney transplant department of the Russian Clinical Hospital.
He explained that the two main types of dialysis are peritoneal dialysis and hemodialysis. Hemodialysis is carried out outside the body, peritoneal dialysis is carried out inside the body. Both types of dialysis are effective for treating chronic kidney failure. The choice between these two types depends on personal preferences and lifestyle, as well as the general clinical condition of the patient.
During its work, the department performed about 400 transplantations from deceased and living donors. Doctors consider the optimal option to transplant a kidney from living related donors: with such operations there are fewer complications and a greater chance that the organ will function normally. The survival rate of patients in the Republican Clinical Hospital after such an operation is one of the best in the country. In general, experts say that a kidney transplant can be done four times, if possible - once every ten years.
Selecting a donor organ for a patient, according to Ksenia Sitkina, a doctor at the kidney transplant department of the Russian Clinical Hospital, is a complex process that requires a lot of research. Thus, the most important condition for successful transplantation is the compatibility of recipient and donor tissues. This means that both parties must have compatible blood and tissue types, which reduces the risk of the donor kidney being rejected by the recipient's body. To check compatibility before surgery, a series of laboratory tests are performed.
After a donor kidney is found, the operation is performed as soon as possible. All data of future recipients is in a special registry, they regularly undergo tests, go for hemodialysis to maintain good body condition and know that they must be ready for surgery at any time.
However, even after the most successful transplant, the kidney will still not become their own; throughout the rest of their lives they will have to follow a special regime and take special medications - immunosuppressants in order to prevent rejection of someone else’s kidney.
It is clear that the earlier the disease is detected, the easier it is to treat. So, experts say that the earliest diagnosis of renal failure is laboratory tests, and not ultrasound, as many people think. An ultrasound determines only the shape and size of the kidney, and tests will show how it works. And doctors also advise that in order to recognize the disease in time, you need to regularly check the level of creatinine in the blood, but, unfortunately, today this test is not included in the list of tests during medical examination.
Today, specialists are ready to perform kidney transplant operations almost every day; the hospital has all the conditions for this, but there is not enough donor material. Doctors are not optimistic about solving this problem in the foreseeable future. The reason for this is our conservative mentality regarding the removal of organs and tissues for transplantation. Today, not everyone agrees to donate their organs to another after death, which means that someone will still have to languish in line for a long time, waiting for a suitable donor kidney, and someone, unfortunately, may not get one at all...