When a kidney ultrasound is prescribed, deciphering its results is of interest to many patients. Kidney diseases remain a pressing problem today. If you trust the data of medical statistics, then there are more and more people with this problem every year. Kidney pathology is considered an insidious disease and can affect a healthy kidney even in childhood, and then can manifest itself at the stage of renal failure. That is, when the disease can no longer be treated.
To examine the kidney, doctors often resort to ultrasound, as it is considered the most reliable and safe type of diagnosis. The patient does not feel any pain, and the best thing is that there are no contraindications for ultrasound examination. If kidney disease is detected early, the patient has a chance for a full recovery.
How to get to the kidneys
Due to the complex location of the kidneys, difficulties may arise with their diagnosis or diagnosis of blood vessels. After all, in order to see the renal vessels and their trunks, it is necessary to choose the optimal location for scanning. Due to the proximity of the intestine to the kidneys, imaging may be difficult. Therefore, in order to determine the best viewing and scanning location, it is necessary to regularly stir the ultrasound machine probe to select a suitable location. In other words, a polypositional research method is used, during which the position of the patient’s body changes to obtain an optimal projection of the organ.
In the study of the kidneys, the lateral position has proven itself very well. While the patient lies on one side, the specialist examines the other. Pressing with the sensor and adjusting the patient's breathing helps to achieve good results during the study.
Kidney stones on ultrasound
On ultrasound, a kidney stone is a hyperechoic structure with an acoustic shadow, more than 4 mm in size. An acoustic shadow is left only by oxalates larger than 8-10 mm, and even then not always. Tiny stones of the kidneys and ureters with CDK give a flickering artifact behind. There is an opinion that one can see accumulations of uric acid salts in the form of a diffuse accumulation of point signals of high echogenicity along the contour of the renal papillae.
Drawing. Ultrasound shows a normal kidney. In the lower pole there is a small hyperechoic inclusion without an acoustic shadow (1, 3); CDC flickering artifact (2). Conclusion: Small calculus in the small calyx of the lower pole of the left kidney. Confirmed on CT scan.
Drawing. A patient complains of discomfort when urinating. On ultrasound, the right kidney is located in the pelvis, the vascular bundle is from the iliac vessels (1); in the pelvis there is a hyperechoic inclusion with an acoustic shadow behind, size 10x10 mm (3, 4). Conclusion: Pelvic dystopia of the right kidney. Echo signs of a stone in the pelvis on the right. On X-ray (4) there is a round radiopaque inclusion in the midline above the S1 vertebra.
Drawing. A patient with urolithiasis was admitted with acute pain in the left lower back. On X-ray (1) the borders of the right kidney are enlarged, radiopaque stones are in both kidneys (triangles). On ultrasound (2, 3) in the right kidney, a lenticular avascular hypoechoic formation with a heterogeneous echostructure compresses the parenchyma; in the area of the CLK there is a hyperechoic focus with a dorsal shadow (triangle), with CDK there is a flickering artifact. Conclusion: Subcapsular hematoma of the right kidney. A stone in the maxillofacial area on the right, without signs of obstruction. CT scan shows a subcapsular hematoma and a calculus in the pelvis in the right kidney; in the left kidney there is a calculus in the ureter and secondary hydronephrosis of 2-3 degrees.
Drawing. When the renal pelvis and calyces are filled with a dense calcified mass, the stone is shaped like coral. On ultrasound (1) there is a coral stone in the kidney with a massive acoustic shadow behind it, one of the upper calyces is dilated.
Drawing. Ultrasound (1) in the right kidney reveals a rounded cavity with an anechoic and hyperechoic component, which change shape when the patient turns. X-ray in the supine position (2) shows a rounded radiopaque formation in the upper pole of the right kidney; in a standing position (3) the radiopaque level is visible. Conclusion: Kidney cyst with calcium milk. Most often, calcium milk accumulates in simple parenchymal cysts or diverticula of the calyx. If the cyst is completely filled, diagnosis is problematic.
Drawing . In 37% of healthy newborns, on the first day of life, ultrasound reveals hyperechoic pyramids without an acoustic shadow. Precipitation of Tamm-Horsfall protein and uric acid causes reversible tubular obstruction. By 6 weeks of life it goes away without treatment.
Drawing. A patient complains of lower back pain. Ultrasound shows hyperechoic pyramids in both kidneys without a dorsal acoustic shadow; in the upper pole of the right kidney there is a hyperechoic round formation with an acoustic shadow, size 20 mm. Conclusion: Medullary nephrocalcinosis. A calculus in the upper calyx of the right kidney. An acoustic shadow behind hyperechoic pyramids is seen in extreme cases of medullary hypercalcinosis. Causes of medullary nephrocalcinosis: parathyroidism - 40% of cases, tubular tubular acidosis (distal type 1) - 20%, medullary spongy kidney - 20%.
Kidney standards
The kidney of adults has certain standards; minor deviations are possible, which will be considered normal. If these deviations are significant, then we can talk about pathological changes that occur in the kidneys.
The length of the kidney ranges from 10 to 12 cm, width from 5.0 to 6.0 cm, and thickness from 4.0 to 5.0 cm. The kidney parenchyma has a thickness of 1.5 - 2.5 cm. It tends to thin out, this change directly depends on age. The older a person is, the lower the density of the parenchyma. In persons over 61 years of age, it can reach 1 cm.
Hydronephrosis on ultrasound
The ureter, minor and major calyces are normally not visible on ultrasound. There are three types of pelvis location: intrarenal, extrarenal and mixed type. With an intrarenal structure, the lumen of the pelvis at an early age is up to 3 mm, at 4-5 years - up to 5 mm, in puberty and in adults - up to 7 mm. For extrarenal and mixed types of structure - 6, 10 and 14 mm, respectively. When the bladder is full, the pelvis can increase to 18 mm, but 30 minutes after urination it contracts.
When the outflow of urine is disrupted, the pelvis and ureter above the obstruction expand. If the pelvis is dilated, this is pyelectasis; the calyces are dilated along with the pelvis - hydronephrosis; in addition, the ureter is dilated - ureteropyeloectasia or ureterohydronephrosis. The outcome of hydronephrosis is always the death of nephrons and atrophy of the kidney parenchyma.
In men, hydronephrosis develops with prostate tumors; in women, it is more often associated with pregnancy and pelvic tumors. Common causes of hydronephrosis in children are congenital stenosis or segmental dysplasia of the ureter, horseshoe kidney, malformed ureter or accessory vessel. Hydronephrosis can develop due to vesicoureteral reflux or increased diuresis after taking diuretics.
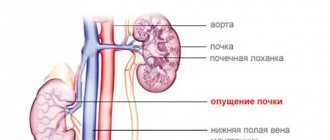
Kidney location
The kidney itself is located in the inner part of the capsule; during an ultrasound examination, it will be displayed as a super-dense line passing along the border of the perirenal fat and the cortex. As a rule, if the kidney is healthy, it has a smooth surface, but a wavy contour may be present. Provided that the embryonic lobulation of the parenchyma is preserved.
The device can distinguish the density of the renal sinus or the parenchyma that surrounds it. In which the presence of medulla and cortex may be observed.
The density of the cortex is slightly less than the liver or spleen. If normal, there may be cortico-medullary differentiation. The density of the pyramid tissue will be lower than the density of the cortex itself, especially in young people. They appear as separate triangular-shaped structures with reduced tissue density, which are located towards the cortex.
When using the ultrasound method with an iodine-containing substance, if the blood flow of the vessels is normal and not disturbed, the development of deviations at this site is excluded.
To evaluate the structure, the ratio of parenchyma size to central density is calculated. This process in medicine is called the parenchymo-pyelic index. Normally, this index should be two to one.
Indications for ultrasound examination of the kidneys
It is advisable for all people to undergo such diagnostics once a year, even if nothing bothers you.
An unscheduled ultrasound examination is carried out in the following cases:
- Pain in the lumbar part of the body.
- If, as a result of a urine test, elevated or decreased values are found.
- When a person experiences urinary incontinence.
- Attacks of renal colic.
- The person has no urinary function.
- Pain occurs during urination.
- When the doctor has suspicions about formations in the organ.
- The presence of an inflammatory process in the lower part of the body.
- If there is an inflammatory process of the genital organs.
- After receiving injuries in the lower back.
- When the color of urine changes.
- If your kidney becomes a donor.
- If you are registered for kidney disease.
- During preventive examinations.
- A comprehensive examination can be performed when the patient is referred for another type of disease.
Age-related changes
With age, the body undergoes a number of changes that cannot affect the functional abilities of the organs. Due to chronic arterial disease, which arises from a disorder of lipid metabolism and is accompanied by the deposition of cholesterol plaques along the inner wall of the vessels, changes in the parenchyma can be provoked. An irreversible process of thinning may occur. This can also occur due to the development of inflammatory diseases.
If the patient experiences an increase in urine at the time of the ultrasound examination, this will help to more clearly visualize the collecting system. Therefore, the patient may be advised to undergo an ultrasound examination of a full bladder to obtain accurate information.
Editor
Update date: 07/21/2018, next update date: 07/21/2021
If you find an error, please select a piece of text and press Ctrl+Enter.
When a kidney ultrasound is prescribed, deciphering its results is of interest to many patients. Kidney diseases remain a pressing problem today. If you trust the data of medical statistics, then there are more and more people with this problem every year. Kidney pathology is considered an insidious disease and can affect a healthy kidney even in childhood, and then can manifest itself at the stage of renal failure. That is, when the disease can no longer be treated.
To examine the kidney, doctors often resort to ultrasound, as it is considered the most reliable and safe type of diagnosis. The patient does not feel any pain, and the best thing is that there are no contraindications for ultrasound examination. If kidney disease is detected early, the patient has a chance for a full recovery.
In just half an hour, the doctor will be able to evaluate the organ visually: study its structure, echogenicity, and find out whether there are any deviations from the norm.
This procedure will allow you to diagnose the presence of tumors, cysts, and changes in the size of the kidney.
You need to remember that if your doctor has referred you to this method of examination, then you need to go, since thanks to it you can establish or suspect diseases such as pyelonephritis, glomerulonephritis, hydronephrosis, polycystic kidney disease, amyloidosis and others.
Kidney cysts on ultrasound
Simple renal cysts on ultrasound are anechoic avascular round formations with a smooth thin capsule and increased signal behind. 50% of people over 50 have a simple kidney cyst.
Complex cysts are often irregular in shape, with internal septations and calcifications. If the cyst has an uneven and even bumpy contour, thick septa, and a tissue component, then the risk of malignant neoplasms is 85%-100%.
Drawing. Classification of renal cysts according to Bosniak. Types 1 and 2 cysts are benign and do not require further evaluation. Cysts types 2F, 3 and 4 require additional research.
Drawing. Ultrasound shows simple (1, 2) and complex (3) kidney cysts. In the absence of urine output, the parenchyma symmetrically moves apart in all directions, forming round parenchymal cysts. Parenchymal cysts will not disappear anywhere, they can only rupture.
Drawing. Ultrasound (1) shows an anechoic round formation in the right kidney, with a clear and even contour, and a hyperechoic tissue inclusion in the wall. Conclusion: Kidney cyst type 2F according to Bosniak. According to the results of the biopsy, renal cell carcinoma.
In polycystic kidney disease, multiple cysts of varying sizes fill almost the entire kidney. In later stages of the disease, the kidneys are enlarged and there is no corticomedullary differentiation. For more details, see Polycystic kidney disease on ultrasound.
Drawing. Ultrasound (1, 2) and CT (2) show multiple cysts in both kidneys. This is an autosomal dominant polycystic kidney disease.
Pathologies detected by ultrasound examination
Ultrasound can reveal signs of many kidney abnormalities and diseases in children. We will briefly consider the typical echographic signs of the most common detected pathologies and the terms used in this case, which the ultrasound doctor can add to the conclusion. In children, various developmental options may occur: an additional kidney, an intrarenal septum, a hypertrophied renal column or Bertin's column. All of them are anatomical features of a particular child and do not pose any danger to his health.
Extra kidney
An additional kidney is defined as a formation similar in shape and structure to a normal kidney, but significantly smaller in size. In this case, the doctor carries out a differential diagnosis with a tumor.
Connective tissue defect
A connective tissue defect or intrarenal septum in the renal parenchyma is defined by ultrasound as a hyperechoic (white) formation of a triangular or round shape, extending from the anterosuperior or posteroinferior surface of the kidney, or as a thin hyperechoic linear signal from the surface of the kidney to its hilum. These structures are three times more likely to be detected in the right kidney and can be mistaken for a scar, the presence of which makes one think about the consequences of injury or the process of shrinkage.
Hypertrophied renal column of Bertin
The hypertrophied renal column of Bertin, as a rule, is detected in the center of the kidney and has the appearance of a homogeneous formation of a triangular or round shape with clear boundaries, the echogenicity of which exceeds the echogenicity of the surrounding tissue. A hypertrophied column can be mistaken for a tumor. A Doppler study reveals the vessels wrapping around this area.
Frehley syndrome
Another development option is considered to be an expansion of the upper calyx, not exceeding 8 mm - Frehley syndrome , which occurs as a result of the abnormal location of the vessel, pinching the neck of the calyx and making it difficult to pass urine. In this case, an expanded upper calyx is detected on echograms.
Wandering kidney
If the fixing apparatus is weak, the kidneys may become displaced (“wandering kidney”). During inspiration, the displacement of the kidneys in young children is on average 1 cm, in older children from 1.5 to 2 cm. In a standing position, the normal descent of the kidney is up to 1.8% of the child’s height. Displacement ranging from 1.8% to 3% is regarded as excessive mobility, and more than 3% - as nephroptosis.
In case of developmental anomalies, ultrasound of the kidneys is not always fully informative. The absence of a kidney in a typical location may be due to agenesis (complete absence of an embryonic organ rudiment), aplasia (embryonically damaged but detectable non-functioning kidney rudiment), dystopia (displacement of an organ to an atypical location), anomaly of fusion and requires additional radiological research methods.
Doubling
Various types of kidney duplication are the most common form of congenital pathology. It is not always possible to notice two collecting complexes during ultrasound examination. The first sign of doubling is different lengths of the buds. Lack of symmetry, a difference in length of more than 5 mm is most often due to doubling of the larger kidney. Size asymmetry can also be caused by another pathology - hypoplasia, wrinkling of one of the kidneys and, accordingly, vicarious enlargement of the other. The final answer is established after excretory urography.
Pyelonephritis and abscess
Unlike adults, acute pyelonephritis in children is almost always reliably visible on ultrasound. It is characterized by thickening of the walls of the pelvis against the background of blurred or loss of cortico-medullary differentiation in the form of unclear or lack of visualization of the pyramids. With it, expansion of the pyelocaliceal system may be observed.
An abscess in the kidney looks like an irregularly rounded area with uneven, fuzzy contours and a hypoechoic center.
Chronic atrophic pyelonephritis is echographically represented by fragmented thinning of the parenchyma, a decrease in the size of the kidney, and a slight expansion of the pyelocaliceal system. The contours of the kidney become uneven, and retractions may appear.
Nephrosclerosis
Nephrosclerosis or “shrunken kidney” is the final stage of almost any kidney damage and leads to chronic renal failure. In this case, the kidney is significantly reduced in size, the echogenicity of the parenchyma is increased, and cortico-medullary differentiation is not determined.
Stones and concretions
The formation of stones and concretions in the kidneys occurs even in infants. The calculus is described as a hyperechoic structure that produces a distinct acoustic shadow.
Cysts
Kidney cysts come in a wide variety of forms. Most often they look like anechoic structures (completely black) of a round shape with clear, even contours, with distal acoustic enhancement. If many small cysts are detected, then this may be a manifestation of “adult-type” polycystic disease, which is often combined with cysts in the liver and pancreas.
Juvenile type polycystic disease may be detected in infants . With it, the entire renal parenchyma is thickened and represented by a collection of small cystic inclusions with the formation of a “spongy” structure.
Glomerulonephritis
Acute glomerulonephritis on ultrasound is manifested by an increase in the size of the kidney, increased echogenicity of the parenchyma, and blurred pattern of pyramids. But these signs can also be observed in other diseases, so it is impossible to clearly establish the diagnosis of glomerulonephritis only with the help of ultrasound.
Injuries and tumors
Kidney injuries are often clearly visible using ultrasound. Small tears are defined as hypoechoic or anechoic areas against the background of increased echogenicity of the parenchyma. After healing, a scar forms in this area.
More severe injuries are characterized by an unclear contour of the organ, accumulation of heterogeneous contents around, decreased corticomedullary differentiation and zones of reduced echogenicity in the renal parenchyma.
Kidney tumors in children are rare and do not have clear ultrasound signs. They can be very different in their structure and echogenicity. In this case, ultrasound is used only as a screening method for identifying them, and further diagnosis is carried out using CT or MRI, as well as biopsy.
Hydronephrotic pathology
In a newborn child, a sharp dilation of the pelvis and calyces (hydronephrotic pathology) can be caused by malformations of any part of the urinary system, which leads to disruption of the outflow of urine from the kidneys. The cause of obstruction leading to such a pathology can also be a stone, a tumor, the consequences of severe inflammation, trauma, or vesicoureteral reflux. Ultrasound diagnosis of PMR is possible when urine is thrown up to the pelvis (stage 3–4 of the process).
Clinical characteristics
The first symptoms in most patients appear in the neonatal period.
Kidneys On examination: enlargement of the right and left lateral areas of the abdomen, where space-occupying formations are palpated. The volume of urine excreted is usually reduced, although polyuria and polydipsia may occur if the concentration function of the kidneys is impaired. Severe forms with the development of acute renal failure (ARF) will be manifested by oliguria, hyponatremia, an increase in creatinine and urea nitrogen in the blood. But with age, due to the development of normal renal tissue, renal function improves and the manifestations of acute renal failure decrease. Despite this, in approximately 50% of those affected, the disease progresses to end-stage renal failure in the first decade of life. Symptoms of severe arterial hypertension, which debuts from the first days, also become less severe over time.
Liver With the development of methods of replacement therapy for kidney function and transplantation, long-term survival of patients is improving. Due to this, hepatobiliary clinical manifestations become the main problem of older age groups. Congenital liver fibrosis leads to progressive portal hypertension, which is manifested by varices of the esophagus, stomach, hemorrhoidal veins, hepatosplenomegaly, protein-losing enteropathy and gastrointestinal bleeding.
Caroli syndrome is a non-obstructive dilatation of the intrahepatic bile ducts and common bile duct, occurring in more than 60% of cases of PCB-AR. Insufficient drainage function of the biliary system predisposes to the development of bacterial ascending cholangitis and sepsis. Malabsorption due to cholestasis leads to a deficiency of fat-soluble vitamins (A, D, E and K). In adult patients, biliary hyperplasia predisposes to the development of benign and malignant tumors.
RENAL CYSTADENOMA (Perelman tumor)
Renal cystadenoma (multilocular cystic nephroma) is a benign intracapsular tumor in the form of multiple myxomatous cysts.
Boys (<4 years) and older women (50-70 years)
MR - signs
MRI without contrast enhancement:
- Encapsulated multilocular cystic formation
- Sizes from 3 to 30 cm
- Myxomatous fluid (protein fluid)
- Thick fibrous septa
MRI with contrast:
- The tumor capsule accumulates CV more often
- Thin partitions more often moderately accumulate CV
- The lumen of the cysts does not communicate with the kidney PC
- Sometimes deforms the maxillofacial joint with obstruction
Features of the results in a newborn
The perception of kidney ultrasound results in newborns has its own characteristics, because they retain the features of an incomplete kidney structure.
In newborn children, the kidneys are located lower than in older children, and almost parallel to the spine, and then gradually rise higher to the diaphragm and come together at the upper poles.
The outline of the kidneys in newborns is usually lumpy because they have a lobular structure. It can last up to 2 years, and according to some sources, up to 5 years.
In children under 6 months of age, the echogenicity of the cortical layer of the parenchyma is higher than in older children, and exceeds the echogenicity of the liver and spleen.
In a newborn, the echographic sign of “white pyramids” may be detected, manifested by the hyperechogenicity of several pyramids in the renal parenchyma. It is defined as the norm for up to 1-2 months. The collecting system on echograms, if it is not expanded, is not visible in newborns and children under 6 months of life
Features of the violation
Lymphadenopathy is accompanied by chest pain, shortness of breath and difficulty breathing
Hilar lymphadenopathy is an enlargement of the mediastinal nodes. The mediastinum is the space between the heart and the bronchi (middle part of the chest). This area contains many lymph nodes, which can enlarge under the influence of various factors.
According to ICD-10, lymphadenopathy is designated by code R59. In this case, the disorder is not classified according to the location of the enlarged nodes.
Hilar lymphadenopathy is characterized by a number of symptoms that make it possible to quickly differentiate this disorder. Moreover, the symptoms depend on the location of the affected nodes. In general, enlarged lymph nodes in the thoracic region are considered as a single disorder, but the following types of pathology are distinguished:
- pulmonary lymphadenopathy;
- mediastinal lymphadenopathy;
- supraclavicular, or paratracheal, lymphadenopathy.
Pulmonary lymphadenopathy (also called bronchopulmonary lymphadenopathy) is often of a tumor nature. This is a very dangerous symptom that requires timely treatment to the clinic.
Mediastinal lymphadenopathy, which affects the mediastinum, is a general term that describes enlargement of any lymph nodes in the chest. The paratracheal form of the disease is an enlargement of the nodes located along the wall of the trachea, which are also called supraclavicular.
Pathological anatomy
Macroscopic structure
The fetus has a characteristic appearance (Potter's face): narrow eyelid slits, a characteristic groove under the eyelid line, micrognathia, a flattened nose, soft large ears of an abnormal shape. The kidneys are increased in size, while maintaining their bean-shaped shape, but cannot perform their function. Poorly functioning kidneys do not produce enough fetal urine, leading to oligohydramnios and pulmonary hypoplasia. The hydrostatic pressure of the amniotic fluid ensures the normal development of the respiratory system.
Figure 1 | Fetus, 23 weeks. Fetal death after premature birth was due to pulmonary hypoplasia, caused by oligohydramnios due to PBP. Enlargement of both kidneys with displacement of the abdominal organs in combination with lung hypoplasia.
Figure 2 | Longitudinal section of a kidney with PCB.
Microscopy
Kidneys Radially oriented dilated collecting ducts form renal cysts with a diameter of 1–2 mm, between which normal glomeruli and tubules are visible.
The size of cysts can vary depending on age. In the early stages, the disease begins with microcysts, which then grow and turn into macrocysts. Cystic kidney disease is accompanied by slight interstitial fibrosis of the renal parenchyma.
Figure 3 | Microscopic specimen of a kidney from a patient with PBC-AR. Twenty-fold magnification, hematoxylin-eosin staining. ✱ — radial renal cysts; ▼—renal capsule. Arrows indicate normal glomeruli between dilated collecting ducts.
Liver Histological changes in the liver include the following malformations of the ductal plate: biliary hyperplasia, biliary ectasia and periportal fibrosis.
Disturbances in the morphogenesis of the development of the bile ducts lead to their dilatation. With subsequent progression of the disease, the dilated ducts turn into macrocysts connected by normal ducts, which allows them to be verified quite well using MRCP.
Figure 4 | Pathological changes in the liver. a) The structure of the normally branched portovenous and ethmoidal systems of the biliary tract (left) is disrupted due to a defect in the development of the ductal plate and errors in the terminal differentiation of cholangiocytes (right); b) Coronal T2-weighted image of the abdominal cavity: - the arrow indicates a cystic fusiform dilatation of the bile ducts; — arrow like an arrowhead — nephromegaly with small cysts; ✱ — splenomegaly. c) Preparation of a liver fragment, hematoxylin-eosin staining, 40x magnification:
✱ — extensive fibrosis of the portal area;
arrow - dilated tortuous bile ducts; arrowhead type arrow —hypoplasia of tributaries of the portal vein.
Encyclopedia of Ultrasound and MRI
Currently, ultrasound of the kidneys in children is the most frequently prescribed instrumental method for diagnosing the pathology of this area. It has many advantages, including non-invasiveness, painlessness, speed, fairly high accuracy, and relatively low cost. This method has wide application not only in the presence of symptoms of kidney diseases, but also as the first method for detecting congenital anomalies and kidney diseases in a child.
How are the results interpreted?
How is kidney ultrasound interpreted? Many people have probably done different diagnostic options, and everyone knows that after the procedure, the patient is given a sheet with many incomprehensible words written and a conclusion at the end. True, not everyone is happy with this option, because they want to know what exactly is written there.
Number of kidneys. All healthy people have two. But, however, such an indicator cannot always be found, since many live their whole lives with one and do not even know about it. A kidney is an organ that may be absent from birth or may be underdeveloped. It cannot be ruled out that it can be removed surgically. But there are also unique people who have more than two. Such kidney abnormalities sometimes occur, but often the additional organs do not function.
Kidney size and contour. In an adult healthy person, the organ has the following parameters: length 10-12 cm, width 5-6 cm, thickness 4-5 cm. If you were written in the conclusion that the organ is different in size, then you need to start looking for the cause of this phenomenon. If you are diagnosed with “chronic glomerulonephritis,” then in this case the kidney loses its size. And during hydronephrosis, on the contrary, it increases in size. The norm is when the contour of the organ is smooth.
Location. In the normal state, the right kidney is located at the level of 12 and 2 lumbar vertebrae, and the left one - at 11 and 1. There are cases when the organ descends or, conversely, is located far from its usual location. There are situations when the kidney is in the pelvis.
Parenchyma thickness. This part of the organ is responsible for the formation of urine, being a functional component of the kidney. The parenchyma contains nephrons, which are responsible for its structural formation. In normal condition, its thickness is 18-25 mm. If there is an increase in it, this indicates an inflammatory process or swelling, and a decrease, on the contrary, indicates a dystrophic change in the organ.
Cortico-medullary differentiation is also important. In a normal state, its boundaries are clearly visible. An example is a case where a patient is diagnosed with hydronephrosis, and the differentiation disappears.
The structure of the parenchyma is an important indicator of the condition of the kidney. In order to understand whether there are changes in it, you need to know what increased, normal or decreased echogenicity is.
Ultrasound can be performed in multidisciplinary city hospitals or special medical institutions. A similar procedure is carried out in private clinics; there is also such a service as calling a sonologist to your home with portable equipment.
In the Moscow region, on average, an ultrasound examination of the kidneys ranges from 600 to 1200 rubles, but if additional examination of the urinary system is required, the price reaches 1500 rubles. A house call before 6 pm will cost 3,000 rubles, and the cost of payment reaches 4,000-5,000 rubles. Prices are current for 2015.
Modern medicine offers a fairly convenient method for diagnosing the organs of the urinary system - ultrasound diagnostics. With its help, the cortico-medullary differentiation of the kidneys is also assessed.
Today there are practically no people left who have not at least once tried the principle of operation of ultrasound equipment in a doctor’s office. The method is safe and quite reliable. With its help, you can identify a number of dangerous pathologies.
During the study, attention must be paid to corticomedullary differentiation (CMD). This is a drawing of two kidneys - medullary and cortical. This zone occupies ⅔ of the entire renal pattern.
If a person has complaints about any pathologies of the urinary system, then he is prescribed an ultrasound. To get the correct picture, a person must lie down so that the specialist can examine the kidneys in detail.
Therefore, the doctor will ask the patient to change the position of the body until he finds one with a sufficiently good view. Usually they stop at the lateral position, since this way the vessels and each side of the kidney are accessible.
Diseases in which CMD does not change
There are pathologies of the kidneys and urinary system when the boundaries of cortico-medullary differentiation do not change. These include:
- Nephritis (damage to kidney tissue)
- Allergic vasculitis (manifested against the background of an infectious lesion, intoxication of the body, taking medications with pronounced side effects)
- Leukemia.
- Acute tubular necrosis.
- Chronic glomerulonephritis.
- Renal vein thrombosis (unilateral and bilateral)
- Blocked kidney tubules and kidney failure.
- Kidney damage after lupus erythematosus.