We perform ultrasound scanning of the renal arteries ( duplex scanning of the renal arteries ) and guarantee the accuracy of the results. The procedure takes place without pain or discomfort. We use a Japanese ultrasound scanner Mindray DC-8.
The duration of the procedure is ten minutes. The results are deciphered five minutes after the end of the study. We print the photo on film.
Currently, work is underway on the website to change the price list; for current information, please call: 640-55-25 or leave a request, and an operator will contact you.
Prices for servicesServices
The information and prices presented on the website are for reference only and do not constitute a public offer.
Kinds
Dynamic renal scintigraphy (DS) - a scan of the kidneys is performed after the administration of a radiopharmaceutical at certain time intervals, recording its entry into the kidneys and passage through the ureters into the bladder. The DS images show the entire process of urine formation and excretion in stages, which makes it possible to most thoroughly study the performance of both kidneys as a whole and each one separately.
Static scintigraphy (SS), an additional research method after radiography, records the general condition of the kidneys, size, shape and their location. SS does not inform about functional disorders of the urinary organs, so it cannot provide a complete picture of the disease.
What is it and how does it work
The full name of kidney ultrasound is duplex Doppler ultrasound. The principle of the study is based on the Doppler effect: ultrasonic waves are reflected from red blood cells and allow you to see the vessels from the inside in action.
The difference between duplex ultrasound and conventional ultrasound is that a standard black-and-white image and images of vessels with moving blood are simultaneously displayed on the doctor’s monitor.
Duplex Doppler examination of the kidneys shows disturbances in the volume and speed of blood flow, the condition of the walls and lumens of blood vessels.
In addition to diagnosis, ultrasound of the renal vessels is used to assess the progress of treatment.
Indications for renal scintigraphy
Dynamic nephroscintigraphy in urology is used more often than static one, because this method is more informative.
Dynamic renal scintigraphy is prescribed in the following cases:
- disturbances or changes in renal function of varying severity;
- hydronephrosis (stages 2 and 3) – expansion of the renal pelvis and calyces as a result of impaired urine outflow;
- anomalies in the structure and development of the kidneys;
- cysts and neoplasms (to determine the degree of malignancy);
- when planning an operation to remove one kidney (nephrectomy) to assess the condition of the second (presence of renal failure);
- examination of the only kidney before organ-preserving surgery;
- diagnosis for suspected metastases in the organs of the urinary system.
Indications for static nephroscintigraphy are:
- violation of the anatomical and topographic location of the kidneys;
- malformations of the urinary organs;
- pyelonephritis and other kidney pathologies.
Interpretation of indicators: norms for blood vessels and blood flow
When scanning the kidney vessels, the doctor should evaluate the following indicators:
- Artery diameter. Normally, for the main trunk it should be 3.3-5.6 mm, for segmental arteries - 1.9-2.3 mm, for interlobar arteries - 1.4-1.6 mm, for arcuate arteries - 0.9- 1.2 mm.
- Systolic velocity of blood flow in the renal arteries. Normally, for the main trunk it should be 47-99 cm/sec., for interlobar arteries – 29-35 cm/sec.
- Diastolic blood flow velocity in the renal arteries. Normally, for the main trunk it should be 36-38 cm/sec, for interlobar arteries – 9-17 cm/sec.
The doctor also evaluates other indicators of the condition of the kidneys: shape and size, clarity of contours, location, and so on.
Contraindications
Despite the fact that scintigraphy is considered a relatively safe procedure, there are situations in which it is recommended not to perform it at all or to postpone the examination for some time.
The patient's condition is assessed by doctors as serious - for such patients, the duration of the procedure from 45 minutes to 1.5 hours can be tedious;
Pregnancy - radiopharmaceuticals can have a negative effect on the intrauterine development of the fetus. Scintigraphy for expectant mothers is performed only in emergency cases;
Breastfeeding period - radiopharmaceuticals are removed from the human body within 24 hours after the examination. At this time, it is necessary to wean the child from the breast, replacing mother's milk with formula;
Cancer patients after a course of chemotherapy or radiotherapy - before scintigraphy, it is necessary to pause for a period of 3 weeks (after “chemo”) and 2-3 months (after irradiation).
Preparing for diagnosis
Doppler sonography is a non-invasive procedure. It is carried out by placing a sensor on the patient’s body in the projection areas of the kidneys. Ultrasound, before reaching the area under study, overcomes the resistance of other tissues, especially the intestines.
If there is increased gas formation in the intestines, this will interfere with obtaining accurate test results. Therefore, before the procedure, a number of measures are taken to reduce fermentation processes in the intestines.
Limit intake of foods that cause increased gas formation:
- fresh vegetables and fruits;
- for better absorption, consume food in small portions every 3-4 hours;
- water regime – up to 2 liters of water per day.
Prohibited:
- fatty meats and fish;
- dairy products;
- juices, kvass, beer, carbonated drinks;
- legumes: beans, peas, soybeans;
- rye bread and yeast baked goods;
- nuts, seeds;
- alcoholic drinks.
Allowed:
- boiled chicken;
- porridge with water;
- boiled eggs;
- dried bread, crackers, biscuits.
For constipation for more than 2 days - cleansing enemas the night before or laxatives.
The last meal is a light dinner before bed.
To reduce gas formation in the intestines, enterosorbents are prescribed 2 days before the procedure: Enterosgel, Polysorb .
It is advisable to undergo the test in the morning on an empty stomach. If for some reason it is not possible to do Doppler ultrasound in the morning, then the minimum interval after the last meal before the procedure should be at least 6 hours.
It is impossible to perform an ultrasound scan of the kidney vessels on the same day after other instrumental methods of examining the digestive tract: fibrogastroendoscopy, colonoscopy, since air entering the intestines during these manipulations will distort the results.
Methodology
Renal scintigraphy is performed on an outpatient basis in a specially equipped diagnostic room. The patient is asked to remove all metal objects from the area being examined. The nurse then administers an intravenous injection of radiopharmaceutical.
After the injection, the scanning process begins. At this time, the patient is in a separate room on the diagnostic table of the gamma tomograph, and the medical staff monitors the progress of the procedure from the adjacent room.
You cannot move or talk during the examination. Failure to do so may affect the quality of the images. Sometimes the doctor may ask the patient to change his body position. This is the moment when you should inform the doctor about a deterioration in your health (heaviness, palpitations, dizziness, shortness of breath, etc.), if this occurs.
Depending on the purpose of the examination, the patient is additionally administered medications before or during the procedure: antihypertensive drugs to diagnose patients with hypertension and diuretics to identify mechanical obstructions in the ureters.
Photo: D. Milosevic, E. Bilic, D. Batinic, M. Poropat, R. Stern-Padovan, S. Galic and D. Turudić - (December 17, 2014). Renal thromboembolism during treatment with recombinant activated factor VII (rFVIIa) in a child with hemophilia B with factor IX inhibitors
The essence of the method
Like ultrasound in general, duplex scanning is based on the varying ability of human body tissues to reflect ultrasound waves.
This study includes two mandatory components:
- B-mode (vascular scanning);
- Dopplerography.
B-mode is the so-called “conventional” ultrasound, that is, two-dimensional gray scale echography. The ultrasonic waves generated in the device’s sensor are recorded and directed to the area under study.
The doctor sees a black and white image on the screen
Important! Different anatomical structures have different densities and abilities to absorb and reflect ultrasound.
The reflected signal is perceived by the sensor, and based on the data received, the device builds a two-dimensional black and white image, in which the vessels and surrounding tissues are clearly visible.
The Doppler mode is an additional dynamic study that allows real-time assessment of blood flow parameters. It is based on the Doppler effect - a change in the wavelength of radiation that the sensor reads from a moving object - blood running through the vessels.
The cartogram is encoded as follows:
- red shades – the speed of blood flow moving towards the sensor;
- blue shades – the speed of blood flow moving in the direction from the sensor.
Arterial and venous vessels are clearly visible
Note! The more saturated the color of the image, the higher the speed.
Thus, duplex scanning of the kidneys is a diagnostic method that determines:
- indicators of blood flow in the renal arteries: direction, speed, linearity, uniformity;
- geometry of the vascular lumen;
- tortuosity of the riverbed;
- the presence of congenital or acquired anomalies;
- wall thickness;
- the presence of pathological formations in blood vessels (thrombi, atherosclerotic plaques, etc.).
Note! With duplex scanning, a visual assessment of the distribution of blood flow between the right and left kidney is performed. Speed characteristics and coefficients are also compared with the data of the opposite party.
Safety of nephroscintigraphy
Any diagnostic procedures related to nuclear medicine are safe for human health in general. Side effects after administration of radiopharmaceuticals are very rare, unlike contrast agents used in radiography or computed tomography.
Radiopharmaceuticals have a short-term effect; within 24 hours they disintegrate and are completely eliminated from the body, without having a negative effect on the functioning of internal organs and systems. To speed up this process, experts recommend drinking more fluids on the first day after scintigraphy.
Nephroscintigraphy carries such a minimal radiation dose that it makes it possible to conduct examinations almost daily. At the same time, radionuclide diagnostics is a highly informative method that detects abnormal changes in the kidneys 1-1.5 years earlier than conventional radiography.
The only drawback of scintigraphy is its inaccessibility. Not all private medical centers, let alone public clinics, can afford to purchase expensive equipment.
Benefits of Sonography
Non-invasive (no needle or injection)
To conduct an ultrasound scan, it is not necessary to make punctures or incisions on the patient’s skin. There is also no need to use a contrast agent to improve visualization.
Get results quickly
Recording of results and assessment of blood flow in the renal vessels are carried out during the examination. After completing the examination, the patient receives the results with a transcript.
Allows you to identify pathology at the time of examination
At the time of examination, ultrasound makes it possible to make accurate diagnoses. It is important how correctly the patient prepared for the procedure. Also, of course, the technical capabilities of the ultrasound machine and the qualifications of the doctor are important.
Mechanism of occurrence
Pathological polyuria is observed when adaptation mechanisms break down. In clinical practice, a combination with polydipsia (extreme thirst) is known. It is caused by hormonal changes and is manifested by increased fluid intake. The syndrome is considered polyetiological and is called the state of “polyuria-polydipsia.”
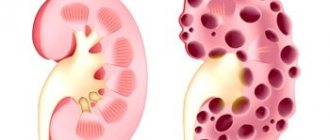
By origin, increased diuresis is conventionally divided into: renal (renal) and extrarenal (extrarenal). Renal - the main causes are located directly in the kidneys, observed:
- with congenital and acquired pathological changes in the tubules;
- in the initial stage of chronic renal failure (chronic renal failure);
- during the recovery period in acute kidney failure.
Accompanies some urological diseases complicated by impaired renal function:
- polycystic disease;
- chronic pyelonephritis;
- distal tubular acidosis;
- hydronephrosis;
- benign prostatic hyperplasia in men.
Extrarenal - caused by a violation of general blood circulation, neuroendocrine regulation of urine formation, and a disorder of the urinary tract functions.
Water homeostasis is regulated by a complex mechanism of balance between water intake (which itself is also complexly regulated), renal perfusion, glomerular filtration, and reabsorption of soluble electrolytes in the tubules and water in the renal collecting system.
When water intake increases, circulating blood volume increases, which increases renal perfusion and GFR and leads to an increase in urine volume. However, increasing water intake decreases blood osmolality, which decreases the secretion of ADH (also known as arginine vasopressin) from the hypothalamic-pituitary axis.
Because ADH stimulates the reabsorption of water in the collecting ducts of the kidneys, decreasing ADH levels increases urine volume, which allows the body's water balance to return to normal.
In addition, high concentrations of soluble electrolytes in the renal tubules cause passive osmotic diuresis and thus an increase in urine output. A classic example of this process is glucose-induced osmotic diuresis in uncompensated diabetes mellitus, when high concentrations of glucose in the urine (more than 250 mg/dL) exceed tubular reabsorption capacity, resulting in high glucose concentrations in the renal tubules; water enters their lumen passively, causing polyuria and glucosuria.
Classification of the syndrome
According to the nature of polyuria, it can be:
- temporary – caused by an inflammatory process in the body or pregnancy;
- constant - a consequence of pathologies associated with impaired renal function.
Learn about the symptoms of bladder prolapse in women and the treatment of the disease. Instructions for using the dietary supplement Monurel PreviCyst are described on this page.
Polyuria is most often divided into:
- temporary – for example, after a hypertensive crisis;
- permanent - formed in diseases of the kidneys and endocrine glands.
There are several types of increased diuresis. Aqueous - urine of low concentration is released (hypoosmolar), this is due to a lack of antidiuretic hormone, decreased permeability of the tubules and collecting ducts, the ratio of dissolved substances in the urine to their content in the blood plasma is less than one.
In healthy people it is possible:
- when drinking a significant amount of liquid;
- transition from active life to strict bed rest.
Polyuria with low concentration in urine is determined by:
- during hypertensive crisis;
- after an attack of paroxysmal tachycardia;
- in the terminal phase of renal failure;
- during the treatment of heart failure when edema resolves;
- renal diabetes insipidus;
- hypokalemia;
- chronic alcoholism;
- polydipsia after encephalitis, mental trauma.
Osmotic - a lot of urine is released due to the simultaneous large loss of active substances (endogenous - glucose, urea, bicarbonate salts, and exogenous - mannitol, sugar). A significant accumulation of these compounds disrupts the ability of the tubules to reabsorb, they begin to leak water into the final urine. As a result, a large volume of liquid with a high concentration of active substances is released.
When does polyuria occur in children?
Polyuria is rare in children. Babies' kidneys are not able to filter large amounts of fluid. Therefore, children are very sensitive to both flooding and dehydration.
The maximum values of diuresis in children are shown in the table
| Child's age | Max diuresis in ml |
| 3 months | 600 |
| 6 months | 700 |
| 9 months | 750 |
| 1 year | 820 |
| 5 years | 900 |
| 14 years | 1400 |
| 18 years | 1500 |
In young children, the causes of the pathological condition should be distinguished from the habit of attracting attention to oneself by going to the toilet, or uncontrolled drinking.
| Child's age | Max diuresis in ml |
| 3 months | 600 |
| 6 months | 700 |
| 9 months | 750 |
| 1 year | 820 |
| 5 years | 900 |
| 14 years | 1400 |
| 18 years | 1500 |
How to improve kidney hemodynamics?
As a result of complications of kidney function, toxins accumulate in the body, which is the basis for deterioration in well-being. Poor nutrition, insufficient drinking, and medications negatively affect kidney function. The use of medications and herbal medicine improves blood circulation and restores organ functions.
Before using a drug that improves blood flow, it is necessary to find out the cause of the underlying disease, and at the same time restore the blood supply to the organ. If you are required to consult a doctor, a treatment regimen is drawn up:
- vascular medications (“Rovatinex”, “Trental”);
- antioxidants and membrane stabilizers (B vitamins, vitamin D, Mexidol, Berlition, Cytoflavin);
- special dietary food;
- cleansing procedures for the intestines.
Folk remedies will help improve kidney function:
- Lingonberry decoction. 2 tbsp. l. lingonberry leaves for 2 tbsp. water, cook for 15 minutes, take 100 ml of broth 4 times a day before meals.
- Licorice herb. 2 tbsp. l. pour 300 ml of boiling water, let it brew and take throughout the day.
- Celery, parsley. It is useful to drink juice and add to salads.
- Ginger. Tea with ginger throughout the day.
Herbal therapy should continue for at least a year. A course of 1 to 3 weeks is allotted for taking one drug, then it needs to be changed. After 2 -2.5 months a break is taken. To control the situation, it is necessary to do a urine test and be sure to consult a doctor on the amount of daily fluid intake.
How is vascular duplex performed?
Preparation
No special preparation is required to conduct the study, however, in order to increase its effectiveness, it is important to reduce the risk of developing increased gas formation in the intestines.
To obtain a high-quality ultrasound image, doctors advise:
- 2-3 days before going to the clinic, exclude foods that provoke flatulence - raw vegetables, fruits, legumes, sauerkraut, fresh baked goods, brown bread, sweets, milk;
- give up alcohol and carbonated drinks for the same period;
- have a light dinner the day before, and do the test in the morning on an empty stomach;
- if you are prone to increased gas formation, take enterosorbents (Polysorb, Smecta, activated carbon).
If the abdomen is bloated, the information content of ultrasound will be low
In emergency cases, it is possible to perform an ultrasound without prior preparation.
Progress of the procedure
Duplex scanning is performed by a qualified sonologist. The procedure is no different from a regular ultrasound.
After applying a special gel to the skin, the doctor runs an ultrasound probe over it (from the back, abdomen, and also on the right or left side). For better visualization, the doctor can examine the renal arteries with the patient standing.
It is most convenient to examine blood flow with the patient lying on his side
Duplex scanning does not cause any discomfort or discomfort. Sounds that may accompany the advancement of the sensor indicate blood flow indicators.
Calm ones indicate that blood moves freely through the vessel, and sharp ones indicate the presence of some kind of anatomical obstacle. On average, the entire procedure takes 25-30 minutes, and its price is 1000-2000 rubles. (together with ultrasound of the kidneys).
Interpretation of results
After the examination, the patient is given a medical report, which he must pass on to his attending physician. The specialist compares the obtained indicators with generally accepted standards and makes a clinical diagnosis.
Table: Normal ultrasound parameters of the renal arteries:
| Renal arteries | Diameter, mm | Diastolic/systolic blood flow velocity, cm/sec |
| Main trunk | 4,5 | 80/38 |
| Segmental | 2,2 | 50/25 |
| Interlobar | 1,5 | 35/18 |
| Arc | 1,1 | 26/12 |
Blood supply to the kidney
Based on the results of duplex scanning, the doctor receives qualitative and quantitative information about blood flow. He can assess the presence or absence of hemodynamic disorders, as well as determine the degree of their severity.
Note! In addition to blood flow indicators during an ultrasound, the doctor also evaluates the kidneys themselves. The contours of the urinary organs must be smooth, the anatomical structure must correspond to the norm. The parenchyma of healthy kidneys has a homogeneous structure and moderate echo density.
Pyelonephritis: causes, symptoms, diagnosis and treatment
Pyelonephritis is an inflammation of the urinary system, which can occur in acute and chronic forms. According to statistics, about 2/3 of urological patients suffer from pyelonephritis.
Its danger is that the symptoms of the disease are often not expressed - it can be mistaken for cystitis, a cold, radiculitis and even gastritis. Pyelonephritis may not appear for years, but if it is not detected in time, it becomes chronic.
Chronic pyelonephritis, the treatment of which is longer and more labor-intensive, can lead to serious complications. These include:
- Kidney failure
- Purulent kidney diseases
- Sepsis
Causes of pyelonephritis
The main cause of pyelonephritis is infection. The bacteria that cause it include:
- E. coli
- Proteus
- Staphylococcus
Very rarely, pyelonephritis is caused by a single bacterium. As a rule, several pathogens are detected in patients at once. Bacteria that enter the urinary system do not always cause illness. It can develop against the background of the following factors:
- Irregular urine flow
- Insufficient blood supply to the kidneys
- Reduced immunity
- Lack of personal hygiene
Bacteria that enter the bladder travel to the kidney, where pyelonephritis develops over time. It can be either an independent disease or a complication of existing pathologies, such as:
- Urolithiasis disease
- Prostate adenoma
- Diseases of the female genital organs
- Tumor in the genitourinary system
- Diabetes
A person can get pyelonephritis at any age.
At risk:
- Children under seven years old due to anatomical features of development
- Men over 55 years of age with prostate adenoma
Pyelonephritis also often develops in young women (symptoms and treatment are different from those in men). Through their short and wide urethra, microbes can easily penetrate the bladder, and from there into the kidneys, causing inflammation.
Symptoms of pyelonephritis
Symptoms of the disease depend on the form of the disease. Pyelonephritis in the acute stage manifests itself:
- High temperature
- Nausea and vomiting
- Frequent urge to urinate
- Sweating
- Thirsty
- Dull pain in the lower back
Sometimes the disease is preceded by acute cystitis, accompanied by frequent and painful urination, pain in the bladder area, and the appearance of blood in the urine.
If you notice any of the following symptoms, you should immediately consult a doctor.
. If therapy is not started on time, pyelonephritis can become chronic, and it will be very difficult to cure.
The symptoms of chronic pyelonephritis are not so pronounced, which is why the disease is often mistaken for a common cold, as it is often accompanied by the following manifestations:
- Fever
- Muscle weakness
- Headache
In addition to these symptoms, there may be the following:
- Frequent urination
- Strong, unpleasant odor of urine
- Aching pain in the lower back
- Dry mouth
- Belching
- Edema
- Pale skin
These symptoms are not constant and often the patient does not pay attention to them. This can continue for several years, and meanwhile, the inflammation will gradually spread to the kidneys and nearby tissues. The main differences between chronic and acute pyelonephritis:
- In chronic pyelonephritis, both kidneys are affected by the disease, while in the acute stage the disease makes itself felt only on one side
- Chronic pyelonephritis has stages of remission and exacerbation, during which the symptoms manifest themselves as clearly as in acute
Complications of pyelonephritis
If, during the acute stage of pyelonephritis, complete recovery does not occur within three months, the disease becomes chronic. Pyelonephritis in an advanced stage can cause the following complications:
- Kidney failure
- Paranephritis
- Sepsis
- Kidney carbuncle
Pyelonephritis, which has not been treated, enters the terminal stage: the diseased kidney is completely filled with pus and tissue decay products - pyonephrosis occurs. In this case, the kidney will need to be removed.
If the surgical intervention is performed correctly and the patient complies with all the doctor’s instructions, the prognosis is favorable. This disease is more common in patients over 40 years of age. It practically never occurs in children.
Treatment of pyelonephritis
Treatment of pyelonephritis is carried out comprehensively. Therapy will include medications and physiotherapeutic methods. Only this approach ensures the effect and contributes to the patient’s speedy recovery.
In acute pyelonephritis, antibiotics are prescribed to quickly eliminate the inflammatory process in the kidney.
Frequently changing medications is one of the basic principles of successful treatment, since bacteria very quickly become resistant to one or another antibiotic. In addition to antibiotics, the doctor may prescribe immunomodulators to increase the body's resistance to infection and prevent the disease from becoming chronic. Multivitamins are also used to boost immunity.
Treatment of chronic pyelonephritis is not much different from treatment of the acute stage of the disease, but it is much longer and more difficult. The following main activities are envisaged:
- Elimination of causes that cause difficulty in the outflow of urine or poor circulation in the kidney
- Drug therapy
- Increasing the body's immunity
The goal of therapy is to achieve stable remission. Sometimes this may take a year. The initial continuous course of antibiotics lasts 6-8 weeks. This is exactly how long it takes to suppress the inflammatory process in the kidney and prevent complications. The following signs indicate the success of therapy:
- Urine flow is normalized
- Blood and urine tests return to normal
- Body temperature remains stable at 36.6
- Swelling disappears
- Blood pressure stabilizes
If treatment goals have not been achieved and the patient's condition has not changed or has become worse, surgical intervention is required. As a rule, surgery is performed when purulent pyelonephritis or an abscess is detected. Depending on the severity of the disease, the following types of surgical intervention are prescribed:
- Removal of prostate adenoma
- Removing stones from the kidneys and urinary tract
- Nephrectomy (surgery to remove a kidney)
- Plastic surgery of the urethra, etc.
Due to the anatomical features of the urinary system, the infection enters the body differently in women and men. Therapy also varies and has the following features.
Treatment of pyelonephritis in women
Therapy is aimed at restoring the outflow of urine and destroying the source of inflammation. To do this, the doctor prescribes:
- Antibiotics
- Antibacterial agents
- Uroseptics
The course of treatment also includes a diet high in light carbohydrates and fermented milk products, and drinking plenty of fluids is recommended. The course of therapy for acute pyelonephritis is designed for 10-14 days. In the chronic form of the disease, stable remission can be achieved within 6 weeks to a year.
Treatment of pyelonephritis in men
To prevent the spread of infection, a course of antibiotics is prescribed - orally, infusionally or intravenously.
In addition to antibiotics, antispasmodics may be prescribed. If necessary, catheterization of the bladder is performed (in a hospital setting). After exiting the acute phase of the disease, the following are prescribed:
- B vitamins and ascorbic acid
- Antioxidants – selenium, tocopherol
- Diuretics
In exceptional situations, surgical intervention is resorted to. For pyelonephritis, the following operations are performed:
- Kidney decapsulation - removal of the fibrous capsule of the kidney
- Pyelostomy - creation of a fistula on the renal pelvis for the outflow of urine
- Nephropyelostomy – drainage of the renal pelvis through kidney tissue
- Nephrectomy – removal of the kidney (performed for extensive purulent lesions)
Along with the listed types of treatment, the patient is prescribed a special diet, the purpose of which is to strengthen the immune system and minimize the load on the urinary system.
If within a year after remission there was a relapse at least once, the patient’s dispensary registration is extended to three years and regular monitoring of tests is prescribed.