Adrenalectomy is the only radical surgical method for treating many pathologies of the adrenal glands. These glands perform an important hormonal role in the body, regulating complex processes of the reproductive, cardiovascular system and metabolic processes. Clinical manifestations depend on which hormone is produced to a greater extent by the adrenal glands.
Indications
There are some pathologies that require adrenal surgery:
- adrenal cancer (cortical cancer);
- serious dysfunction of organs;
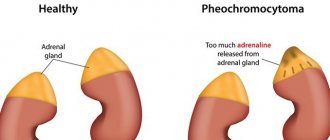
- pheochromocytoma (tumor of the brain);
- Cushing's syndrome (hypercortisolism);
- aldosteroma (tumor with the production of aldosterone);
- carcinoma or adenoma;
- increased mass of the adrenal glands.
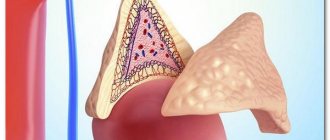
If the disease is benign or inactive, a partial adrenalectomy is performed. In this case, the specialist removes only pathological tissue without including the adrenal glands. The isolated material is subjected to laboratory histological examination. This allows us to identify the type and cause of the tumor.
Organ-sparing adrenalectomy is very important if the patient is diagnosed with damage to both adrenal glands. It gives a chance to reduce the lifelong use of hormonal drugs in order to regulate metabolic processes in the body.
Diagnostics
With a clinically active form of the disease, thanks to the characteristic symptoms, an experienced doctor is able to suspect a hormone-producing tumor of the adrenal gland even during a visual examination and questioning. To confirm the diagnosis, the patient is still recommended to undergo:
- for consultation with an endocrinologist and surgeon
; - laboratory study of hormonal profile . An analysis of hormones in the blood and urine allows you to evaluate the functioning of the adrenal glands, determine the level of hormones, and also specify the hormone produced by the tumor. A hormonal profile test involves taking blood in the morning on an empty stomach. To obtain reliable results, the patient is advised to avoid physical activity and stress the day before and on the day of the test.
- 24-hour urine analysis , the results of which can determine the type of adenoma.
- computed tomography with intravenous contrast . When carried out, it is possible to obtain three-dimensional images, based on which it is easier to determine the structure of the tumor, its size and density, and most importantly, to determine the likelihood that the tumor is malignant.
A biopsy of an adrenal adenoma is performed extremely rarely due to its low diagnostic significance and high potential morbidity.
Surgery to remove the adrenal gland
There are several types of adrenalectomy. Usually, the doctor decides the advantage of a certain method for each patient, taking into account the damage to the glands and the type of disease:
- Traditional method
In this case, the adrenal glands are removed through a cavity incision. The indication for a complex operation with an increased risk of bleeding is performed only for large tumors reaching 10-12 cm. It can be resorted to in urgent (urgent) situations when the patient’s condition is aggravated by symptoms and there is no time for a comprehensive examination. To do this, a radical incision is made, which helps to assess the general condition of the kidneys and identify possible metastases.
For formations of impressive size, a wide incision is made in the abdomen. This makes it easier to access and manipulate the tumor. After surgery, a large suture of at least 20 cm is placed, and drainage may be required.
- Laparoscopy
Thanks to modern equipment, surgery on the adrenal glands can be less traumatic for the patient. There are several types of laparoscopic access:
- From the back. Incisions are made in the lower back, and the patient assumes a prone position.
- Transabdominal. Access to the adrenal glands is through the anterior wall of the abdominal cavity.
- Lateral transabdominal. The patient is placed on the operating table on his side, where the healthy adrenal gland is located).
The laparoscopic method has become widely practiced in urological surgery. It requires minimal access to the glands. The only significant drawback is the increase in surgical intervention time. It goes like this:
- The doctor removes the affected organs or diseased tissue through several small incisions not exceeding 1.5 cm in diameter.
- Monitoring of the activities inside is carried out through endoscopic equipment with the image transmitted to the screen.
- The operation in this way is effective and safe, the possibility of injury to other organs is practically excluded.
- Through one of the incisions, gas is supplied into the abdominal cavity through a tube, forming an operating space.
- Standard instruments for surgery are inserted into the trocars (tubes): a clamp, a coagulator, a video camera and scissors.
- After surgery, a barely noticeable scar remains on the lower back.
- Bilateral adrenalectomy
If it is necessary to remove two adrenal glands at once, the patient is placed on his stomach or back. During the operation, the doctor makes sequential movements, influencing the glands one by one. Sometimes bilateral intervention requires complete removal of both adrenal glands or preservation of one, if indicated.
Material and methods
On the basis of the Department of Laparoscopic Surgery and Cholelithiasis of the Institute of Surgery and Transplantology named after. A.A. Shalimov and the surgical department of the Institute of Endocrinology and Metabolism named after. V.P. Komissarenko performed 32 laparoscopic resections of the adrenal glands (adenoadrenalectomies) during the period 2002–2013. Surgical interventions were performed using endoscopic equipment from Richard Wolf (Germany), Medpharmservice (Russia), Karl Storz (Germany), Olympus (Japan), Viking (USA). To achieve hemostasis, we used the Patonmed EKVZ300 generator (Ukraine) and bipolar endoscopic electric welding instruments developed at the Institute of Electric Welding named after. E.O. Paton.
All surgical interventions were performed as planned, after adequate instrumental and laboratory examination of patients.
All patients had benign neoplasms, confirmed preoperatively using multislice computed tomography with intravenous contrast enhancement. Statistical data on the diagnoses and tumor sizes are presented in Table 1. The schematic location of the tumors and the lines of adrenal resection are shown in Figure 1.
The method of pain relief in all cases was endotracheal anesthesia. The Gagner lateral transabdominal approach was used in all cases of unilateral adrenal gland lesions (22 cases) and the anterior transabdominal approach in bilateral adrenal gland lesions (5 cases). Mobilization of the tumor and the adjacent part of the adrenal tissue began from the side in which the tumor was located. The vessels on the side of the healthy part of the adrenal gland were not ligated in order to preserve the blood supply to the remaining tissue. Resection of the adrenal gland was performed using high-frequency electric welding technology. Consecutive electric welding resection allows obtaining an optimal resection line, depending on the shape of the tumor, and preserving a sufficient amount of adrenal tissue, while simultaneously ensuring reliable hemostasis. Ligation of the central vein of the adrenal gland was performed only in cases where it was located in the area of tumor resection. Neoplasms with adjacent adrenal tissue were removed and sent for pathohistological examination.
Price
The price of laparoscopic surgery to remove endocrine glands includes not only the intervention. If the patient does not have the opportunity to receive a quota provided by the state for free medical care, adrenalectomy will not be cheap.
According to the latest reports, the cost of the operation varies from 80,000 rubles. Such prices are due to the complex preparation of the patient for treatment, as well as the use of expensive high-tech equipment.
Forecast
If the tumor is detected and removed in a timely manner, the prognosis for life and subsequent work is considered favorable.
After removal of androstenoma, the patient may remain short in stature. After surgery for pheochomocytoma, residual effects are sometimes observed in the form of rapid heartbeat, transient or persistent hypertension, which is reduced with antihypertensive therapy.
After eliminating aldosteroma, almost 70% of patients recover. 1.5-2 months after removal of a benign caticosteroma, the symptoms disappear, the general condition of the patient improves significantly and the appearance changes.
In the presence of a cancerous tumor and the presence of metastases, the prognosis is unfavorable.
loading…
Consequences for the body
From adrenalectomy, the patient remains at risk of complications regarding the functionality of the body due to access to the adrenal glands and their direct removal. After laparoscopic treatment, the patient observes short-term bed rest (from 24 to 48 hours).
Early complications:
- phlebothrombosis;
- intestinal paresis;
- pleurisy;
- pneumonia and pneumothorax;
- infectious purulent lesion.
There are also later complications when the entire load is directed to the remaining gland during unilateral adrenalectomy. The patient exhibits adrenal insufficiency. It includes hypoglycemia (lack of calcium), hypotension (low blood pressure), confusion and weakness.
With bilateral surgery, the body will not be able to fully function without hormonal replacement treatment.
Results and discussion
The average duration of unilateral laparoscopic adrenal resection was 57.7 ± ± 5.2 minutes; bilateral - 124.1 ± 13.4 min. The average volume of intraoperative blood loss during unilateral surgery was 39.8 ± 4.3 ml; with bilateral - 77.6 ± 8.2 ml. Ligation of tumor vessels, resection of the adrenal gland and final hemostasis were carried out using electric welding technology in the “coagulation” and “automatic welding” modes. Due to the anatomical features of the right central adrenal vein, which is often short and wide and directly drains into the inferior vena cava, it is safer to use hemostatic clips for its ligation. During right-sided resection of the adrenal gland, when ligation of the central vein was necessary (6 cases), clips were applied in 4 (66.7%) cases; in 2 (43.3%) cases, the length of the right central vein allowed electroligation using welding technology. No bleeding was observed from the sealed vessels or resected adrenal tissue. In hormonally active tumors, elevated levels of aldosterone, cortisol, or metanephrines dropped to normal values during the first to fourth days after surgery. Manifestations of arterial hypertension and steroid-induced diabetes mellitus decreased from the first day after surgery to 10 months after surgery. There were no cases of adrenal insufficiency or relapse of the disease.
We performed 32 laparoscopic adrenal resections in 27 patients. We believe that laparoscopic adrenal resection is indicated in the presence of a benign solitary adrenal mass. Laparoscopic adrenal resection is especially important if there are tumors of the adrenal glands on both sides, or if one of the adrenal glands has been previously removed. Bilateral pheochromocytomas are relatively common in MEN type II syndromes. In such cases, this type of surgical intervention prevents the need for lifelong corticosteroid replacement therapy, reduces the risk of developing acute or chronic adrenal insufficiency, which significantly improves the quality of life of patients [9, 10].
Among the contraindications to laparoscopic resection of the adrenal glands: 1) signs of malignancy of the formation; 2) multicentricity of damage to one adrenal gland; 3) atrophy of the adrenal cortex in adenoma with aggressive hormonal overproduction. If there are preoperative signs of malignant growth of an adrenal tumor, open adrenalectomy is indicated. If suspicion of tumor malignancy is established during laparoscopic intervention, conversion to open adrenalectomy is indicated [11, 12]. In cases of benign adrenal tumors, there are also limitations to the laparoscopic resection method. An important condition is to exclude multicentric growth of the formation to prevent the risk of relapse of the disease. If 2 or more formations (even small ones) are detected in one adrenal gland, open or laparoscopic adrenalectomy is indicated. With an adenoma of the adrenal cortex with aggressive hormonal overproduction, when the rest of the adrenal tissue is hypotrophic and thinned, it is technically very difficult to leave a clinically significant amount of tissue and maintain sufficient blood supply for it. In such cases, open or laparoscopic adrenalectomy is indicated.
In terms of the duration of surgery, the volume of intraoperative blood loss, the duration of postoperative hospitalization, the risk of complications and relapses, the results of laparoscopic adrenal resection are comparable to the results of laparoscopic adrenalectomy (Table 2).
After removal of the adrenal glands
The patient will need to change his lifestyle somewhat. Even following the recommendations of a specialist, no one is immune from a deterioration in the quality of life. If symptoms in the kidneys or other organs occur within 3 months after adrenalectomy, it is recommended to consult a doctor for advice. The patient must also:
- Follow a special diet. The diet should be balanced and include a large amount of protein and offal. It is recommended to include vitamins according to the daily requirement. All dishes are prepared gently - baked or steamed. Food is taken in fractional portions.
- After removal of the hormonal glands, it is necessary to minimize stressful situations in which the maximum production of certain hormones occurs. It is important for the patient to undergo an annual examination in the hospital. This will allow you to monitor his condition and detect complications at an early stage.
The adrenal glands and the hormones they produce are vital to the body. If you do not take special medications, lead an unhealthy lifestyle and ignore the symptoms, this can cause death.
Why laparoscopic adrenalectomy?
The use of laparoscopic equipment causes minimal harm to the patient’s body, giving him the opportunity to quickly recover after surgery and return to his usual rhythm of life.
Typically, patients are discharged from the hospital 1-2 days after surgery.
Advantages:
- less pain after surgery;
- short hospital stay;
- rapid postoperative recovery;
- better cosmetic effect;
- less risk of postoperative hernias and suppuration of postoperative wounds.
Adrenalectomy during pregnancy
When pregnancy is combined with chronic adrenal insufficiency, a great threat to a woman’s life remains. It is not recommended to plan to carry a baby with tumor pathology before surgery. Deterioration of the condition is observed from the early stages and persists throughout the entire period and after childbirth. If the type of tumor allows you to delay planned surgery, special therapy is developed for the patient. You should also consider:
- Pregnancy is planned no earlier than a year after adrenalectomy and full compensation of glandular insufficiency.
- A woman must constantly take certain doses of hormonal drugs.
- Prolonged pregnancy is impossible if exacerbations, complications occur, or therapy is not effective.
- After a previous operation, the expectant mother is under constant monitoring by the leading doctor and endocrinologist.
Adrenalectomy is the only adequate treatment of the adrenal glands for tumor pathology and the development of insufficiency. You can also find out the surgeon’s opinion by watching this video about removing an adrenal tumor for abdominal adhesive disease.
Rehabilitation
After surgery, the patient is placed in a room with special equipment that allows monitoring all the basic vital functions of his body. If an open approach was used, the patient can be discharged after a week, and in the case of a laparoscopic technique, the rehabilitation period is reduced to several days.
The most important thing is to determine the hormonal state of a person. For this purpose, various techniques are used, including laboratory tests. The pressure and degree of likelihood of infectious infection are carefully monitored and controlled. If both adrenal glands are removed, hormone replacement therapy is immediately recommended. In case of surgery on one organ, such treatment is most often not required.
Laparoscopy
The laparoscopy method is not as traumatic as abdominal surgery and has fewer negative consequences. Only 4 small incisions are made on the patient’s body, through which special equipment is introduced into the body. All manipulations are controlled by a physician through a monitor. The operation is quite lengthy, but effective.
Transabdominal laparoscopy involves the introduction of endosurgical instruments through punctures in the abdominal cavity. The patient lies on his back or side. Medicine does not stand still, and recently many new surgical techniques for performing adrenectomy have appeared. In modern clinics, surgery can be performed by a surgical robot, without the participation of a physician. Such a machine has steel “arms” for carrying out various manipulations. A person controls the robot from a special console.
Indications and contraindications for surgery
This operation is carried out in strict accordance with the indications. Because there is always a risk to the patient's health.
Indications for surgical intervention include:
- Cortical malignant tumor.
- Cushing's syndrome.
- Hormone-active tumors such as pheochromocytoma, aldosteroma, adenoma.
- Significant increase in organ size.
- Adrenal dysfunction with unknown cause.
Contraindications to the operation include:
- Patient's comatose state.
- Decompensation of cardiac activity.
- Septic infection.
- The presence of diffuse purulent inflammation of the peritoneum.
- Decreased activity of the blood coagulation system.
- Late pregnancy.
- Adhesive disease.
- Infectious processes in the abdominal wall (anterior).
Having compared all the pros and cons regarding the operation, the doctor and the patient or his relatives decide on the rationality of the operation.